1. Background
Delivery is probably the most important life event for women. Along with the pain of tissue injury and trauma, labor pain is a unique physiological process that includes the stimulation of nerve receptors and uterine contractions (1).
Cesarean section is one of the most common surgeries in the maternity ward (2). One of the cesarean section problems is the pain caused by tissue damage, organ dilation, and uterine contractions (3). Pain is one of the patients’ main concerns. Most patients consider postoperative pain as the most painful surgical experience. Pain can increase the length of stay in recovery. Lengthened recovery can delay the relationship between the mother and infant and disturb the breastfeeding process, negatively affecting the mother and infant health (4).
Injectable analgesics are the main source of post-surgery pain relief (5). However, they are used less frequently due to numerous side effects such as respiratory depression, drowsiness, nausea, vomiting, confusion, and fatigue (2, 6).
Analgesics inadequacy for pain relief alone (7), rarity, cost (2), and drug saving are some factors that attract nursing systems to use supplementary, non-pharmacologic treatments (8) and behavioral, non-invasive methods for pain relief. Behavioral methods are superior to invasive procedures due to the ease of use, increase in activity, and reduction in the cost of health care (9).
Most authors have recommended the use of wordless music to allow patients to focus on the music rather than the meaning of words (7). Nature-based sounds (N-BS) have been employed since 1984 to reduce and control anxiety and pain in the treatment of some diseases (10).
Numerous studies have shown the regenerative effects of natural environments in comparison with urban environments. These effects include improving welfare and reducing physiological stress responses (11, 12). Nature sounds have a positive emotional impact on all people (12). They have a higher relaxing impact than other interventions as shown in studies (13, 14).
Researchers at Johns Hopkins Medical Institutions (15) showed that distracting patients with a colorful mural of a meadow and the gurgle of a babbling brook during and after bronchoscopy significantly enhanced efforts to reduce pain.
To the best of our knowledge, no previous study has clearly focused on the comparison of the effects of playing N-BS and using headphones alone on pain severity.
2. Objectives
This study aimed to determine the effect of N-BS intervention and headphone intervention on pain severity after cesarean section.
3. Methods
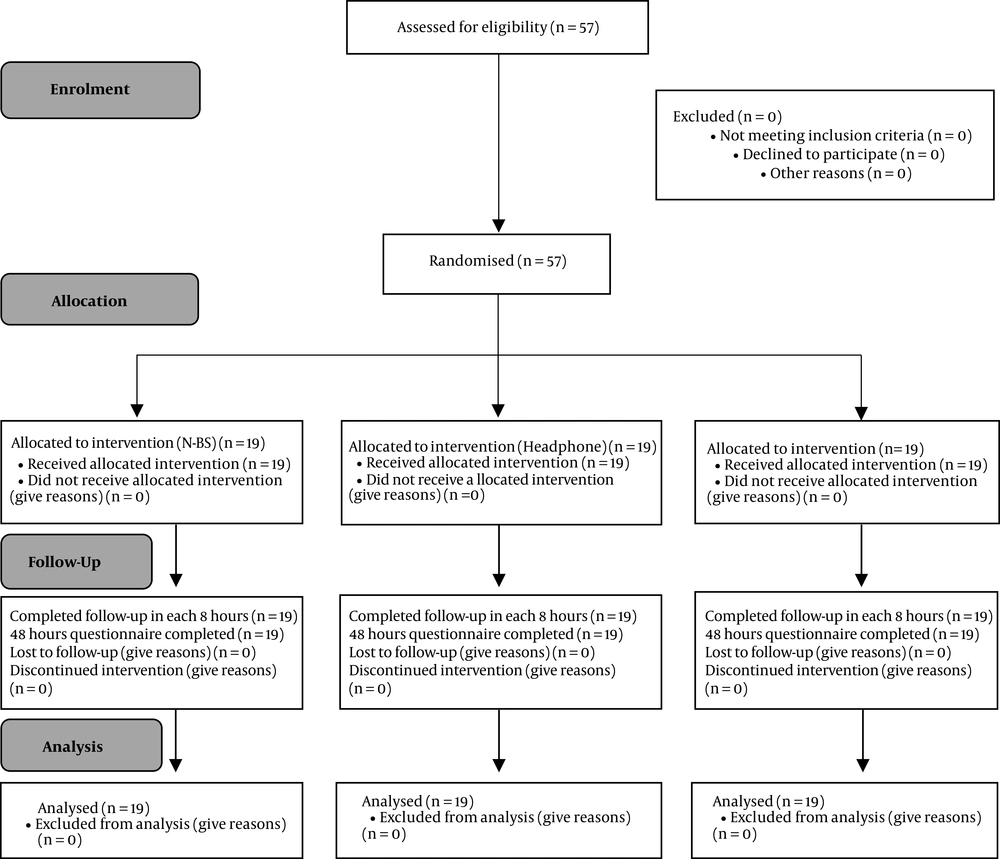
This prospective double-blind randomized trial was conducted from April 2015 to February 2016. The CONSORT flow chart of the randomized trial is shown in Figure 1. The statistical population consisted of all pregnant women who were candidates for elective cesarean section under spinal anesthesia referring to Motahari Hospital in Jahrom, Iran. The sample size was determined for the pain variable using Cohen table with α = 0.05, β = 0.5, a medium effect size, and the power of 80%. Therefore, a sample size of 52 patients was calculated that increased to 57 considering a dropout rate of 10% (19 in each group). Informed consent was taken from the participants. The researcher and women were blinded to treatment allocation. Randomization numbers were created from the Randomizer website of the Social Psychology Network.
