1. Background
In critical care unit, some factors and patient’s condition can alter verbal communication and make pain assessment difficult, including endotracheal intubation, reduced level of consciousness, sedation and administration of paralysing drugs (1, 2). After cardiac surgery, tracheal intubated patients in ICU without verbal communication, usually experience painful care after certain treatments (3) since they cannot express their pain verbally, in writing, pointing with fingers or shaking their heads (4). Nursing staff are usually unaware of their pain and it is likely that pain remains untreated (5). Low level of consciousness and being on ventilator or receiving tranquilizers are some samples of this condition (6). Untreated and prolonged pain can affect endocrine, cardiovascular, immune, nervous and musculoskeletal systems and result in chronic pain syndrome, prolonged hospitalization (7) and increased catecholamine and stress hormones release, which in turn would cause increased blood pressure, increased heart rate and increased oxygen demand and decreased perfusion (8). Heart surgery patients experience extreme pain due to the nature of operation, chest tubes and sternal incision. In fact, stress responses and imbalance between demand and supply for oxygen in myocardium could lead to myocardial ischemia or infarction and may increase mortality rate (9).
Nurses play a vital role in pain assessment (10) and determine pain intensity and perform medical and non-medical treatment for these patients. Therefore, it is necessary for nurses to be fully aware of a standard and systematic pain evaluation protocol (11). In response to these needs, methods were offered to evaluate pain in patients more effectively. Some of such pain assessment tools include facial expression (FE), critical care observation tool (CPOT), non-verbal pain scale (NVPS), faces, legs, activity, cry and consolability scale (FLACC), behavioral pain scale (BPS) and pain assessment in advanced dementia (PAIND) (8).
In 2006, American pain management nursing association recommended using the two tools, BSP and CPOT, for evaluating pain in tracheal intubated and unconscious patients (8, 12). As mentioned before, patients who have undergone open heart surgery would experience severe pain (13) and the only regular method in evaluating pain in these patients in studied hospital was facial expression and the only item studied in this method was patient’s face. On the other hand, CPOT is used for patients in ICU who have had open heart surgery (14) and is easily performed by caregivers (15).
2. Objectives
Therefore, the aim of this study was to evaluate convergence between these two tools for pain assessment and their consistency with hemodynamic changes due to pain in tracheal intubated patients after cardiac surgery.
3. Patients and Methods
This was a prospective study. After the research was approved by the institutional ethics committee, evaluating the diagnostic tests was started in a referral university cardiovascular, medical and research center. The study was conducted on patients who had undergone cardiac surgery and met the necessary criteria for the research and were studied until the target sample size (n = 100) was reached. Inclusion criteria were coronary artery bypass grafting surgery, replacing or repairing heart valve by sternotomy and lack of verbal communication due to tracheal intubation, lack of extreme facial damage, movement in at least one body part, patient’s age at least 18 and at least 3 hours after any administration of sedatives, analgesics and muscle relaxing agents. Exclusion criteria were opium addiction, receiving above mentioned drugs after surgery during the study, comatose patients, spinal cord damage and body limbs paralysis or weakness and patients with heart failure during the surgery who received high doses of inotropes and vasopressors.
3.1. Sampling Method and Size
In this study, the convenience sampling method was used. Patients who had undergone cardiac surgery in a referral university cardiovascular, medical and research center intensive care units, and met the inclusion criteria entered the study. With mathematical relations for KAPPA statistic calculation and general and accidental convergence difference of 0.2 and α type error = 0.5, and study power of 80%, sample size was calculated as 100. Nine people were excluded from study due to incorrect or inadequate data and 91 patients were statistically analyzed.
