1. Background
Laparoscopy was introduced in 1986 (1). This kind of laparoscopic surgery is currently proposed as a standard treatment for gallstone disease and it leads to less postoperative pain than open cholecystectomy (2, 3). Post laparoscopic shoulder pain (PLSP) is a common trouble after Laparoscopic surgeries (4).
Pain after LC has been classified to 3 major types. These include PLSP (referral pain can be localized in the right shoulder), visceral pain (biliary colic), and parietal pain (pain in the abdominal wall or surgical area) (5). Patients report PLSP resulting from diaphragmatic stimulation caused by insufflation of CO2 in the abdomen and its mixture with water and carbonic acid (5, 6) and the residual pneumoperitoneum after LC (7). Various pharmacological agents were chosen to control postoperative pain associated with pneumoperitoneum. All of them have already been well-documented in the literature, such as non-steroidal anti-inflammatory or COX II inhibitors, dexamethasone (90 minutes prior to induction), and pre-incisional use of bupivacaine (8). However, pain management after LC remains an unresolved issue (9).
To the best of our knowledge, randomized trials have demonstrated that clonidine, an Alpha 2 adrenoceptor agonist, could reduce postoperative pain (10), intra-operative, and postoperative narcotic requirement (11-14), and improves perioperative hemodynamic stability (14, 15) without significant side effects. Moreover, spinal anesthesia with adjuvants, such as low dose intrathecal clonidine, modify hemodynamic trends with significant reduction in PLSP (16). There has been relatively little literature published on the effect of clonidine in post-operative shoulder pain, none of them tried to investigate the effect of oral premedication of clonidine on PLSP after LC in patients under general anesthesia.
2. Objectives
This study aimed at evaluating the effect of oral clonidine on PLSP intensity, MABP and heart rate (during the 8th hour after operation) in patients, who had laparoscopic cholecystectomy indication.
3. Methods
This study was a double-blind randomized placebo-controlled clinical trial. The study was approved by the ethics committee of the Yazd University of Medical Sciences (ethics ID: IR.SSU.REC.1390.125789) and followed ethical considerations of the declaration of Helsinki (17). The study was registered at the Iranian registry of clinical trials (IRCT ID: IRCT2017071117468N4). A written informed consent was obtained from each patient and they could withdraw from the study any time.
The study population consisted of patients, who were candidates for LC, from March 25th to August 6th, 2017.
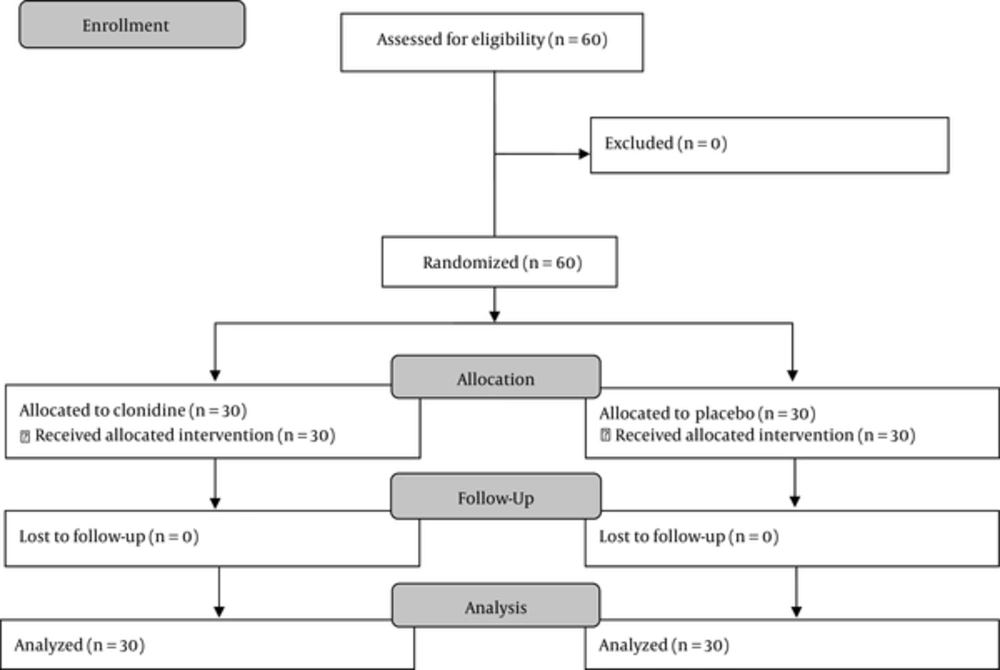
Sample size was (at least 30) calculated with confidence level of 95%, a power of 80%, and in accordance to a previous study (10). Then, 60 patients were randomly (simple random sampling method) selected and allocated to 2 equal groups of clonidine and placebo using the block randomization method. A double–blind technique was used, according to which the first research assistant (an anesthetist), who was responsible for the data collection, and all patients were blinded to the group allocations (conducted by the researcher).
