1. Background
Renin angiotensin system is one of the effective factors that influence vascular tone. Angiotensin converting enzyme inhibitors (ACEIs) and angiotensin receptor antagonists (ARAs) are commonly used in hypertension control and are specially recommended for patients with ischemic heart disease, block the activation of the renin–angiotensin system, and could delay the progression of both heart failure and atherosclerosis (1). It is suggested that all antihypertensive agents should be continued until the day of surgery. However, this idea is not significantly distinguished about ACEIs and ARAs. Some studies have been reported that consumption of ACEIs and ARAs, until the day of surgery caused hypotension during anesthesia induction (2-4). This point is very important in patients who are a candidate for open-heart surgery with cardiopulmonary bypass (5). It is important to consider that some premedication drugs like benzodiazepines (midazolam), opioids (remifentanil), and anti-convulsion agents (gabapentin and pregabalin) can cause hemodynamic changes during anesthesia induction (6, 7). In some studies preoperative ACEI / ARB consumption increased use of intravenous vasoactive medication, however, it did not increase major adverse cardiac events, stroke, or death. Therefore, the use of preoperative ACEI /ARB appears safe before surgery (8). There are controversies about whether preoperative angiotensin-converting enzyme inhibitor (ACEI) therapy is associated with adverse outcomes after coronary artery bypass grafting (CABG) (9, 10). In some studies preoperative ACEI usage in patients undergoing CABG can decrease in-hospital mortality (11). Renin angiotensin system activation during rewarming and after separation from CPB, preserves systemic vascular resistance, however, blockade of this system with ACEIs and ARAs may cause hypotension and necessity of vasopressors injection. During CPB, hypoxia, hypo perfusion, hemodilution, and systemic inflammatory responses can cause hypotension (12), which is not constant and is eliminated with body vasoactive responses (13). In some cases low dose vasopressors are sufficient. However, if severe vasodilation due to chronic consumption of ACEIs and ARAs occurs during CPB, the weaning process will not be probable and high dose vasopressors will be needed (14). Some investigations have reported diminishing ischemic events, myocardial infarction, renal failure, and mortality rate by ACEIs and ARAs administration (11, 15, 16). Due to these contrary findings about ACEIs and ARAs, the aim of our study was to determine the effect of chronic consumption of ACEIs and ARAs on blood pressure and inotrope consumption after separation from cardiopulmonary bypass (17, 18).
2. Methods
This study was conducted with the approval of the scientific and ethical review boards of Urmia University of Medical Sciences. In the prospective analytical study, 200 patients who were scheduled for coronary artery bypass graft surgery (CABG) were enrolled in our prospective analytic study. All patients were ASA (American society of anesthesiologists) physical status II-III according to the ASA’s classification system. Subjects were assigned into two groups: those who were treated with either ARAS or ACEIs (case group n = 100) over at least 2 months or those who were not treated with any RAS antagonists (control group, n = 100) were enrolled. Patients ASA IV and more, with ejection fraction less than 40%, with abnormal liver function tests, with the history of endocrine disorders, with renal failure, and who received other antihypertensive agents (beta blockers, calcium channel blockers, nitrates and diuretics) were excluded from the study. Preoperative evaluation was performed in all patients. Basic monitoring including electrocardiography, arterial saturation of oxygen (SaO2), heart rate, and Bispectral index (BIS) (A-2000 XP version 3.11, aspect Medical system, USA) was done for all patients at the time of their entrance into the operation room. All patients were premedicated with intravenous 3 µg/kg of fentanyl and 0.015 mg/kg of midazolam. Arterial line was prepared in the radial artery of the non-dominant hand with a catheter number 20 for invasive blood pressure monitoring. Anesthesia was induced using 0.05 mg/kg midazolam, 10 µg/kg fentanyl, and 2 mg/kg intravenous sodium thiopental. Cisatracurium 0.1 mg/kg was administrated to facilitate intubation. After anesthesia induction, central venous catheter was prepared in the right external jugular vein for central venous pressure monitoring. Before cardiopulmonary bypass, maintenance was with oxygen and isoflurane. Any decrease of mean arterial pressure under 60 mmHg was treated with vasoconstrictor included repeated doses of phenylephrine 100 µg boluses. Patients were monitored during surgery. All the monitoring instruments were calibrated. The BIS was in range of 50 - 55 and the capnography was in the normal range during surgery. Furthermore, central venous pressure, mean arterial blood pressure, heart rate, and phenylephrine doses were checked and recorded in different times including: after induction (T1), before cardiopulmonary bypass (T2), and after separation from cardiopulmonary bypass (T3). All gathered data were statistically analyzed via chi-square and independent t-tests, or Fisher’s exact and Mann-Whitney U tests where needed, by using SPSS software version 19 (Chicago, IL).