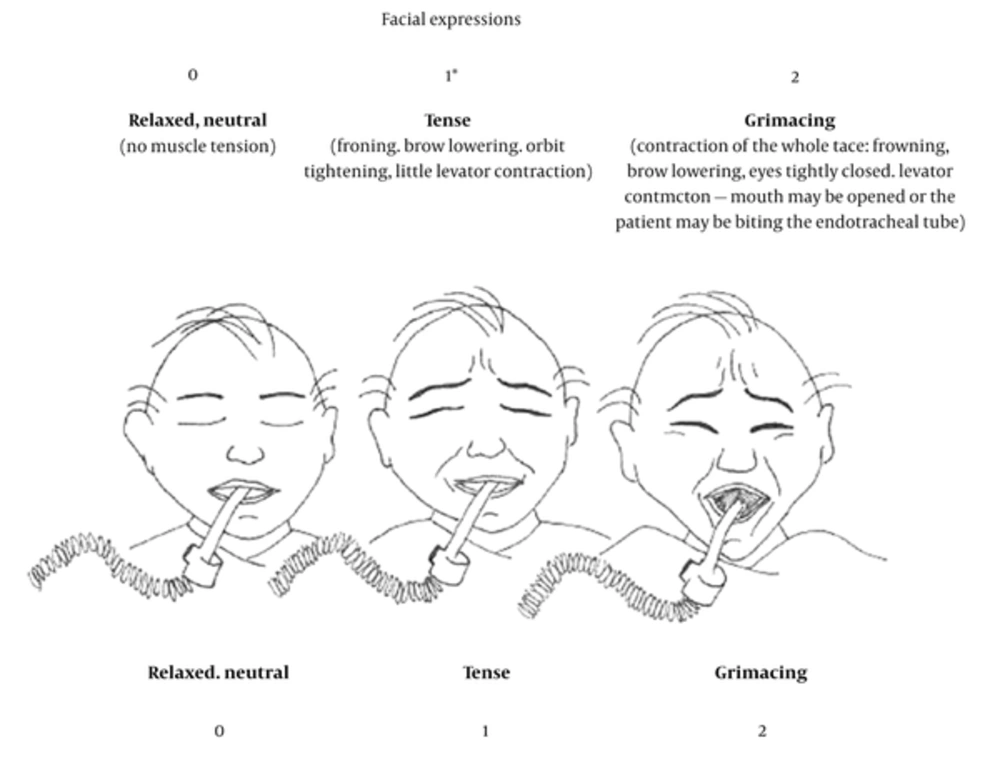
Data collection tool included demographic information including age, gender, history (diabetes and blood pressure), surgery type and consciousness level, history of drug abuse, sedation and analgesic drugs. Vital signs checklist included systolic and diastolic pressure, pulse and respiratory rate collected by the researcher and recorded by the monitoring device. The behavioral pain scale form for CPOT, which included 4 items of facial movement, body movement, muscle tune and acceptance of ventilator in intubated patients and sound making of non-intubated patients, had two points for each item, 8 points in total. Zero for no pain, and eight for the maximum amount of pain (Table 1). The Behavioral pain scale form for FE including only expressions of patient’s face (Figure 1) was completed by the colleague of the project to create blinding.
| Indicator | Score | ||
|---|---|---|---|
| 0 | 1 | 2 | |
| Facial description | No muscular tension observed: relaxed, neutral | Presence of frown brow lowering, orbit tightening, and levator contraction: tense | All of the above facial movements plus eyelid tightly closed: grimacing |
| Body movements | Does not move at all (does not necessarily mean absence of pain): absence of movements | Slow cautions movements, touching or rubbing the pain site, seeking attention through movements: protection | Pulling tube, attempting to sit up, moving limbs/thrashing, not following command, striking at staff, trying to climb out of bed: restlessness |
| Muscle tension (evaluation by passive flexion and extension of upper extremities) | No resistance to passive movements: relaxed | Resistance to passive movements: tense, rigid | Strong resistance to passive movements, inability to complete them: vary tense or rigid |
| Compliance with the ventilator (intubated patients), OR | Alarms not activated, easy ventilation: tolerating Ventilator or movement | Alarms stop Spontaneously: coughing but tolerating | Asynchrony: blocking ventilation, alarms frequently activated: fighting ventilator |
| Vocalization (extubated patients) | Talking in normal tone or no sound | Sighing, moaning | Crying out, sobbing |
a(16).