The inclusion criteria were as follows: American society of anesthesiologists (ASA) grades I and II, male and female gender, adult patients aged 18 to 65 years, body mass index (BMI) > 35 kg/m2, schedule for elective LC surgery. Patients with history of bronchial asthma, diabetes, hypertension (essential or secondary), severe cardiovascular abnormalities (ischemic heart disease, valvular heart disease, and AV conduction blocks), concomitant use of monoamine oxidase inhibitors, tricyclic antidepressants or opioids, and allergy to clonidine were excluded. Also, lack of patient consent was considered as exclusion criteria.
In the clonidine group, patients received 0.2 mg oral clonidine (Clonidine HCL TAB, Toliddaru, Iran) 90 minutes before induction. In the placebo group, the patients received 100 mg of Vitamin C tablet at the same time with the clonidine group.
Premedication was performed by metoclopramide 0.1 mg/kg, midazolam 0.05 mg/kg, and fentanyl 1 μg/kg. General anaesthesia was induced by thiopentone 5 mg/kg and atracurium 0.5 mg/kg. Anesthesia was maintained with isoflurane and N2O (60%).
The position of the operating table was made revers Trendelenburg during peritoneal insufflation. After that, it was changed to revers Trendelenburg and left tilt about 15º. Intra-abdominal pressure was not allowed to exceed 15 mm Hg during the surgery.
Post-operative analgesia was conducted by meperidine 0.5 mg/kg IV in the recovery room. Moreover, the patients received (400 mg) orally ibuprofen in the ward whenever it needed to the additional painkillers.
The background and demographic questionnaire was designed with 8 items about variables, such as age, gender, job, education level, marriage status, height, weight, and ASA class. The VAS was used to measure PLSP intensity related to LC. According to Gallagher et al.’s study, this scale was valid and reliable (r = 0.99) for measuring acute pain (18). The scale consisted of a horizontal line VAS (0 to 100 mm); the left and right extremes demonstrated the lowest and highest levels of pain, respectively. Hemodynamics (MABP and heart rate) were recorded prior to induction (basal time). Also, VAS and hemodynamics were assessed in semi-sitting position at emergence from anesthesia, 4 and 8 hours after operation. A researcher made-checklist was used to record adverse effects, such as hypotension (blood pressure less than 25% of baseline or SBP less than 90 mmHg), bradycardia (heart rate less than 20% of baseline or absolute heart rate less than 40 beats per minute), nausea, and vomiting (yes/no).
Quantitative variables were shown as mean and standard deviation of mean, and qualitative variables were represented as number of frequency and their percentage. The researchers used Chi-square, Fisher’s exact, and independent samples t tests to assess homogeneity of the variables. Independent samples Students t-test was used for comparison between groups. To perform Statistical analysis, SPSS software version 18.0 was used.