3. Results
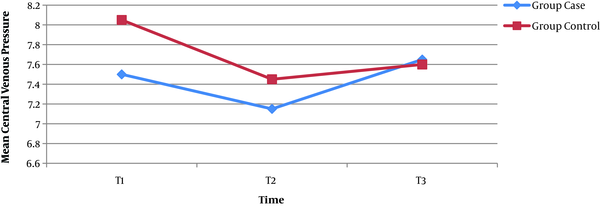
In this prospective analytic study, 200 ASA II-III patients were enrolled. Demographic and clinical characteristics were compared between two groups. We did not have any data regarding the rate of preoperative HTN in our patients; due to the fact that when they came to the operation room, they were under chronic treatment with ACEIs and ARAS. The mean age was 63.65 ± 9.47 years in the case group and 60.50 ± 8.30 years in the control group. There was no significant age difference between the two groups (P = 0.27). In the case group, 12 (60%) were male and 8 (40%) were female, 14 patients (70%) in control group were male and 6 (30%) were female (P = 0.37). The mean pumping time was 114.60 ± 18.79 minutes in the case group and 123.55 ± 28.53 minutes in the control group. Mean aortic cross clamp time was 75.60 ± 10.98 minutes in case group and 85 ± 27.38 minutes in control group. Mean preoperative ejection fraction was 44.25% ± 7.82% in case group and 43.42% ± 8.82% in control group. There was no significant difference in mean pumping time, mean aortic cross clamp time, and mean preoperative ejection fraction between two groups. Mean central venous pressure after induction of anesthesia (T1) was 7.50 ± 2.11 mmHg in case group and 8.05 ± 2.02 mmHg in the control group. Before CPB (T2) this was 7.15 ± 2.30 mmHg in case group and 7.45 ± 2.32 mmHg in control group. After separation from CPB (T3), this was 7.65 ± 2.03 mmHg in case group and 7.60 ± 2.08 mmHg in control group. There was no statistically significant difference in mean central venous pressure between two groups. Mean arterial pressure at T1 was 84. 20 ± 7.40 mmHg in case group and 85.25 ± 7.74 mmHg in control group. At T2, this was 77.40 ± 6.71 mmHg in case group and 81.30 ± 7.04 mmHg in control group. At T3, this was 83.10 ± 8.55 mmHg in case group and 6.85 ± 84 mmHg in control group.
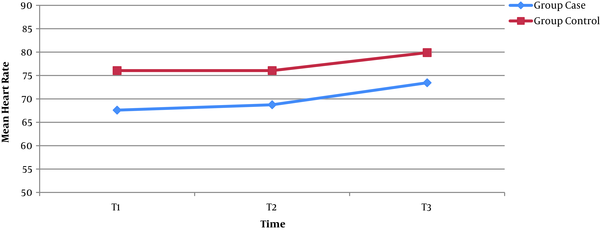
Mean heart rate in case group was 67 ± 10 bpm at T1, 68 ± 10 bpm at T2, and 73 ± 10 bpm at T3 and in control group was 76 ± 13 bpm at T1, 76 ± 13 bpm at T2, and 79 ± 12 bpm at T3. There was no statistically significant difference in mean arterial pressure and mean heart rate between two groups. The average mean arterial pressure during CPB was 63 ± 12 mmHg in case group and 66 ± 10 mmHg in control group (P = 0.4). Total dose of phenylephrine bolus injection during CPB was 1.5 ± 0.7 mg in the case group and 1.4 ± 0.6 mg in the control group (P = 0.4). Neither in case group nor in control group were inotropes needed during weaning from CPB and rewarming.
