1. Background
Adequate postoperative analgesia is a prerequisite for successful day surgery. At the same time, adequate postoperative analgesia in a day surgery setting is challenging for several reasons. Firstly, patients have to manage their pain at home by themselves (1) and secondly, the arsenal of analgesics and route of administration of analgesics (i.e. no epidural or intravenous administration) are limited. Moreover, pain management in a day surgery setting is becoming even more demanding due to the recent evolution in day surgery towards more complex and painful surgical procedures.
Most studies analyzing postoperative pain have focused on the immediate postoperative course and classified the different types of surgery to a wide range of surgical disciplines, such as general, urological or orthopedic surgery (1, 2) or evaluated only a small number of surgical procedures (3, 4) making comparison between a global range of surgical procedures and their impact on postoperative pain impossible. Consequently, postoperative pain management has mainly focused on the first two postoperative days and based on a broad discipline-specific manner. Additionally, there is also a lack of pain studies for “minor” surgical procedures, often performed in a day surgery setting, because of the belief that these procedures elicit minor, and even no postoperative pain (5).
In day surgery settings, a rapid restore of self-care is of utmost importance. Adequate pain management in the first three to five postoperative days is an important tool to achieve this restoration of self-care (6). An optimal identification of painful surgical procedures is a prerequisite for the development of future preventive, procedure-specific pain-treatment schedules. Moreover, to reduce moderate to severe postsurgical pain, additional measures, such as a better preoperative empowerment of the patient and the implementation of a tailor-made home and follow-up care schedule, should be considered. Therefore, a more profound understanding of the variability of acute postsurgical pain (APSP) after different types of day surgery is needed.
A strong association between preoperative pain and postoperative pain has already been demonstrated by several studies (7-12). In this context, it could be of great value to demonstrate this pre- and post-operative pain relationship for specific surgical procedures. The purpose of this study was two folds: Firstly, to evaluate the prevalence of APSP on the fourth postoperative day, in a large adult population undergoing various types of day surgery. Secondly, to assess the predictive value of preoperative pain for the development of moderate to severe postsurgical pain after a wide range of surgical procedures.
2. Methods
The present study analyzed data from a large cohort of patients, who participated in a prospective longitudinal cohort study, assessing both pain outcomes as well as prevalence and possible predictors of patient non-adherence to pharmacological acute pain therapy at home after day surgery. The methods of this study and the results on patient non-adherence have been reported elsewhere (13).
Briefly, the study was approved by the institutional Ethics Committee of the Maastricht University Medical Center+ in 2008 and written informed consent was obtained from all patients. All patients that underwent day surgery were eligible to participate. Exclusion criteria were age of younger than 18 years, inability to express themselves, visual dysfunction, and insufficient understanding of Dutch (13).
2.1. Procedure and Questionnaires
Patients planned for day surgery at the Maastricht University Medical Center+ between November 2008 and April 2010 were asked to participate. All patients received an envelope containing information about the study, a baseline and a follow-up questionnaire, and two return envelopes. Patients were asked to complete the baseline questionnaire one week before the surgery. At baseline, demographics (age, gender, educational level, and work status), average pain intensity over the past week, and prescribed and over-the-counter analgesic use were assessed. Average pain intensity was measured by an 11-point Numeric Rating Scale (NRS; where 0 = no pain, and 10 = worst pain imaginable). An NRS value between four and five was applied for moderate postoperative pain (9, 10). Severe postoperative pain was defined as an NRS > 5 (14, 15). The follow-up questionnaire had to be completed on the fourth day after the surgery. The follow-up questionnaire included questions regarding average and present pain intensity related to surgery and the influence of pain on daily activities during the first four postoperative days, also using the 11-point NRS. Only patients, who returned both the baseline and the follow-up questionnaire were included in the analyses. Clinical information (i.e. ASA physical status, surgical procedure, and type of anesthesia) was acquired by systematic chart review. Patients received a standardized prescription for postoperative analgesics (i.e. acetaminophen 1000 mg four times a day or acetaminophen/tramadol 650/75 mg four times a day). Instructions were given to start first with acetaminophen and only to switch to acetaminophen/tramadol in case the first line therapy did not provide sufficient control of pain.
2.2. Statistical Analysis
Homogenous surgical groups consisting of at least 20 similar or closely related procedures were created to compare pain outcomes after various types of surgery (5). Potential loss of statistical power and precision was prevented by using multiple imputation to impute any variables with missing data. The number of imputations was set to 10. The presented patient data in the results are based on the original data. Descriptive statistics were performed on baseline and follow-up data using mean (SD) and percentages (%), and for pain data, median was used (25th to 75th percentile). The researchers analyzed the dataset based on these definitions.
