1. Background
One of the most important measures employed for patients under general anesthesia in the operating room, was to maintain patent airway and provide sufficient ventilation. Although several techniques and devices were developed for this purpose, most of them have special requirements.
The management of the airways is an essential component of anesthesia training and the inability to establish a secure airway is the most prevalent concern about anesthesia, in relation to mortality and morbidity. Laryngeal mask airway (LMA) plays an important role in modern anesthesia. It is usually used to maintain the airway during spontaneous breathing of patients undergoing elective short-term surgeries, having a difficult airway and under emergency situation. Correct placement of LMA needs some degree of expertise (1-7). However, LMA can be used in emergency conditions, where patients cannot be intubated. In an emergency practice, LMA is considered to be better than mask ventilation, yet has lower applicability compared with endotracheal intubation. The design of LMA allows for a patent way for ventilation from the epiglottis opening through the ventilation system. The LMA uses an inflatable silicon cuff to provide a laryngeal seal (2).
If the position of the LMA is optimal, its orifice will be appropriately inserted through the glottis. The tip of the LMA is placed in the initial parts of the esophagus, lateral portion of pear-shaped cavity and superior edge of the base of the tongue. The inflatable cuff is adjusted according to the anatomy of the airway and provides a relatively tight barrier against air leak. Proper placement of the LMA is required for appropriate anesthesia depth and suppression of airway reflexes to avoid gag reflex, coughing, and laryngeal spasm (2). Various anesthesia methods and techniques for LMA placement have been suggested (3, 7). The time needed for placement, to provide ventilation is referred to as the placement time. In the study of Bih- Chenlin et al., the mean of placement time was 16 seconds. Some anesthesiologists use muscle relaxant to facilitate LMA placement (4). Using LMA is easier in comparison with intubation and is associate with smooth emergence. If this is not done in the appropriate time, especially in high risk patients (e.g. patient with ischemic heart disease or hypertension) or patients with hypersensitive airway, adverse reactions, such as straining, coughing and intense abdominal muscle movement can lead to undesirable complications. The determination of the optimal time for LMA placement is of prime importance (5, 8). Therefore, the aim of the present study was to determine the appropriate placement time in patients under general anesthesia.
2. Methods
This was a two-blinded prospective study, in which the clinical trial was conducted on 96 cases for 6 months at Shohda teaching hospital, Tabriz, Iran. This clinical trial was registered (IRCT2016020226328N1) and approved by the ethical committee of Tabriz medical sciences (93.1 to 5.12). The patients were selected by internet randomization and informed consent was obtained before conducting the study. The power was 90%. The sample was divided to four groups (n = 24 cases). Patients undergoing surgery lasting less than 1 hour and within the age range of 16 to 65 years were included in the study; those with a history of pulmonary complications in their previous anesthesia use, laryngeal disorders in preoperative examination, allergy to anesthetic drugs, heart disease and hypertension or possible pulmonary aspiration, receiving psychotropic drugs or addiction to opioids, were excluded. The limitation of this study was that it was conducted at one center and by five anesthesiologists; other surveys will be required for other centers and anesthesiologists with different experience levels.
One anesthesiologist was responsible for drug administration, another took the face mask without having information about the termination time for propofol administration and the third person recorded the results without information about the administration and insertion time. In this study, the anesthesia induction technique was performed with 2 mg/kg propofol, 2 µg/kg fentanyl, and 0.03 mg/kg midazolam. The rate of propofol administration was 30 seconds. These drugs were administered by anesthesiologists, who were not aware of the infusion termination time.
The participants were divided to four groups, each with 24 cases, based on the time interval between anesthetic agent administration and intubation with classic LMA; that is, up to 15 seconds for the first group, 16 to 30 seconds for the second, 31 to 45 seconds for the third, and 45 to 60 seconds for the forth group.
Finally, data were collected through questionnaire administration, analyzed and then compared with respect to age, gender, easy intubation, need for additional drug administration, basic blood pressure before drug administration in 1, 3, and 5 minutes after the placement of cLMA, duration of cLMA, SaO2 before and after placement of LMA, coughing, patient’s movement, laryngospasm, gag reflex after intubation, appropriate ventilation allowance, presence of sore throat after surgery, number of attempts, extent of mouth opening, and leak in peri-LMA space.