4. Results
In this study, 60 patients were enrolled. No one was excluded during the course of assessment for eligibility and follow-up. Therefore, final analysis was done for all individuals (Figure 1). The mean age of individuals was 36.85 ± 10.93 years and the mean BMI was 26.34 ± 3.46 kg/m2. As shown in Table 1, the 2 groups of individuals were not comparable with respect to age, gender, marriage status, education level, job, ASA class, height, and weight (P ≥ 0.05) (Table 1).
| Variable | Group | P Value | ||
|---|---|---|---|---|
| Clonidine | Placebo | |||
| Age | 36.5 ± 11.1 | 37.1 ± 10.8 | 0.84b | |
| Gender | Male | 9 (30.0) | 5 (16.7) | 0.22c |
| Female | 21 (70.0) | 25 (83.3) | ||
| Marriage status | Single | 6 (20.0) | 7 (23.3) | 0.75c |
| Married | 24 (80.0) | 23 (76.7) | ||
| Education level | Illiterate | 5 (16.7) | 12 (40.0) | 0.24c |
| Elementary | 14 (46.7) | 10 (33.3) | ||
| Diploma | 5 (16.7) | 3 (10.0) | ||
| College | 6 (20.0) | 5 (16.7) | ||
| Job | Housewife | 19 (63.3) | 19 (63.3) | 0.74b |
| Employee | 3 (10.0) | 5 (16.7) | ||
| Farmer | 1 (3.3) | 2 (6.7) | ||
| Others | 6 (20.0) | 4 (13.3) | ||
| ASA class | I | 25 (83.3) | 26 (86.7) | > 0.97b |
| II | 5 (16.7) | 4 (13.3) | ||
| Height | 160.5 ± 4.7 | 160.1 ± 6.3 | 0.78d | |
| Weight | 67.3 ± 8.1 | 70.6 ± 11.0 | 0.19d | |
| PLSP | Occurrence | 24 (80.2) | 25 (83.3) | 0.73d |
Abbreviation: ASA, American society of anesthesiologists.
aValues are expressed as mean ± SD or No. (%).
bIndependent t-test.
cChi-square test.
dFisher exact.
In the clonidine group, 24 patients (80.2%) had PLSP, while 25 patients (83.3%) complained about pain in the placebo group immediately after LC (P = 0.739).
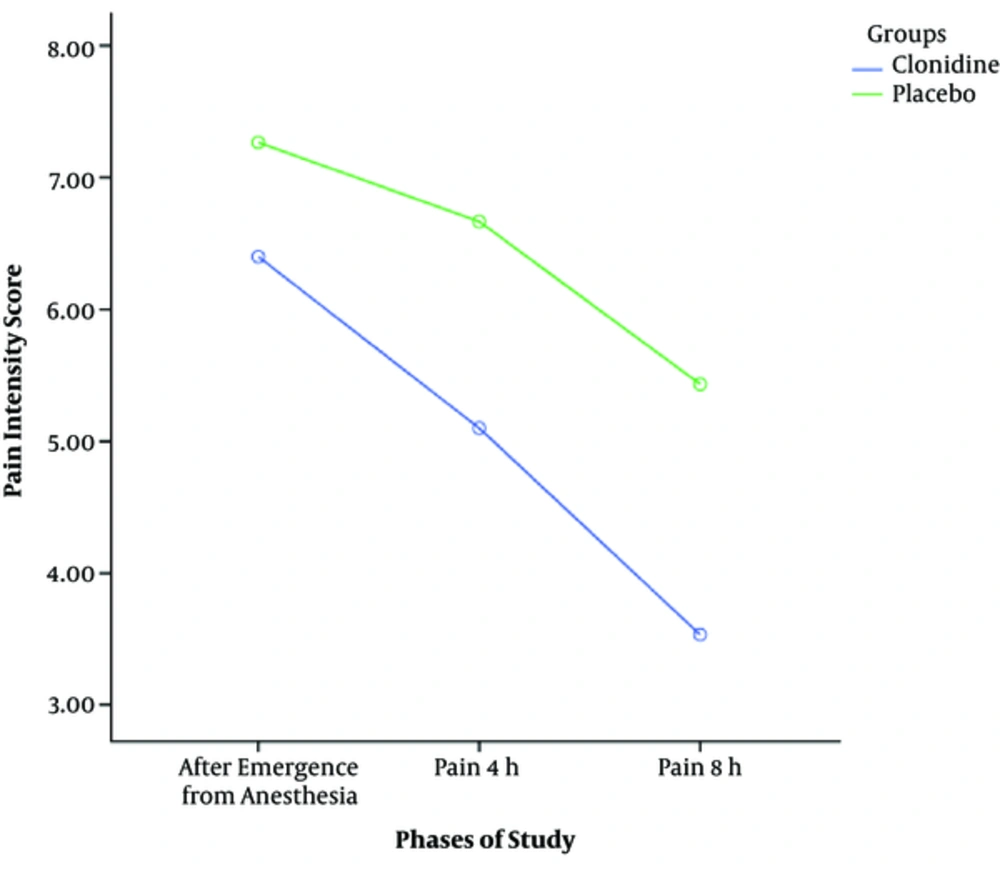
As shown in Table 2, a significant difference was found in the intensity of PLSP between the 2 groups at the emergence from anesthesia (P = 0.012), 4 and 8 hours after the operation (P = 0.001) (Table 2). Therefore, the clonidine group reported a larger reduction in pain level at these phases (Figure 2).