To assess the predictive value of preoperative pain for acute postoperative pain for each type of surgery, univariate logistic regression analysis was performed. The reported results of the regression analyses were based on the pooled outcome of the 10 data sets. The regression analysis was stratified for the surgical procedure, and an overall odds ratio was calculated. An additional post-hoc regression analysis was performed to determine if the variability of the predictive value of preoperative pain between the procedures was affected by the procedure-specific variability in preoperative pain prevalence. Procedures were labeled as having a high prevalence of preoperative pain if the prevalence was ≥ 20%. Procedures with a prevalence of < 20% were labeled as having a low preoperative pain prevalence. Then, the overall odds ratio was calculated again, including preoperative pain prevalence. A p-value of < 0.05 was considered statistically significant. All analyses were performed using SPSS version 23.0 (SPSS Inc, Chicago, IL).
3. Results
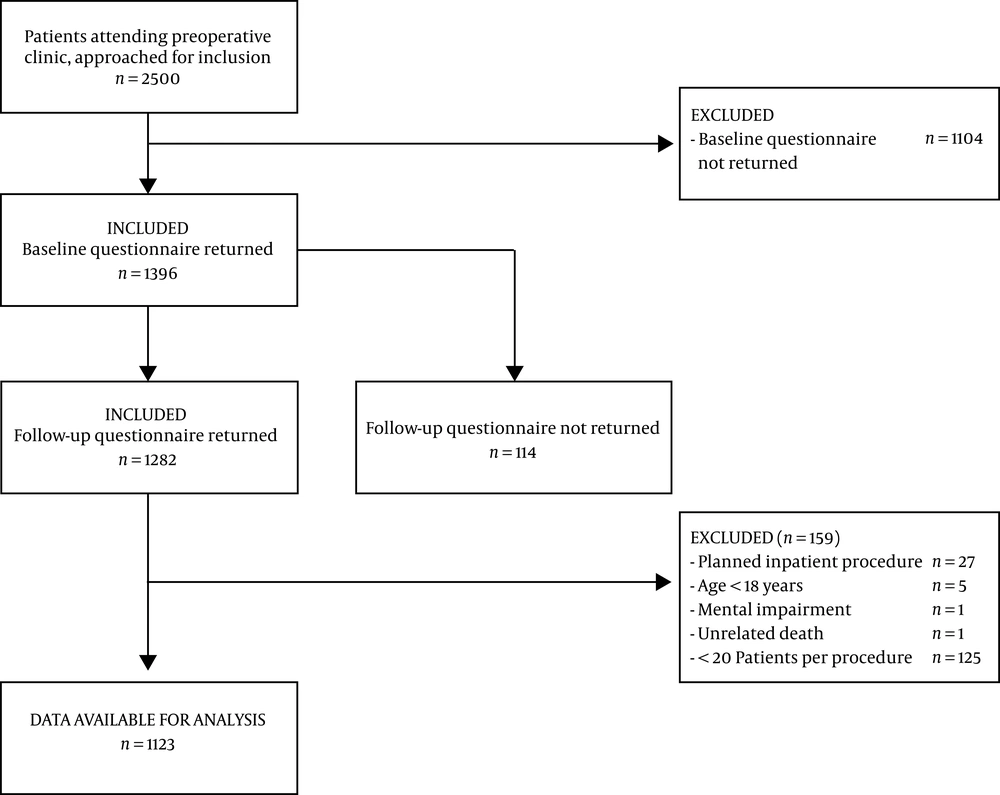
In total, 2500 patients were invited to participate in the study. Only data of 1123 patients were used for analysis as shown by Figure 1.
Baseline patient characteristics are presented in Table 1.
| Variables | Values |
|---|---|
| Age, y | |
| Mean ± SD | 52.5 ± 14.2 |
| Range of age | 18 - 88 |
| Missing data | 0 |
| Gender | |
| Female | 615 (54.8) |
| Male | 508 (55.2) |
| Missing data | 0 |
| Educational level | |
| None, elementary school | 79 (7.1) |
| High school | 797 (71.8) |
| College, university | 234 (21.1) |
| Missing data | 13 |
| ASA physical class status | |
| I | 565 (51.4) |
| II | 484 (44.0) |
| III | 51 (4.6) |
| Missing data | 23 |
| Preoperative pain | |
| Yes, NRS > 3 | 425 (38.7) |
| No, NRS < 3 | 674 (61.3) |
| Missing data | 24 |
| Preoperative analgesic use | |
| Yes | 274 (24.7) |
| No | 836 (75.3) |
| Missing data | 13 |
| Type of anesthesia | |
| General | 877 (78.3) |
| Loco-regional | 183 (16.3) |
| General and loco-regional | 60 (5.4) |
| Missing data | 3 |
Abbreviation: NRS, Numeric Rating Scale.
a Values are expressed as No. (%) unless otherwise indicated.