The indices for evaluation of the above variables were as follows:
1- Easy placement, for the first attempt without resistance
2- Easy placement, for the first attempt with minimal resistance
3- Slightly difficult placement, but successful during the second attempt
4- Unsuccessful placement
Also, the rate of placement quality was determined based on the presence or absence of these variables:
1- Ventilation allowance
2- Gag reflex
3- Coughing
4- Patient’s movement
5- Laryngospasm
6- Decreased SaO2
7- Postoperative sore throat
8- Leak around the cuff seal
9- Extent of mouth opening
10- Hemodynamic changes
The data were analyzed by statistically descriptive methods (mean, standard deviation, frequency, and percentage), and the paired sample t-test was used for comparison of the pre and post-test mean value. Normal distribution of data was determined using Kolmogorov- Smirnov, and chi-square test was used for qualitative data. Data was analyzed with the SPSS 20 software. P values higher than 0.05 were considered statistically significant.
3. Results
The total number of cases was 96 (72 males and 24 females). The mean age of the participants was 40.64± 15.9 years old. The demographic variables are shown in Table 1.
| Variables | 1 | 2 | 3 | 4 | P Value |
|---|---|---|---|---|---|
| Mallampati class | 0.915 | ||||
| Class I | 13 | 14 | 15 | 14 | |
| Class II | 9 | 7 | 8 | 9 | |
| Class III | 2 | 3 | 1 | 1 | |
| BMI | 27.65 ± 4.76 | 27.35 ± 5.01 | 26.95 ± 4.91 | 28.01 ± 3.51 | 0.875 |
| Distance between teeth | 4.55 ± 1.84 | 4.47 ± 1.63 | 4.85 ± 1.81 | 4.90 ± 1.33 | 0.755 |
| Difficulty in ventilation, % | 34 | 36 | 33 | 35 | |
| Age | 39.93 ± 1.02 | 40.41 ± 2.64 | 39.87 ± 1.57 | 41.01 ± 1.15 | 0.085 |
| Gender, No. (%) | |||||
| Female | 5 (20.83) | 6 (25.00) | 7 (29.17) | 6 (25.00) | 0.932 |
| Male | 19 (79.17) | 18 (75.00) | 17 (70.83) | 18 (75.00) |
The rates of success were as follows: 56 cases (index 1), 26 cases (index 2), 10 cases (index 3), and 2 cases (index 4). In 18 cases of group 1, 13 cases of group 2, and 12 cases of group 4, the placement of LMA could be easily performed. The results showed that the placement of LMA was significantly easier for the first group compared with the other three groups (P = 0.03). Two cases (one case of group 1 and one case of group 4) had unsuccessful placement. Comparison of results between the groups revealed that placement with resistance was significantly higher in group 2 (P = 0.01).
However, there was no statistically significant difference of the placement difficulty among the other three groups. The placement of LMA was easily performed in most patients. In these patients, the mean placement time was 4.62 seconds (Min = 2 seconds, Max = 10 seconds). The mean of the placement time was 7.25 seconds in group 2, 25.8 seconds in group 3, and 43.5 seconds in group 4. The mean placement time for all the patients was 8.43 ± 10.
Additionally, the basic blood pressure before drug administration, 1, 3, and 5 minutes after the placement of LMA were measured. The results were as follows (Table 2):
| Variable | Min | Max | Mean | P Value |
|---|---|---|---|---|
| Basic systolic pressure, mmHg | 112 | 179 | 129.99 | - |
| Systolic pressure at min 1 | 103 | 168 | 127.79 | 0.035 |
| Systolic pressure at min 3 | 98 | 152 | 121.6 | 0.00 |
| Systolic pressure at min 5 | 95 | 149 | 116.09 | 0.00 |
| Basic diastolic pressure, mmHg | 60 | 102 | 77.23 | - |
| Diastolic pressure at min 1 | 60 | 93 | 75.45 | 0.04 |
| Diastolic pressure at min 3 | 54 | 88 | 71.88 | 0.00 |
| Diastolic pressure at min 5 | 56 | 82 | 68.56 | 0.00 |
The mean of the heart rate was higher 1 minute after the placement of LMA, than other times and was not statistically significant in comparison with the other groups. The comparison of the four groups showed that blood pressure had no significant difference at different times.
By increasing the time between propofol administration and the placement of LMA in the four groups, the mean time of the placement was increased. The difference between group 1 and 2 was not statistically significant (P = 0.089), yet there was a significant difference between group 1 and 3 (P = 0.03) and group 1 and 4 (0.00). Six patients showed postoperative sore throat (two cases of group 3 and four cases of group 4). This was significantly higher in group 3 and 4 (P = 0.00, P = 0.01).