After obtaining permissions, the investigator and a trained interviewer visited the maternity ward of the hospital and received the list of pregnant women undergoing a cesarean section. The inclusion criteria were the interest of mothers in the study participation, lack of cancer and chronic pains, lack of hearing or speech impairment, lack of addiction to drugs, sedatives, and alcohol, psychological and mental health, hemodynamic stability, a minimum education level of primary school, and consent to participate. The women were randomly divided into three groups: control, headphone (without playing N-BS), and N-BS. A demographic questionnaire was then completed.
3.1. Anesthesia
All cesarean section candidates received spinal anesthesia. Prior to the spinal anesthesia, 10 cc/Kg of ringer serum was administered to all women. In all cases, women were sitting and 5% Marcaine solution (10 mg) was injected by an anesthesiologist through the spinal needle No. 25. In the case of inadequate sensory block, general anesthesia was used and the patient was excluded from the study.
3.2. Interventions
Eight hours after the surgery, the investigator re-communicated with the mothers in the gynecology ward and evaluated the pain intensity. In the control group, mothers only received classical standard care (somehow personalized care based on patient’s post-operation condition with PRN as the analgesic treatment) and no intervention was performed. In the headphone group, in addition to classical standard care, the women used a headphone (without playing sounds) for 20 minutes. In the N-BS group, in addition to classical standard care, Marshal Headphones (Major) and MP3 Players (Sony NWZ-B183F) with 25 - 50 dB (10) were used for playing a collection of N-BS including birds song, soothing rain sounds, river streams, waterfall sounds, or a walk through the jungle. The comments of an audiologist were taken into account to calibrate the N-BS. The N-BS was played for 20 minutes in accordance with the intervention purposes. Each participant was asked to lie gently with closed eyes, resting, and following the flow of sounds. The family members of the patients were asked not to meet the participants during the intervention to avoid any reduction in the effectiveness of the intervention and patients’ cooperation. In the headphone group, mothers were asked to put headphones on their ears and stay silent for the same period as the intervention group. The mothers assigned to the control group were asked to rest for a similar duration.
Data collection was carried out at specified intervals. Women in the three groups were evaluated for the study parameter immediately before the intervention and 15 and 60 minutes after the end of the intervention. The investigator recorded pain intensity every eight hours after the surgery. The investigator was not aware of group allocation to limit bias in the recording of parameters. The parameters were completely recorded during 48 hours after the surgery. All nursing and medical measures were similar for all the three groups. The pain was evaluated when it did not interfere with drug intake. In order to prevent the spread of infection through the headphones, they were sterilized and the pads were replaced after each time of use.
3.3. Measurement Parameters
Data were collected using two questionnaires including a demographic form (age, job, weight, education, gestational age, and the number of pregnancies) and the visual analogue scale (VAS) for pain. If the mothers were sleeping, they were not woken up and zero was considered for them.
3.4. Statistical Analysis
Data were analyzed using descriptive statistics, such as mean and percentage, and statistical tests, such as ANOVA (parametric data) and Kruskal-Wallis (non-parametric data) concerning pain comparison between the three groups, followed by Tukey (parametric data) and Mann-Whitney (non-parametric data) tests for comparing a pair of groups using SPSS V. 16. The statistical significance level was considered P < 0.05.