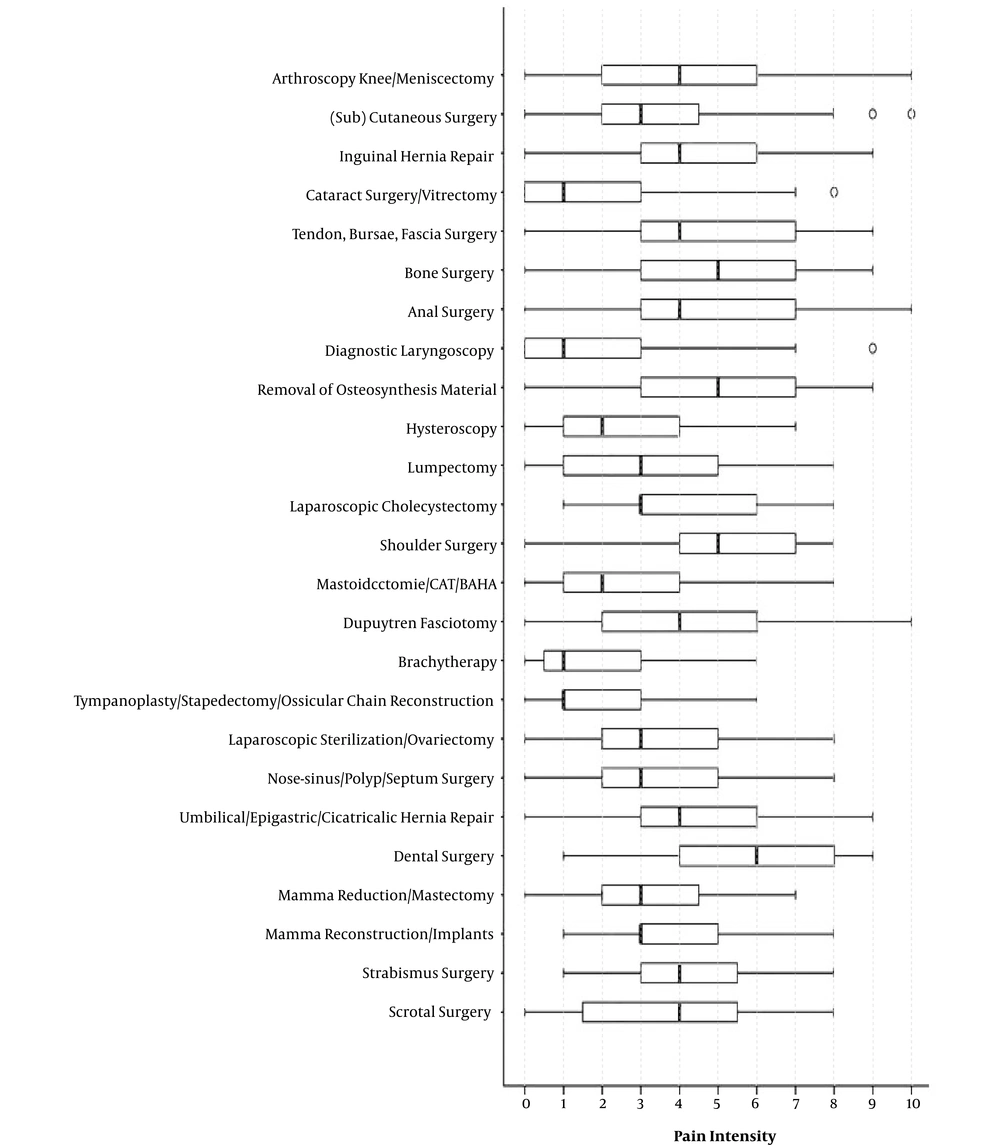
From a total of 1123 patients, 182 patients experienced moderate pain (NRS 4 - 5) (16.3%) and 136 patients experienced severe pain (NRS > 5) (12.1%) on the fourth postoperative day. The number of patients with moderate and severe pain, median pain scores, and median pain interference with daily activities as related to the surgical procedure are presented in Table 2. A high variability was observed in APSP and pain interference between the different surgical procedures. For example, shoulder surgery, anal surgery, and dental surgery were associated with the highest pain scores (median NRS = 4) on the fourth postoperative day. With these types of surgeries, severe pain (NRS > 5) was noted in over 28% of patients. In contrast, ophthalmological procedures, diagnostic laryngoscopy, brachytherapy, and lumpectomy were associated with low pain scores on the fourth postoperative day. For these procedures, median pain NRS-scores did not exceed a score of one and less than 12% of the patients reported moderate postoperative pain (NRS 4 - 5). Pain interference with daily life activities was highest after shoulder surgery and bone surgery, with a median NRS of 7. Box plots showing pain scores on the fourth postoperative day are presented in Figure 2.