In the present study, the placement of LMA was successful in 87% of cases. In one case, the placement of LMA was performed in the third attempt. The results indicated that the rate of success for LMA placement in one attempt was higher in group 1 and 2.
A severe gag reflex was only seen in one case. In all the groups, the absence of gag reflex could be observed. Coughing was observed only in one case (group 3). On the whole, 41 patients were immobile at the point of placement. One case of laryngospasm was seen in group 4.
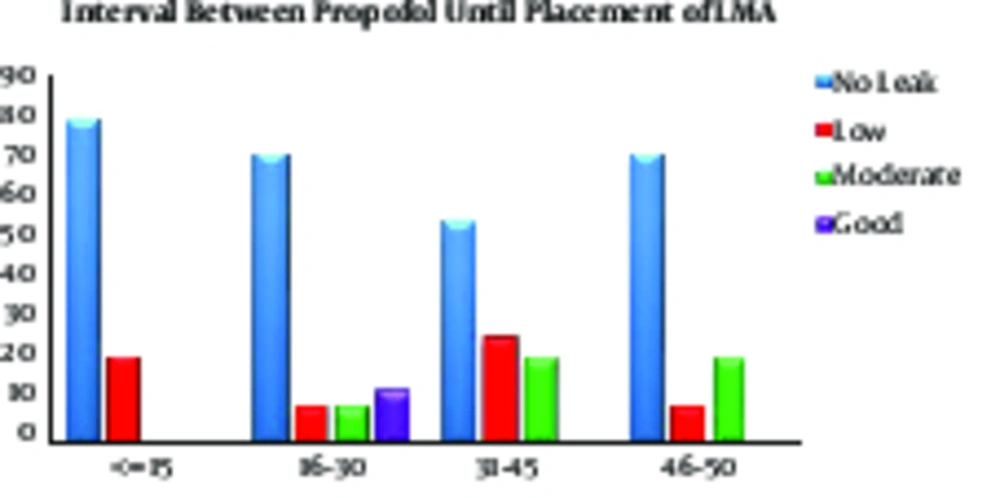
In all groups, coughing, patient immobility, and laryngospasm showed significant differences (P value = 0.00). The proportions of mouth opening at the placement time were classified as low, moderate, and good. Only two individuals did not have good measurements (Figure 1).
The results showed that there was no significant difference among the four groups. The mean SaO2 after the placement of LMA was 98.33%, 98.58%, 97.67%, and 96.29%, respectively.
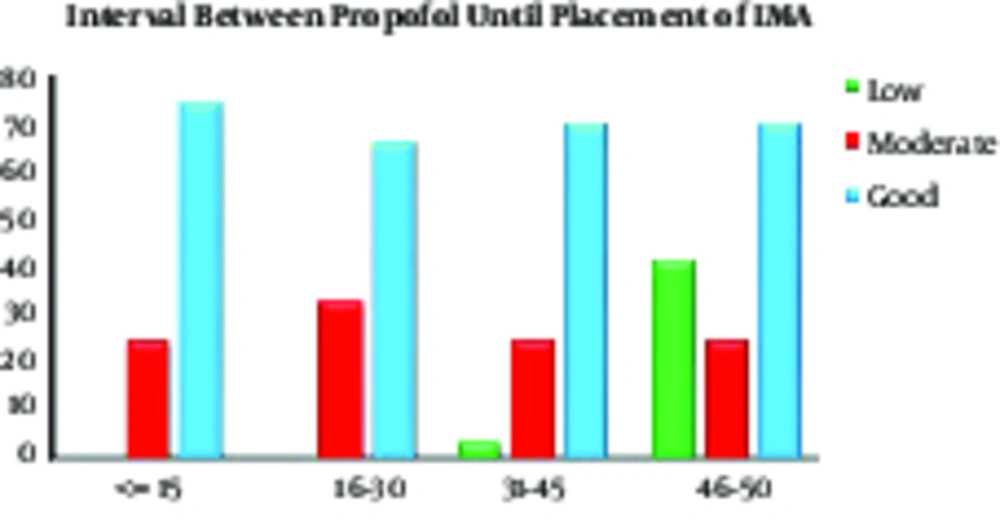
The rates of peri-cuff leak were classified to four groups: 1, no leak; 2, low leak; 3, moderate leak; and 4, high leak. In group 1, 79% of cases and in group 2, 12.5 % of cases (three cases) had no leak. The rate of leak in group 3 and 4 was higher than the other groups (Figure 2).