A score of 1 may be attributed when a change in the patient’s facial expression is observed compared with rest assessment (e.g. open eyes, weeping). The drawings were inspired from Prkachin’s study (17).
3.2. Data Collection
Anesthesia induction was performed by Midazolam 0.1 mg/kg, Fentanyl 5 - 10 μg/kg or Sufentanil 2.5 - 4 μg/kg, Cisatracurium 0.15 mg/kg and for maintenance of anesthesia we used Midazolam 1 µg/kg/min and Fentanyl 1 - 3 μg/kg/h or Sufentanil 0.5 - 1 μg/kg/h and Atracurium besilate 0.3 to 0.6 mg/kg/h. After completing the cardiac surgery, patients were admitted to ICU while intubated. The steps of pain assessment were: 1) between 3 - 4 hours after patients were admitted to ICU, the patient gradually emergence from anesthesia and while the patient was still intubated, the researcher would evaluate patient’s pain severity using CPOT tool and the research colleague nurse would do the same using facial expression tool, without knowing each other’ results (blinded) at Time Zero T0. 2). After the initial pain evaluation, the level of analgesia, BP, heart and respiratory rates and the level of oxygen saturation evaluated and recorded every 30 minutes for two hours (T1 = 30 minutes,T2 = 60 minutes, T3 = 90, T4 = 120 minutes). In total, all the units in the research were evaluated 10 times (5 times with CPOT and 5 times with FE).
3.3. Statistical Analysis
Analysis was performed using SPSS 21.0 for Windows statistical software (SPSS Inc. IBM Corp., Chicago, Illinois, USA). Compatibility of quantitative data distribution with normal distribution was evaluated using one-sample Kolmogorov-Smirnov test. To describe data, mean and standard deviation (SD) for continuous variables and numbers (percentage) for categorical variables were used. To evaluate quantitative variables