| Parameters | Case | Control | P Value |
|---|---|---|---|
| Mean pumping time, min | 114.60 ± 18.79 | 123.55 ± 28.53 | 0.24 |
| Mean aortic cross clamp time, min | 75.60 ± 10.98 | 85 ± 27.38 | 0.16 |
| Mean ejection fraction, % | 42.25 ± 7.82 | 43.42 ± 8.82 | 0.75 |
Comparison of the Mean Values of the Parameters Between the Case and Control Groups
| Parameters | Case | Control | P Value |
|---|---|---|---|
| Mean CVP in T1, mmHg | 7.50 ± 2.11 | 8.05 ± 2.02 | 0.45 |
| Mean CVP in T2, mmHg | 7.15 ± 2.30 | 7.45 ± 2.32 | 0.68 |
| Mean CVP in T3, mmHg | 7.65 ± 2.03 | 7.60 ± 2.08 | 0.93 |
| MAP in T1, mmHg | 84.20 ± 7.40 | 85.25 ± 7.74 | 0.66 |
| MAP in T2, mmHg | 77.40 ± 6.71 | 81.30 ± 7.04 | 0.08 |
| MAP in T3, mmHg | 83.10 ± 8.55 | 84 ± 6.85 | 0.71 |
| Mean HR in T1, bpm | 67.60 ± 10.12 | 76.05 ± 13.78 | 0.27 |
| Mean HR in T2, bpm | 68.75 ± 10.43 | 76.05 ± 13.78 | 0.06 |
| Mean HR in T3, bpm | 73.45 ± 10.76 | 79.90 ± 12.54 | 0.08 |
Comparison of the Mean CVP, MAP and Mean HR in Three Different Times Between the Case and Control Groupsa
4. Discussion
In this study we investigated the effect of chronic consumption of ACEIs and ARAs on hemodynamic variables and inotropes administration during weaning from CPB. Sympathetic nervous system, arginine vasopressin, and renin angiotensin system are the main vasopressor systems in blood pressure stability. The effect of angiotensin II in this process is due to its receptor. The advantage of ARAs in comparison with ACEIs is its specific effect on renin angiotensin system (13). It is well defined that renin angiotensin system antagonists administration in the preoperative period can suppress vasoactive responses due to vasoconstriction neurohormones like arginine vasopressin (13), which may cause hypotension and need to vasoactive drugs during CABG in patients who had chronically received these agents. During CPB, during blood circulations in pipes and oxygenator, inflammatory mediators are produced and decrease systemic vascular resistance. Some studies have explained the effect of ARAs to use vasoactive drugs during weaning from CPB. Deakin and collogues announced that chronic consumption of ACEIs decreases systemic vascular resistance, mean arterial pressure, and need to inotrope injection (19). In our study, we did not evaluate the systemic vascular resistance. There was no significant difference in mean arterial pressure between two groups and entirely no patient needed vasoactive agents during weaning from CPB and rewarming. This finding correlates with Kinoshita᾿ study, which explained that preoperative enalapril administration did not cause any hemodynamic changes during surgery (15). Our results did not correlate with Devbhandari᾿s investigation in which the mean arterial pressure was higher in the group who received ACEIs. However, they explained that according to different ideas about ACEIs continuing or discontinuing, it is necessary to design comprehensive studies for this point (20). In our study there was no significant difference in mean arterial pressure, mean central venous pressure, and vasopressor injection requirement between two groups. Sometimes blood pressure decreasing may occur with these agents (21), however, in our study, as the patients were under usual dosages of ACEIs and ARAs, significantly hypotension was not seen. Therefore, we can result that other factors may affect mean arterial pressure and hemodynamic changes during surgery and more study designing is needed. Our results are also in conflict with the new “2017 EACTS guideline” (European association for cardio-thoracic surgery) that recommends to stop ACEI/ARB before surgery. Maybe preoperative ACEI/ARB dosages make this difference.
One of the limitations of this research is that we did not separate consumers of ACEIs from ARAs and also different dosages were not compared. Therefore, it is recommended that in further studies, ACEIs and ARAs will be investigated separately and the efficacy of different dosages on blood pressure and inotrope injection necessity will be evaluated. 2-We did not have any data regarding the rate of hypertension, which was the reason of ACEIs or ARAs consumption in preoperative period in each group.