| Variable | Phase | Clonidine | Placebo | P Valueb |
|---|---|---|---|---|
| Post laparoscopic shoulder pain | After emergence from anesthesia | 6.4 ± 1.9 | 7.4 ± 0.6 | 0.012 |
| 4 hours after operation | 5.1 ± 2.1 | 6.6 ± 1.2 | 0.001 | |
| 8 hours after operation | 3.5 ± 2.2 | 5.4 ± 2.1 | 0.001 | |
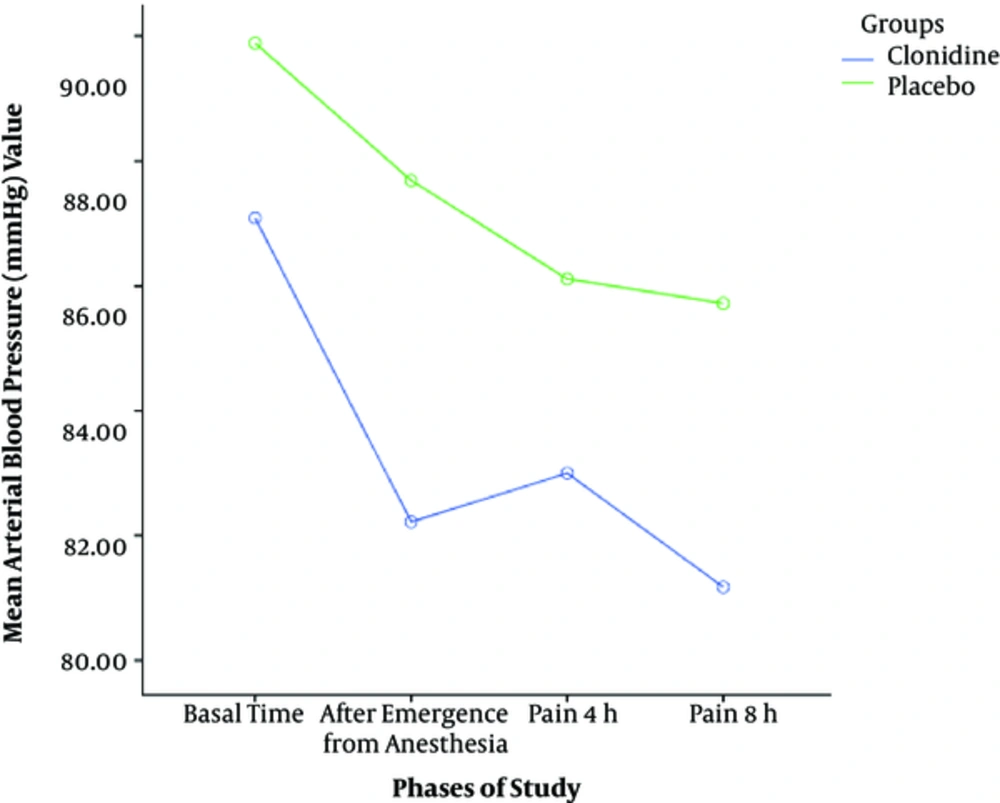
| Mean arterial blood pressure | Basal time | 87.0 ± 6.2 | 89.8 ± 4.3 | 0.058 |
| After emergence from anesthesia | 82.2 ± 10.3 | 87.6 ± 8.7 | 0.031 | |
| 4 hours after operation | 83.0 ± 11.3 | 86.1 ± 8.4 | 0.234 | |
| 8 hours after operation | 81.1 ± 11.9 | 85.7 ± 6.9 | 0.076 | |
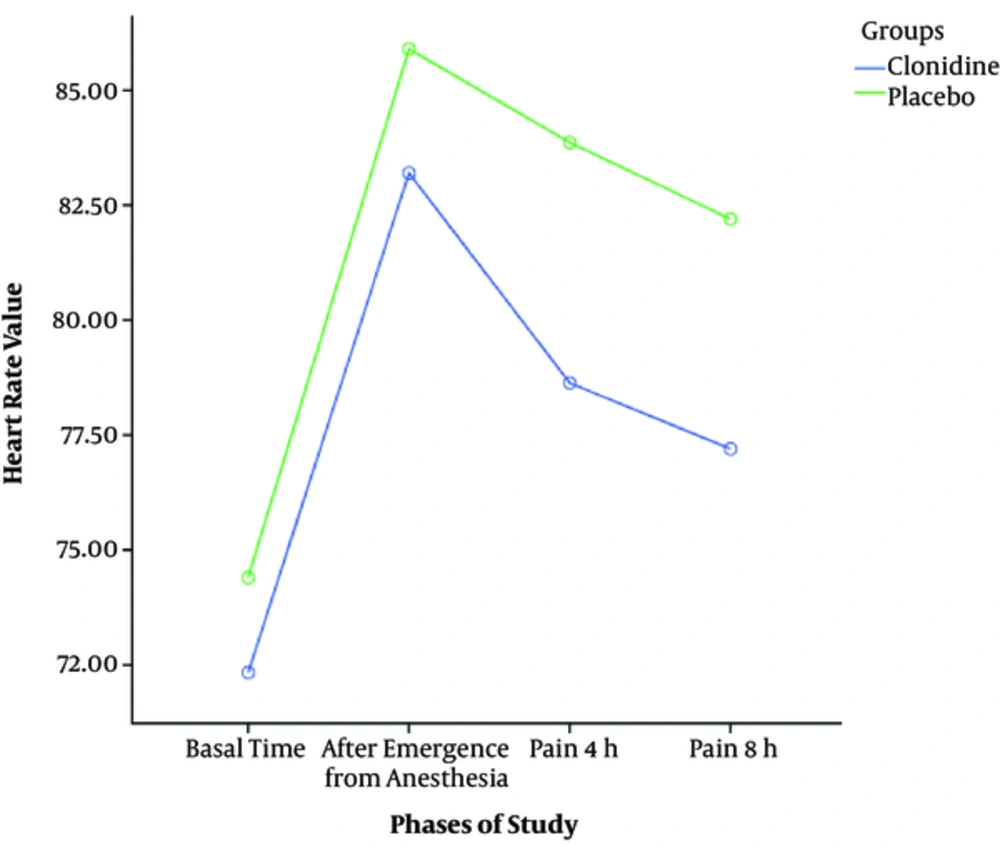
| Heart rate | Basal time | 72.3 ± 7.2 | 74.4 ± 7.2 | 0.275 |
| After emergence from anesthesia | 83.2 ± 14.0 | 85.9 ± 9.9 | 0.395 | |
| 4 hours after operation | 78.6 ± 11.5 | 83.8 ± 9.7 | 0.062 | |
| 8 hours after operation | 77.2 ± 10.3 | 82.2 ± 6.5 | 0.029 |
aValues are expressed as mean ± SD.
bIndependent t-test.
The result of independent t-test showed that there is no significant difference in MABP value between two groups prior to induction of anesthesia (P ≥ 0.05). As shown in Table 2, the result of this test indicated that there was no significant difference between the 2 groups at all measurements (P ≥ 0.05) with the exception of emergence from anesthesia time (P = 0.031). In this phase, mean value of MABP declined by 5.9% to basal time in the clonidine group and it declined by 2.5% in the placebo group (Figure 3).