4. Results
The mean age of the participants was 29.158 ± 6.058 in the N-BS group. In this group, the mean gestational age was 37.842 ± 1.980 weeks. Six mothers (31.6%) had a high school education and 12 (63.2%) had a previous surgical history. In the headphone group, the mean age of mothers was 26.737 ± 4.458. In this group, the mean gestational age was 38.316 ± 1.003 weeks. Seven mothers (36.8%) had primary school education and 13 (68.4%) had a previous surgical history. None of the mothers was a smoker. The results of ANOVA and chi-square tests showed no significant difference between the three groups in terms of demographic variables (P > 0.05). Therefore, the three groups were homogenous concerning demographic variables.
In the first shift after the surgery, the mean score of pain severity prior to the intervention was compared between the three groups. According to ANOVA, no significant difference was found (F = 0.292, P = 0.748). Fifteen minutes after the intervention, the difference in the mean pain scores became statistically significant between the three groups (F = 20.716, P < 0.001). According to the Tukey test, this significant difference was between the control and N-BS groups (P < 0.001) and between the headphone and N-BS groups (P < 0.001). However, the difference was not significant between the control and headphone groups (P = 0.953). Sixty minutes after the intervention, the mean scores were significantly different between the three groups according to the Kruskal-Wallis test (F = 10.459, P = 0.005). The Mann-Whitney test showed the same results as measured 15 min after the intervention (Table 1).
| VAS | N-BS Group | Headphone Group | Control Group | P Value | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Mean ± SD | CI Lower | CI Upper | Mean ± SD | CI Lower | CI Upper | Mean ± SD | CI Lower | CI Upper | ||
| First shift | ||||||||||
| Before | 5.789 ± 1.751 | 4.946 | 6.633 | 6.053 ± 1.580 | 5.291 | 6.814 | 6.263 ± 2.330 | 5.140 | 7.386 | 0.748a |
| 15 minutes | 2.211 ± 2.347 | 1.079 | 3.342 | 6.053 ± 1.840 | 5.166 | 6.940 | 6.263 ± 2.330 | 5.140 | 7.386 | < 0.001a |
| 60 minutes | 3.105 ± 2.514 | 1.893 | 4.317 | 4.684 ± 0.885 | 4.258 | 5.110 | 5.211 ± 1.182 | 4.641 | 5.780 | 0.005b |
| Second shift | ||||||||||
| Before | 5.105 ± 0.809 | 4.715 | 5.495 | 4.579 ± 1.644 | 3.787 | 5.371 | 4.579 ± 2.364 | 3.439 | 5.719 | 0.559a |
| 15 minutes | 1.684 ± 1.701 | 0.864 | 2.504 | 4.474 ± 1.679 | 3.664 | 5.283 | 4.579 ± 2.364 | 3.439 | 5.719 | < 0.001a |
| 60 minutes | 2.000 ± 1.633 | 1.213 | 2.787 | 4.895 ± 1.524 | 4.160 | 5.629 | 4.368 ± 1.342 | 3.722 | 5.015 | < 0.001a |
| Third shift | ||||||||||
| Before | 3.316 ± 2.056 | 2.325 | 4.307 | 3.947 ± 2.172 | 2.900 | 4.994 | 4.000 ± 1.915 | 3.077 | 4.923 | 0.523a |
| 15 minutes | 0.737 ± 1.368 | 0.078 | 1.396 | 3.895 ± 2.025 | 2.919 | 4.871 | 4.000 ± 1.915 | 3.077 | 4.923 | < 0.001a |
| 60 minutes | 1.526 ± 1.577 | 0.766 | 2.286 | 3.316 ± 1.157 | 2.758 | 3.874 | 4.211 ± 1.512 | 3.482 | 4.939 | < 0.001b |
aANOVA test.
bKruskal-Wallis test.
In the second shift of the first 24 hours, the mean scores of pain severity were compared between the three groups prior to the intervention. According to ANOVA, no significant difference was found (F = 0.588, P = 0.559). After 15 minutes of intervention, the mean scores became statistically significant between the three groups (F = 13.591, P < 0.001). According to the Tukey test, this significant difference was between the control and N-BS groups (P < 0.001) and between the headphone and N-BS groups (P < 0.001). The difference was not, however, significant between the control and headphone groups (P = 0.985). Sixty minutes after the intervention, the mean scores showed a significant difference between the three groups (F = 19.961, P < 0.001). The Tukey test showed the same results as measured 15 min after the intervention (Table 1).