4. Discussion
The aim of this study was to determine the proper time for the placement of LMA in patients under general anesthesia. Overall, the results showed that decreased time interval between propofol administration and the placements of LMA gave a better outcome and lower complications.
Traditionally, several studies were conducted on the effects of propofol on easy placements of LMA, its quality, and adjunct drugs. For instance, Taha Wafa Salem et al., in their survey revealed that propofol in conjunct with midazolam was more efficient and increased the success rate of LMA placement, 2000 (2). Another study had the same results, indicating that adding remifentanil to propofol (as the main drug) had an appropriate influence on the placements of LMA (2, 5). The required time for the placement of LMA was 5.89 seconds (group 1), 6.25 seconds (group 2), 9.12 seconds (group 3), and 12.25 seconds (group 4), hence it is assumed that a prolonged interval after drug administration and initiation of the placement was associate with increase in the time for placement of LMA, yet the difference was not significant (P = 0.89). In the study of Dipasri Kumar et al., the mean time of LMA placement was 15 seconds (1), which was higher than the current results. In the study of Bih-Chern Lin et al., this time was 16 seconds (4). It could be suggested that the applied drugs and training of the anesthesiologist were different.
Furthermore, in the four groups of this study, the mean of diastolic and systolic blood pressure and heart rate had no significant difference at one, three, and five minutes after and before placement. Although, after anesthetic administration, diastolic and systolic blood pressure slowly declined until the fifth minute, the peak of the heart rate was observed in the first minute and then it slowly decreased. These results showed that the impact of time for placement on hemodynamic variables was negligible and acceptable until 60 seconds after the termination of propofol injection. The study of Dutta A revealed that patients usually experienced less anxiety with appropriate analgesia and so, their blood pressure and heart rate value decreased; in the present study the same results were observed.
On the whole, throat pain was less, compared with other related studies; for example, the postoperative throat pain rate reported by Nakayama et al. was 16% higher than this study. This is likely to be due to the improvement of LMA structure in the past years. Here, it was demonstrated that by increasing the time between the termination of propofol injection and placement of LMA, the rate of success decreased. The rate of successful placement in the first attempt was significantly higher. A similar study showed that the rate of success was slightly higher than 80%, which was obviously better than the current results (8). In the survey of Mohammadzade et al., the placement of LMA had several problems; one of which was inadequate proportion of mouth opening (50%). In another study, the authors demonstrated that the ED50 of remifentanil plus propofol for rapid airway management in the elderly was lower than that of the young ones (1). One randomized trial investigated 70 patients, who underwent an operation with anesthesia by LMA in two groups (trapezius squeezing, n = 35, and jaw thrust, n = 35). They inserted LMA after failed attempts to deal with trapezius squeezing or jaw thrust (1, 2). Agdashi et al. conducted a study for assessing the success rate of pediatric LMA placement in patients. They found muscle relaxants may be helpful in reducing complication, facilitating LMA insertion, and improving ventilation situation (9). Another group suggested that using I- GEL was associate with lower success rate than LMA insertion. However, the incidence of postoperative complications and the mean insertion time was not significantly different between the two groups (10). Imani et al. demonstrated that remifentanil in combination with propofol for anesthesia induction can induce optimum status for ideal endotracheal intubation as alfentanil, yet the patency of the vocal cords by remifentanil was better than alfentanil (11). Another study evaluated respiratory complications after prolonged ear, nose and throat (ENT) operations by tracheal tube or Laryngeal Mask Airway (LMA) and suggested low complications in the LMA group (12).
The lowest SaO2 in group 4 was explained by the prolonged time of LMA placement or resistance against the placement. The magnitude of leak around the mask during anesthesia in group 1 was lower than the other groups, yet this was not statistically significant. This could be due to improper placement of LMA.
The prevalence of cough was very low and not significantly different between the four groups. These results were similar to the results of Hye Jin park et al. (8). Some principles included oxygenation and prevention of trauma, which are achieved by devices, such as LMA (13). In pediatric patients, the success rate of correct placement of the Laryngeal mask airway (LMA) at the first attempt varied between 67% and 90% (14). Due to the selection of various techniques and different insertion periods by anesthesiologists, further survey is needed on these areas.
4.1. Conclusion
Based on the results of this study, delay in LMA placement after anesthetic drug administration increased the required time for placement. Prolonged time of LMA placement can lead to a high incidence of complications. Most of these complications can be induced by prolonging the time between anesthetic drugs administration and the initiation of LMA placement. However, the rate of placement time in the first attempt and its quality was decreased by lengthening the termination time of propofol administration.