1. Background
Airway management in morbid obese patients can present many challenges as these peoples have traditionally greater risks for difficult airway and difficult intubation compared to general people (1). Although obesity is not an independent risk factor for difficult airway, it is a factor that should be considered in evaluation of the airway, which depends on the measure or definition of difficult intubation (2). Obese patients have obesity-related airways and respiratory changes that can result in difficult airway management. Excess neck fat tissue deposition, reduced lung volumes, increased airway resistance, and increased oxygen consumption are encountered in obese patients and their combination can increase the risk of difficult intubation and consequently rapid desaturation in oxygen in the perioperative period (3). Preoperative airway evaluation in obese patients should include assessment of predictors of difficult mask ventilation beside those for difficult intubation. Optimizing preoxygenation can be achieved by a head-up position, CPAP (continuous positive airway pressure), or PEEP (positive end-expiratory pressure). During direct laryngoscopy, best laryngeal exposure is achieved when the patient is in the “ramped: position (4). Morbidly obese patients have excessive fat in their mouth, neck, pharynx, breast, thorax, and abdomen, which makes access to airway (intubation, tracheostomy) and patency of the upper airway (during sedation or mask ventilation) more difficult compared to lean patients. Moreover, the function of lungs decreases (decreased residual capacity and aggravated ventilation perfusion mismatch) (5). Recognizing the individual factors more closely related to difficult intubation has special importance. Several studies have shown that great neck circumference in morbidly obese patients is a predictor of difficult intubation (6-8). Ezri et al. examined the anterior neck of morbidly obese patients by ultrasound and demonstrated more difficult laryngoscopy in patients with larger neck circumference and greater amount of pre-tracheal soft tissue (9). In morbid obese patients, adipose tissue is located predominantly in the upper truncal and low cervical parts and is related to more oxygen consumption and higher incidence of cardiovascular disease (10). In this study, we evaluated the effect of manual caudal and downward displacement of lower cervical adipose tissue on laryngoscopic view in morbid obese patients.
2. Methods
After getting approval from the ethics committee of Tabriz University of Medical Sciences, 70 patients with BMI ≥ 35 candidate for elective surgery under general anesthesia, were enrolled in this study. Written informed consent was obtained from all subjects. Study was conducted in Imam Reza hospital (a university affiliated hospital) during Jan 2015 till Sept 2016 and registered in IRCT with the number of 201411213915N15. Inclusion criteria were older than 18 and ASA physical status I or II. The exclusion criteria included patients who had difficulty in airway management after anesthesia induction. After careful preoperative evaluation, patients were enrolled in the study. Mallampati score was noted for all patients in sitting position and before induction of anesthesia. All patients were monitored with ECG, Spo2, ETCo2, and BP and situated in ramped position as external auditory meatus was positioned in the same line as suprasternal notch. Patients underwent preoxygenation for 3 minutes and after that fentanyl 2 µg/kg, lidocaine 1 mg/kg and midazolam 0.03 mg/kg were injected. After 2 - 3 minutes, induction was performed with 2mg/kg propofol and 0.15 mg/kg atracurium. Laryngoscopy and intubation time was confirmed by nervestimulator with PTC (Post tetanic count) of 0. Patients were randomized (Block randomization) into 2 groups: with and without manual caudal and downward displacement of cervical adipose tissue displacement. Laryngoscopy was performed with a skilled anesthesiologist who was blinded to the study protocol. We draw a curtain on the cervical part of the patient to separate the anesthesiologist who was performing laryngoscpy with the other one who was performing manual displacement of adipose tissue. One anesthesiologist performed the laryngoscpy twice and rated the laryngoscopic view based on Cormack-Lehane grading. Another anesthesiologist performed manual caudal and downward displacement of lower cervical tissue during the first or second laryngoscopic attempt. Of course, his hand was on the patient's chest during both laryngoscopic attempts but the maneuver was performed only during 1 of the laryngoscopies. The maneuver was performed while the anesthesiologist made his dominant hand semi circle, thumb, and 2nd finger in 2 sides on trunk and stood in the right side of the patient. Laryngoscopic view with and without the maneuver, upper lip bite test, BMI, hyomental distance, and thyromental distance were noted for all patients. Difficult intubation was defined as more than 3 attempts or more than 10 minutes for a successful endotracheal intubation (10). All data were analyzed with SPSS statistical package number 17. We used the t-test for evaluation of the relation between age, weight, BMI, thyromental, and hyomental distance with difficult airway and used Chi-square test for the relation of difficult intubation with other variables. We used sign test for showing the relationship between performed maneuver and laryngoscopic grade. P value less than 0.05 was considered significant.