Two groups of individuals were equal in terms of heart rate at basal time (P ≥ 0.05). The result of independent t-test demonstrated no statistically significant difference in heart rate between placebo and clonidine groups at basal time, emergence from anesthesia time, and 4 hours after the operation (P ≥ 0.05). However, the results of this test indicated that the mean heart rate significantly differed between the 2 groups at 8 hours (P = 0.029) (Table 2). The mean heart rate value in the clonidine group was less than the placebo group (Figure 4). The result of Fisher’s exact test showed no significant difference in side effects between the 2 groups during post-operative phases (P > 0.97). Incidence of side effects is reported in Table 3
| Variable | Clonidine (n = 30) | Placebo (n = 30) |
|---|---|---|
| Hypotension | 1 (3.3) | 0 (0.0) |
| Bradypnea | 2 (6.7) | 5 (16.7) |
| Nausea and/ or vomiting | 3 (10.0) | 2 (6.7) |
5. Discussion
This study was designed to survey the effect of oral clonidine on PLSP and hemodynamic respond after LC surgery.
Clonidine is a central alph2-receptor agonist, including sedative, anxiolytic, and analgesic properties, which may induce postoperative analgesia in the absence of related considerable side effects (19-24). Our results have shown that patients, who received a low dose of clonidine (0.2 mg) 90 minutes prior to induction presented lower level of PLSP, MABP, and heart rate levels compared to patients, who received placebo at emergence from anesthesia until 8 hours after the operation.
In this study, patients, who received premedication dose of oral clonidine, reported less PLSP during post-operative phases until 8 hours after the operation. This result is not compatible with a previous study, which has shown that administration of low dose of oral clonidine cannot improve postoperative analgesia significantly (25). However, some previous researches are consistent with this study (10, 21). Samantaray et al. demonstrated that clonidine premedication was effective in reducing pain intensity and analgesic consumption after thoracotomy surgery (10). Also, another clinical trial showed that clonidine could provide a relative postoperative analgesic effect in patients undergoing abdominal hysterectomy (25). Analgesia and sedation effect of clonidine could be explained by actions on the spinal cord and locus coeruleus, respectively (26).
Clonidine induced less increase in heart rate (at 8 hours after operation) and MABP (at emergence from anesthesia) values, postoperatively. These hemodynamic responses are congruent with previous studies (15, 21, 27-29). Singh et al.’s study indicated that administration of a low dose clonidine (150 μg) prior to induction in patients undergoing LC procedure could provide perioperative hemodynamic stability (27). Another randomized controlled clinical trial showed a single bolus dose of clonidine reduced additional metoprolol consumption in patients undergoing functional endoscopic sinus surgery (15). Das et al.’s study demonstrated clonidine at an oral dose of 150 µg is a safe and effective premedication, which provides stable hemodynamics in patients undergoing LC (29). These effects could have been the result of sympatholytic actions of clonidine by inhibiting norepinephrine release, reducing plasma cortisol concentration, and it’s central alpha 2 adrenergic action (10, 26).
The current finding showed that administration of low doses of oral clonidine is a safe method without any significant adverse effects. This is in line with findings of a similar study, which has not reported any significant side effects, including hypotension, bradycardia, bradypnea, nausea, and vomiting (27).
The main limitation of the study was the lack of recording of secondary outcomes, such as anxiety. Another limitation of this study was lack of recording of hemodynamic changes during intubation and operation, lack of recording of analgesic request, and maximum and minimum of pain intensity during the study.
6. Conclusions
The most obvious finding of this study was that administration of premedication low dose oral clonidine is not effective in preventing PLSP. However, it is safe and effective on PLSP intensity in the first postoperative hours. Also, clonidine perioperative administration causes further decrease in MABP and heart rate immediately after emergence from anesthesia. Further trials are recommended to determine the effect of clonidine on perioperative secondary outcomes, such as anxiety. Also, further studies are necessary to record and assess hemodynamic responds during intubation and operation, especially in patients with ASA III and IV.