in different time steps, in each group, “repeated measures analysis of variance (ANOVA)” Statistical model was used. Comparison between rating variables (for pain tools) was performed using “Wilcoxon sign-ranked test”. To evaluate pain intensity as time passed, Friedman test was used. Convergence between the pain tools was evaluated using weighted kappa with 95% certainty range. P value equal to or less than 5% was considered as statistically significant.
4. Results
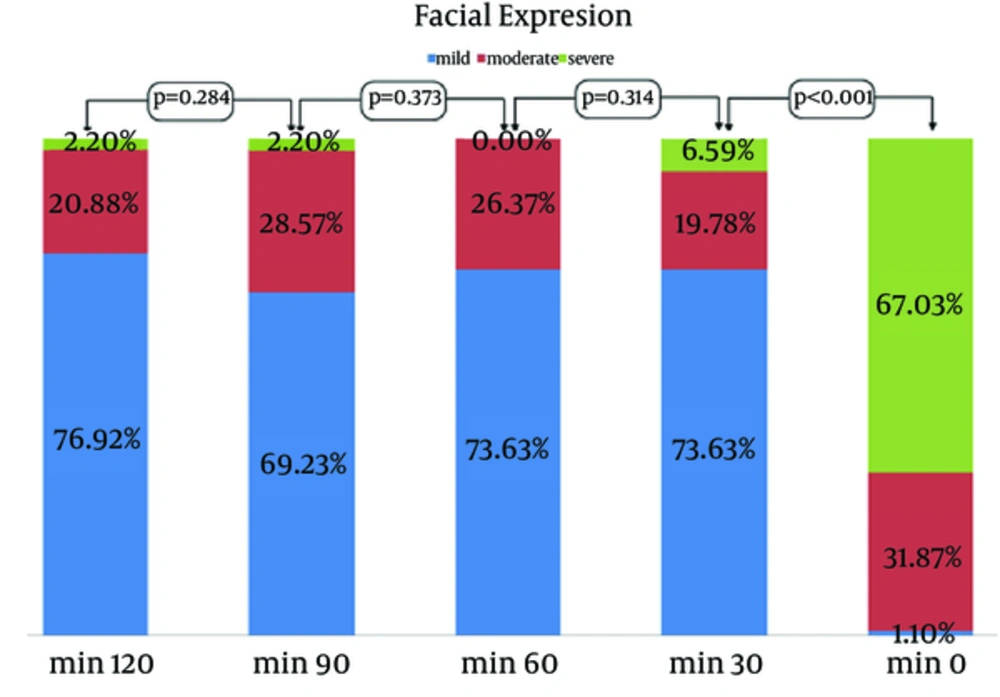
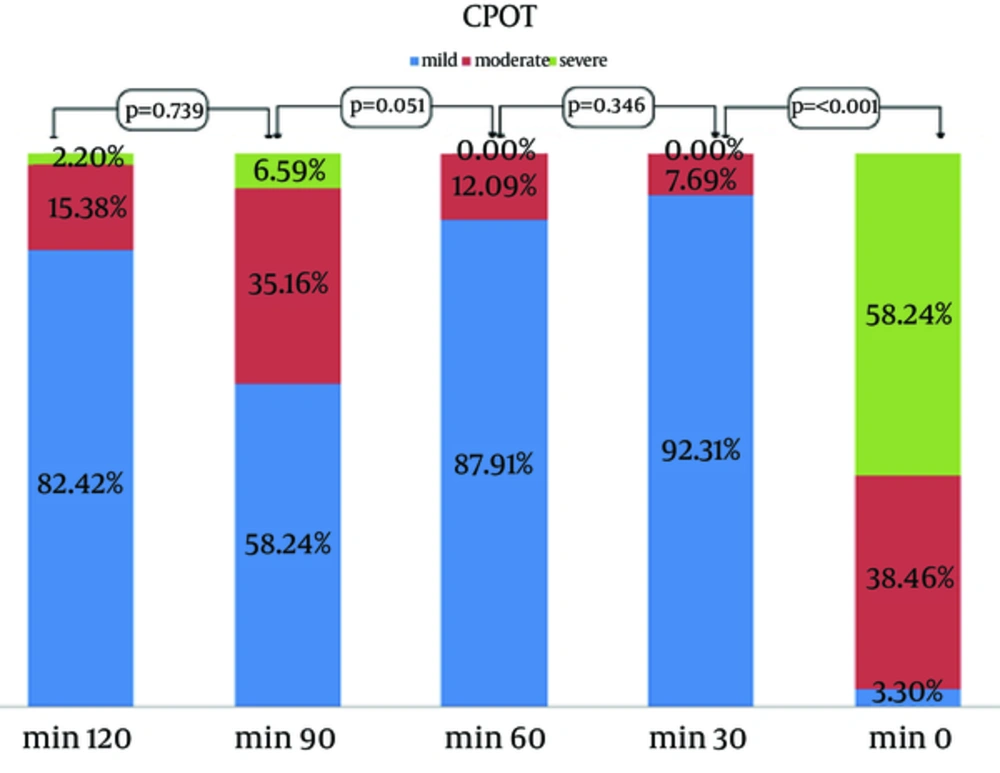
Data was collected from 91 intubated patients in ICU following cardiac surgery. Demographic data of patients are presented (Table 2). Sixty three patients were male (69.2%) and the mean age was 56 years. Hypertension and diabetes mellitus were reported as 28.5% and 24.1%, respectively. Obtained pain evaluation pattern showed severe pain for over a half of patients at T0 after the effect of anesthetic drugs eliminated; 58.2% of patients based on CPOT behavioral tool and 67% based on FE behavioral tool. Then the pain decreased and in minutes 30 and 60, patients experienced almost no extreme pain. In minute 90, a number of patients experienced moderate pain and a smaller number experienced severe pain, which intensity decreased in minute 120. Statistically, the Friedman test was performed on each data from CPOT tool and FE resulted in P ˂ 0.001, which showed that changes in pain levels as time passed were significant (Figures 2 and 3).
| Variables | Values |
|---|---|
| Age (15 - 83), y | 14.8 ± 56 |
| Height (153 - 180), cm | 6.4 ± 167 |
| Weight (45 - 105), kg | 12.2 ± 70 |
| Gender | |
| Female | 28 (30.76) |
| Male | 63 (69.24) |
| Diabetes mellitus | 22 (24.1) |
| Hypertension | 26 (28.5) |
aData are presented as mean ± SD or No. (%).