In the last shift of the first 24 hours, the mean scores of pain severity were compared between the three groups prior to the intervention. According to the ANOVA test, no significant difference was found (F = 0.655, P = 0.523). After 15 minutes of intervention, the mean scores became statistically significant between the three groups (F = 20.337, P < 0.001). According to the Tukey test, this significant difference was between the control and N-BS (P < 0.001) and between the headphone and N-BS groups (P < 0.001). The difference was not, however, significant between the control and headphone groups (P = 0.982). Sixty minutes after the intervention, the mean scores showed a significant difference between the three groups according to Kruskal-Wallis (F = 20.971, P < 0.001). The Mann-Whitney test showed the same results as measured 15 min after the intervention (Table 1).
In the first shift of the second 24 hours, the mean scores of pain severity were compared between the three groups prior to the intervention. According to the ANOVA test, no significant difference was found (F = 1.514, P = 0.229). After 15 minutes of intervention, the mean scores became statistically significant between the three groups (F = 8.756, P = 0.001). According to the Tukey test, this significant difference was between the control and N-BS (P < 0.001) and between the headphone and N-BS groups (P<0.001). The difference was not, however, significant between the control and headphone groups (P = 0.732). Sixty minutes after the intervention, the mean scores demonstrated a significant difference between the three groups (F = 3.256, P = 0.046). However, the Tukey test indicated that the difference was not significant between the control and headphone groups (P = 0.964), control and N-BS groups (P = 0.060), and headphone and N-BS groups (P = 0.106) (Table 2).
| VAS | N-BS Group | Headphone Group | Control Group | P Value | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Mean ± SD | CI Lower | CI Upper | Mean ± SD | CI Lower | CI Upper | Mean ± SD | CI Lower | CI Upper | ||
| First shift | ||||||||||
| Before | 4.211 ± 1.398 | 3.536 | 4.884 | 3.105 ± 1.729 | 2.272 | 3.938 | 3.421 ± 2.694 | 2.122 | 4.719 | 0.229a |
| 15 minutes | 0.895 ± 1.286 | 0.274 | 1.514 | 2.895 ± 1.629 | 2.109 | 3.680 | 3.368 ± 2.629 | 2.101 | 4.635 | 0.001a |
| 60 minutes | 1.632 ± 1.571 | 0.874 | 2.388 | 2.895 ± 1.629 | 2.109 | 3.680 | 3.053 ± 2.345 | 1.922 | 4.182 | 0.046a |
| Second shift | ||||||||||
| Before | 2.895 ± 0.737 | 2.539 | 3.250 | 3.421 ± 1.835 | 2.536 | 4.305 | 3.632 ± 2.191 | 2.575 | 4.687 | 0.268b |
| 15 minutes | 0.421 ± 0.769 | 0.050 | 0.791 | 3.579 ± 1.953 | 2.637 | 4.520 | 3.632 ± 2.216 | 2.563 | 4.699 | < 0.001b |
| 60 minutes | 0.526 ± 0.697 | 0.190 | 0.862 | 3.421 ± 1.539 | 2.679 | 4.163 | 3.211 ± 1.398 | 2.537 | 3.884 | < 0.001a |
| Third shift | ||||||||||
| Before | 1.368 ± 0.895 | 0.937 | 1.800 | 1.211 ± 0.976 | 0.740 | 1.681 | 1.895 ± 1.449 | 1.196 | 2.593 | 0.277b |
| 15 minutes | 0.053 ± 0.229 | -0.058 | 0.163 | 1.263 ± 0.933 | 0.813 | 1.713 | 1.737 ± 1.447 | 1.039 | 2.434 | < 0.001b |
| 60 minutes | 0.158 ± 0.375 | -0.023 | 0.339 | 1.368 ± 0.955 | 0.908 | 1.829 | 1.947 ± 1.311 | 1.315 | 2.579 | < 0.001b |
aANOVA test.
bKruskal-Wallis test.
According to the Kruskal-Wallis test, the mean scores of pain severity were not statistically significant between the three groups in the second shift of the second 24 hours before the intervention (F = 2.634, P = 0.268). Fifteen minutes after the intervention, the mean scores became statistically significant between the three groups (F = 27.931, P < 0.001). According to the Mann-Whitney test, this significant difference was between the control and N-BS (P < 0.001) and between the headphone and N-BS groups (P < 0.001). The difference was not, however, significant between the control and headphone groups (P = 0.976). Sixty minutes after the intervention, the mean scores showed a significant difference between the three groups according to the ANOVA test (F = 30.887, P < 0.001). The Tukey test showed the same results as measured 15 min after the intervention (Table 2).