| Procedures | N | Moderate Pain | Severe Pain | Pain | Pain Interference |
|---|---|---|---|---|---|
| Arthroscopy knee/meniscectomy | 146 | 36 (25) | 17 (12) | 3 (1 - 5) | 5.5 (3 - 8) |
| (Sub) cutaneous surgery | 76 [1] | 11 (15) | 6 (8) | 2 (0 - 3) | 4 (2 - 7) |
| Inguinal hernia repair | 72 [1] | 17 (24) | 11 (15) | 3 (1 - 5) | 6 (4 - 8) |
| Cataract surgery/vitrectomy | 61 [1] | 1 (2) | 3 (5) | 0 (0 - 1) | 1 (0 - 3) |
| Tendon, bursae, fascia surgery | 57 | 10 (18) | 15 (26) | 3 (1 - 6) | 6 (3.3 - 8) |
| Bone surgery | 57 | 11 (19) | 12 (21) | 3 (1.5 - 5) | 7 (3.5 - 9) |
| Anal surgery | 51 | 8 (16) | 18 (35) | 4 (1 - 6) | 6 (3 - 8) |
| Diagnostic laryngoscopy | 49 | 3 (6) | 3 (6) | 0 (0 - 1.5) | 0 (0 - 3) |
| Removal of osteosynthesis material | 48 | 13 (27) | 7 (15) | 3 (1 - 4.8) | 5 (3 - 8) |
| Hysteroscopy | 47 | 4 (9) | 2 (4) | 1 (0 - 3) | 3 (0.8 - 4) |
| Lumpectomy | 42 [1] | 2 (5) | 0 (0) | 1 (0 - 2) | 3.5 (1 - 6) |
| Laparoscopic cholecystectomy | 41 | 5 (12) | 2 (5) | 2 (1 - 3) | 5 (3.3 - 7.8) |
| Shoulder surgery | 41 | 11 (27) | 12 (29) | 4 (2 - 6) | 7 (5 - 8) |
| Mastoidectomy/CAT/BAHA | 41 | 4 (10) | 2 (5) | 1 (0 - 2) | 1 (0 - 5) |
| Dupuytren fasciotomy | 32 | 7 (22) | 6 (19) | 3 (0 - 4.8) | 6 (3 - 8) |
| Brachytherapy | 32 | 2 (6) | 0 (0) | 1 (0 - 2) | 1 (0 - 3) |
| Tympanoplasty/stapedectomy/ossicular chain reconstruction | 31 [1] | 5 (16) | 0 (0) | 1 (0 - 2) | 1 (0 - 3) |
| Laparoscopic sterilization/ovariectomy | 30 | 4 (13) | 2 (7) | 1 (0 - 3) | 5 (2 - 6.5) |
| Nose-sinus/polyp/septum surgery | 29 | 3 (10) | 5 (17) | 2 (0.5 - 4.5) | 4 (1.5 - 5.5) |
| Umbilical/epigastric/ cicatricalis hernia repair | 26 | 2 (8) | 1 (4) | 2 (1 - 3) | 6 (3.5 - 8) |
| Dental surgery | 24 | 8 (33) | 7 (29) | 4 (2.3 - 6) | 6 (4 - 8) |
| Mamma reduction/mastectomy | 24 | 5 (21) | 1 (4) | 1 (0.3 - 3.8) | 3.5 (2 - 7) |
| Mamma reconstruction/implants | 21 | 3 (14) | 0 (0) | 2 (1 - 3) | 4 (3 - 8) |
| Strabismus surgery | 20 | 2 (10) | 2 (10) | 2 (1 - 2.8) | 4 (1.3 - 7.8) |
| Scrotal surgery | 20 | 5 (25) | 2 (10) | 2 (0 - 4.8) | 3.5 (0.3 - 7) |
Abbreviations: BAHA, bone-anchored hearing aid; CAT, combined approach tympanoplasty.
a Pain is assessed using a Numeric Rating Scale (NRS), range 0 (no pain at all) to 10 (worst pain imaginable). Moderate pain is defined as an NRS of 4 - 5, severe pain as an NRS 6 - 10. Beside pain intensity also pain interference (impact of pain on daily life activities, average of postoperative day 1 - 4) is shown.
b Values represent the number of patients per surgical procedure [missing data], No. (%), or median (25th - 75th percentile).