When the patient was conscious, a high level of agreement was observed between the two tools in evaluating pain (κ = 0.787). However, the level of agreement was weak in T1 (κ = 0.249) and T2 (κ = 0.555), no agreement was observed in T3 (κ = 0.166), and in T4 (κ = 0.851) the agreement was high (Table 3). In fact, increase in pain intensity was clearly obvious in minute 90, compared to minutes 60 and 120 using CPOT. Whereas, the FE tool evaluated nearly similar pain severity during these times and showed no increase in the level of pain.
| TIME | Kappa | CI 95% |
|---|---|---|
| 0 | 0.787 | (0.675 - 0.919) |
| 30 | 0.249 | (0.082 - 0.477) |
| 60 | 0.555 | (0.354 - 0.755) |
| 90 | 0.166 | (0.0 - 0.295) |
| 120 | 0.851 | (0.696 - 0.974) |
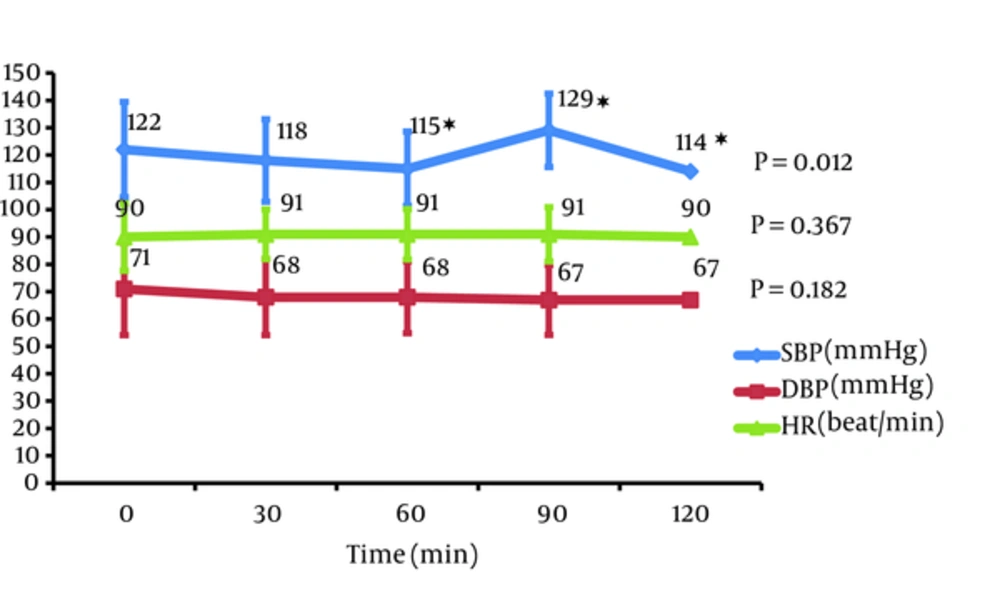
Regarding the correlation of physiologic parameters with level of pain intensity in patients, there was no statistical and clinical significant association between diastolic blood pressure changes and heart rate during the evaluation, and there was only a significant association between systolic blood pressure and the level of pain. Increase in pain intensity with increase of systolic blood pressure was detected and recorded by CPOT tool, whereas this correlation was not observed in FE (Figure 4).
5. Discussion
Many researches performed with an emphasis on the fact that pain control is not enough in ICU patients, and pain is not assessed adequately by caregivers. A number of researches performed to find out the best way to evaluate pain with physiologic and behavioral criteria in unconscious and tracheal intubated patients.