3. Results
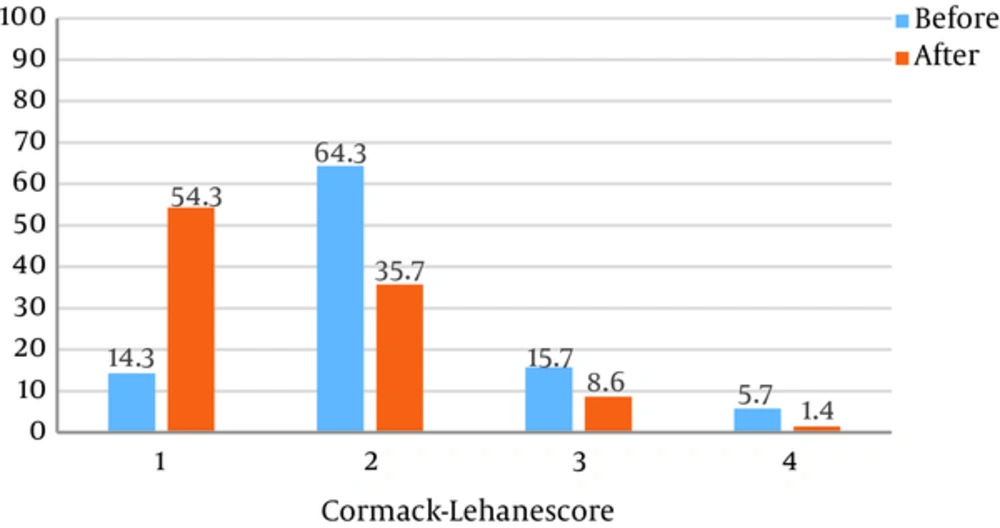
A total of 70 patients who were candidates for elective surgery under general anesthesia were enrolled in this study. Of the 70 patients, 39 were male and 31 patients were female. Difficult intubation was performed in 8 patients. Demographic characteristics of patients are shown in Table 1. As shown, there is no significant relationship between difficult intubation and age, weight, and BMI (Pvalue: 0.42, 0.84, and 0.25, respectively). In our study, 7 patients had loose teeth and 3 patients had large incisor teeth. The relationships between thyromental distance, hyomental distance, and difficult intubation were significant (P value: 0.01 and 0.005, respectively). Based on mallampati score, 14 patients had score I, 34 patients had score II, 20 patients had score III, and 2 patients had score IV. Comparing the laryngoscopic grade before and after performing the maneuver, a significant improvement in laryngoscopic view after the maneuver was achieved (P value < 0.001) (Figure 1). The number of patients in grade I, II, and III, based on upper lip bite test, was 14, 38, and 18, respectively. Table 2 shows correlation of different parameters with difficult intubation in this study. As the table shows, mallampati has the highest correlation with difficult intubation.