According to the Kruskal-Wallis test, the mean scores of pain severity were not statistically significant in the third shift of the second 24 hours before the intervention (F = 2.566, P = 0.277). After 15 minutes, the mean scores became statistically significant between the three groups (F = 24.845, P < 0.001). According to the Mann-Whitney test, this significant difference was between the control and N-BS groups (P < 0.001) and between the headphone and N-BS groups (P<0.001). The difference was not, however, significant between the control and headphone groups (P = 0.371). Sixty minutes after the intervention, the mean scores showed a significant difference between the three groups (F = 23.532, P < 0.001). The Mann-Whitney test showed the same as measured 15 minutes after the intervention (Table 2).
The lack of a significant difference in the mean scores of pain intensity before the intervention showed a similar pain severity in mothers prior to the intervention. The statistically insignificant difference between the control and headphone groups indicated that headphone only did not reduce the pain in the intervention groups. However, the significant difference between the control and N-BS groups showed that nature-based sound therapy reduced the mothers' pain. On the other hand, the significant difference between the headphone and N-BS groups showed that pain reduction in the N-BS group was due to playing N-BS not to use headphones. This highlights the effectiveness of nature-based sounds for reducing the mothers’ pain.
5. Discussion
The use of nature-based sounds (N-BS) is an inexpensive and non-invasive tool. Nurses can easily use N-BS along with other nursing care. Using N-BS, as a branch of alternative medicine, is the center of attention for promoting health indicators (16).
The results of our study showed that using N-BS can reduce pain. In this regard, a study by Hansen-Ketchum and Halpenny (17) reported that the N-BS intervention provides conditions that foster human and environmental health by reducing anxiety and enabling psychological and physical activity.
Tan et al. showed that sound therapy can decline anxiety, pain, muscle tension, and compression during daily care (18). Other investigations revealed that music is efficient in decreasing pain and anxiety in the cesarean section and mastectomy (19); this confirms the results of the current study.
Some studies, however, have reported inconsistent results. A study from Fasa, Iran, showed that music was not effective in reducing the patients' pain and anxiety. The study concluded that if music is selected according to the cultural context, better results would reach (20). Another study investigated the efficacy of music in the length of cesarean section in mothers undergoing spinal anesthesia in order to improve the mother's and infant's conditions. The clinical importance of music was unclear. However, few beneficial effects were observed on the pulse rate and birth satisfaction rate (21).
A study by Besel (22) on patients undergoing mechanical ventilation showed no difference in the pain score measured before and after listening to music, which is inconsistent with the results of our study. Some studies proved the positive effect of playing music selected by patients on pain reduction (23, 24). Although these studies differed from ours concerning the type of music, they showed that listening to music was effective in reducing pain. It is essential to note that neither types of music are superior to others for increasing the relaxation of patients. The most important point is interesting in music (25). Most authors suggested that music should be wordless in order to allow the patient to focus on the music rather than the meaning of words (26).
Nature-based sounds help in the compatibility with emotional stress and stimulation of relaxing reactions by diverting the listeners’ attention from anxiety, pain, and negative experiences to more pleasant ones (27, 28).
In the headphone group, headphones alone as a mediating factor could not lead to a reduction in the mothers’ pain. The study by Mirbagher Ajorpaz and Aghajani showed that headphones can block environmental sounds (29). Ikonomidou et al. stated that headphones are used to prevent the interference of the sounds in the ward (30). These reports are inconsistent with the findings of our study.
The results of our study showed that pain severity had no significant relationship with the history of surgery, which is consistent with a study by Bandyopadhyay et al. (31). The results also indicated a higher satisfaction rate in the N-BS group than in the controls. It was shown that 63.2% of the mothers in the N-BS group preferred to use this method in their next delivery; this is consistent with the results obtained by Ovayolu et al. (32).
Mothers were quite alert in our study and they were trained concerning the VAS. This helped them determine their pain severity.
5.1. Problems and Offers for Future Studies
The present study was conducted in a single hospital. As a result, generalizing the results might not be possible to other settings. Moreover, the study was limited to adult women aged 18-45 years who were undergoing a cesarean section. It may also limit the generalizability of the findings to other settings or populations. It is suggested that similar studies be performed in other age groups in further investigations.