This study aimed to evaluate the use of two tools, CPOT and FE, and their agreement in detecting and evaluating pain levels in intubated patients in ICU, after cardiac surgery. In this research, intubated patients experienced different levels of pain and when their evaluated pain was in highest and lowest levels, the highest level of agreement observed between the two tools. Whereas, there was lack of strong agreement between the tools when there was moderate and low level pain, so that in T4, the change was reported in the pain by CPOT tool, but FE tool was unable to detect this change. This would suggest higher sensitivity of CPOT tool in assessing pain compared to FE.
In the study of Gelinas et al. on intubated patients, over a half of patients experienced pain while resting (18). The researcher here concluded that patients would experience pain during their time in ICU in situations such as low consciousness levels and when trachea was intubated.
Also in Gelinas’s study on intubated patients, most nurses expected body movement to detect patient pain and rarely used FE (19). Whereas, Arif-Rahu and Grap specified FE as one of the most widely used methods of pain detection due to its behavioral expression and feelings richness. However, he considered it as an incomplete tool, since patient’s lower half of face (mouth and lips) is covered by tapes used to fix tracheal tube and/or nasogastric tube; therefore, patient’s face is not exposed fully to evaluate expressions and muscle movements and recommends FACS (facial action coding system) to evaluate and detect pain using FE, also pain detection is not limited to patient’s grimace and patient’s face facial muscles retractions (20).
Moreover, as pain is an occurrence that would happen to the whole body and is not limited to one location (presented in chest, lower body parts, hands, and etc.) a pain assessment tool can evaluate whole body reaction, logically. On the other hand, some patients would grimace unaware when they are awake, and every such expression in awareness cannot be interpreted as pain. Thus, all the mentioned reasons and deficiencies for FE tool can cause underestimate and overestimate in results and cause inappropriate administration of analgesic medications for these patients, just like the first step (T0) in our study, where FE tool recorded higher level of pain compared to CPOT tool.
Of hemodynamic variables, systolic blood pressure was consistent with pain level changes before and after analgesic drugs were used, and increase in systolic blood pressure was consistent with reported pain increase by CPOT tool. Aurbor and Gelinas showed that physiologic indicators would increase with severe pain (21). Whereas, McCaffrey and Locsin (22) reported that physiologic indicators would be affected by environmental conditions such as physiologic and hemodynamic conditions and medications (analgesics, sedatives and tranquilizers), they are not constant indicators of proving pain and recommend physiologic indicators to detect pain. In this research, the agreement between CPOT and changes in physiologic changes because of pain, like systolic blood pressure, was more than FE, which could suggest that CPOT is more sensitive compared to FE.
Marmo and Fowler evaluated pain in intubated patients after cardiac surgery using three multi-criteria tools, FLACC, NVPS and CPOT, and specified CPOT as a more sensitive tool compared to the other two (8). Boitor et al. established validity of CPOT for evaluation of sensory and affective constituents of pain after cardiac surgery. They found that vital signs were not precise to assess pain and validated tools should be used for this purpose (23). Rijkenberg et al. reported that behavioral pain scale (BPS) and critical-care pain observation tool (CPOT) are useful pain evaluation instruments for un-communicative and sedated ICU patients. This study compared validation and consistency of CPOT and BPS in tracheal intubated patients (24).
Pain assessment has always been a challenge in patients hospitalized in ICU, who are unable to communicate adequately and express their pain due to numerous reasons (low level of consciousness, tracheal intubation, etc.). Since pain is a mental and complicated phenomenon usually felt throughout the body, CPOT tool is more sensitive due to having multiple items and evaluating different behavioral indicators for pain in intubated patients compared to FE tool with only one criterion. Moreover, CPOT is more consistent with physiologic changes due to pain in patients. The researcher suggests more studies to confirm the sensitivity of CPOT tool.
There were some limitations in our study, such as research units limited to a single center and only intubated patients undergoing cardiac surgery were studied; therefore, our findings are generalizable to these patients. Second, some behaviors such as stress were considered as pain by the evaluation tool and unpredictable changes in patients’ conditions (return to the operating room, administration of tranquilizers instead of analgesics, changing hemodynamics-hypotension or low cardiac output syndrome to make patient fully unawake) happened that resulted in the samples being less than what was originally intended.