| Variable | Mean ± SD |
|---|---|
| Age | 50.66 ± 10.571 |
| BMI | 39.19 ± 2.794 |
| Weight | 113.71 ± 9.035 |
| Thyromental distance | 5.13 ± 0.818 |
| Hyomental distance | 5.051 ± 0.844 |
| Variable | P Value |
|---|---|
| Gender | 0.243 |
| Loose teeth | 0.133 |
| Large incisor | 0.002 |
| ULBT | 0.040 |
| Neck movement | 0.606 |
| Mallampati | 0.001 |
| Thyromental distance | 0.010 |
| Hyomental distance | 0.005 |
| Cormack-Lehane score | 0.001 |
4. Discussion
Results of the present study showed that caudal replacement of lower cervical adipose tissue could significantly improve the laryngoscopic Cormack-Lehane score. Prediction of difficult intubation and its management is important and challenging, especially in morbidly obese patients (11-13), the excess soft tissue of breast, neck, thoracic wall and abdomen and internally mouth, pharynx and abdomen in morbid obese patients tends to increase the rate of difficult intubation and decrease the patency of the upper airway and the function of the lungs. Therefore, considering this matter for the airway management of these patients can decrease morbidity and mortality. Anatomic changes associated with obesity contribute to difficult intubation and include limitation of the atlanto-axial joint and cervical spine movement by upper thoracic/low cervical adipose tissue. Short and thick neck, excess tissue folds in mouth and pharynx, thick submental fat tissue, supra-sternal, pre-sternal, and posterior cervical fat and large breasts in females are the additional factors leading to more difficult airway. The patient’s neck circumference is shown to be an individual important predictor of difficult airway in morbid obese patients. Juvin et al., in their study on 134 patients, showed that mallampati score and neck mobility were the factors associated with difficult intubation in patients with BMI > 30 (14). We showed similar results with mallampati score, however, neck mobility didn’t have significant correlation with difficult intubation in our patients. Brodsky showed that in patients with BMI > 40, mallampati score is the most important predictor of difficult intubation, which is similar to our results (15). They couldn’t show any significant relationship between thyromental distance and difficult intubation. They also indicated neck circumference at the level of thyroid cartilage of obese patients as a significant predictor of difficult laryngoscopy. The best predictor of difficult laryngoscopy was quantification of cervical soft tissue at the larynx and suprasternal notch (9). Few studies have concentrated on fat distribution in the anterior neck region. Whittle et al. showed that excess fat in submandibular region is a predictor of difficult intubation in morbid obese patients (16). A MRI study demonstrated that in spite of the greater amount of total body fat in women, men have more fat tissue distribution in the neck. This may clarify the reason for greater incidence of difficult intubation in males (17). Gonzalez et al. showed that difficult intubation was associated with a mallampati score of ≥ 3 and greater neck circumference, thyromental distance, and BMI. They recommended that for prediction of difficult intubation, neck circumference should be preoperatively examined (6). Bell et al. showed that neck circumference in morbid obese patients was a significant predictor of difficult airway, however, BMI was not (18). All the mentioned studies indicated that neck soft tissue could be a marker for difficult intubation, which may be due to reducing the anterior mobility of pharyngeal structures.
Based on the previous studies, increasing in neck soft tissue is accompanied by increased possibility of difficult intubation. As morbidly obese patients have substitution of so many fat tissues in their upper trunk/lower cervical and chest wall, there are many studies that have evaluated the effect of this fat tissue on laryngoscopy (19). Collins et al. compared the standard sniff position vs. ramped position. Ramped position was achieved by arranging blankets underneath the patient's upper body and head until horizontal alignment was achieved between the sternal notch and the external auditory meatus. They demonstrated that ramped position, in comparison to a standard sniff position, improved the laryngeal view in morbidly obese patients and could even decrease pneumonia (20). Greenland et al. showed that the external meatus and sternal notch reflected the situation of the clivus and glottis opening, respectively, which may help in correctly positioning any patient in the sniffing position before direct laryngoscopy in both obese and non-obese patients. Therefore, they defined ramped position as horizontal alignment of the sternal notch and external auditory meatus, which yields excellent view for laryngoscopy in morbid obese patients (21). Rao et al. in another study in patients with BMI >30 failed to show any improvement in the laryngoscopic view in the ramped position (22). The negative results of mentioned study may be due to the inclusion criteria as they enrolled patients with BMI > 30, not morbidly obese patients. In these patients, supine position decreases functional residual capacity, which results in more rapid deoxygenation. In addition, ramped position can passively displace chest wall fat tissue downward to make laryngoscopic view better. Previous studies showed that ramped position has some considerations: the success rate of intubation in ramped position for morbidly obese patients is more with skilled and fully trained anesthesiologists than less experienced ones. On the other hand, there is not many studies that evaluated the optimal height of the operating table for endotracheal intubation (23). Based on this hypothesis, we performed this study and our results showed that this maneuver can significantly improve the laryngoscopic grade of morbidly obese patients. This was a single center study and we need more studies with larger sample sizes to generalize the results. Moreover, we need more studies dividing obese patients based on their BMI to show the possible limit for BMI to achieve good results.
4.1. Conclusions
Rapid desaturation of oxygen may happen in obese patients. Possible problems of airway management should be evaluated and predicted, and oxygenation, ventilation, and airway management strategies should be optimized. Difficult tracheal intubation risk may be increased and risk should be assessed in a careful manner. Manual and caudal displacement of lower cervical adipose tissue can be added to "standard" preoperative airway assessment in morbid obese patients.