Pain scores after various surgical procedures on the fourth postoperative day. The box plots indicate worst pain since surgery on a Numeric Rating Scale (NRS) with 0 = no pain to 10 = worst imaginable pain. The 25th and 75th percentiles are indicated by the box edges. The 5th and 95th percentiles are presented by whiskers. The circle indicates outlier.
Univariate logistic regression analysis demonstrated that preoperative pain significantly predicts postoperative pain on the fourth day only after some well-defined procedures of day surgery (Table 3). The overall pooled odds ratio, including all types of surgery, was 4.45 (95% confidence interval 3.38 to 5.86, P < 0.001). For the post-hoc analyses assessing the impact of preoperative pain prevalence, 16 procedures were labeled as “high prevalence” and nine as “low prevalence”. When preoperative pain prevalence was added to the model, the odds ratio for high preoperative pain prevalence was 2.56 (1.75 to 3.73, P < 0.001) and the overall odds ratio of preoperative pain level decreased from 4.45 to 3.37 (2.52 to 4.51, P < 0.001).
| Procedures | Nc | Odds Ratio | CI (95%) | P Value | |
|---|---|---|---|---|---|
| Lower | Upper | ||||
| Arthroscopy knee/meniscectomy | 146 | 4.15 | 1.60 | 10.75 | 0.003d |
| (Sub) cutaneous surgery | 76 [1] | 4.97 | 1.61 | 15.34 | 0.005d |
| Inguinal hernia repair | 72 [1] | 2.32 | 0.88 | 6.12 | 0.089 |
| Cataract surgery/vitrectomy | 61 [1] | 96.83 | 5.85 | 1603.70.48 | 0.001d |
| Tendon, bursae, fascia surgery | 57 | 4.63 | 1.30 | 16.58 | 0.018d |
| Bone surgery | 57 | 3.13 | 0.93 | 10.46 | 0.065 |
| Anal surgery | 51 | 1.56 | 0.50 | 4.90 | 0.448 |
| Diagnostic laryngoscopy | 49 | 20.50 | 2.41 | 174.07 | 0.006d |
| Removal of osteosynthesis material | 48 | 27.27 | 3.17 | 234.93 | 0.003d |
| Hysteroscopy | 47 | 7.20 | 1.13 | 45.96 | 0.037d |
| Lumpectomy | 42 [1] | 7.12 | 0.427 | 118.89 | 0.172 |
| Laparoscopic cholecystectomy | 41 | NC | |||
| Shoulder surgery | 41 | 4.24 | 0.91 | 19.78 | 0.066 |
| Mastoidectomy/CAT/BAHA | 41 | 5.33 | 0.67 | 42.23 | 0.113 |
| Dupuytren fasciotomy | 32 | 6.00 | 1.25 | 28.84 | 0.025d |
| Brachytherapy | 32 | NC | |||
| Tympanoplasty/stapedectomy/ossicular chain reconstruction | 31 [1] | 30.02 | 2.10 | 429.24 | 0.012d |
| Laparoscopic sterilization/ovariectomy | 30 | 1.00 | 0.09 | 11.03 | 1.000 |
| Nose-sinus/polyp/septum surgery | 29 | 0.833 | 0.13 | 5.35 | 0.848 |
| Umbilical/epigastric/cicatricalis hernia repair | 26 | NC | |||
| Dental surgery | 24 | 1.31 | 0.19 | 9.24 | 0.784 |
| Mamma reduction/mastectomy | 24 | 0.39 | 0.04 | 4.15 | 0.436 |
| Mamma reconstruction/implants | 21 | 10.00 | 0.67 | 149.04 | 0.095 |
| Strabismus surgery | 20 | NC | |||
| Scrotal surgery | 20 | 2.20 | 0.24 | 20.40 | 0.488 |
Abbreviations: BAHA, bone-anchored hearing aid; CAT, combined approach tympanoplasty; CI, confidence interval.
a Preoperative pain is defined as average pain over the past week, Numeric Rating Scale (NRS) > 3 (NRS 0 - 10). Postoperative pain is defined as pain at the moment of completing the questionnaire, postoperative day four, NRS > 3.
b NC = not calculable, because of the patients with postoperative pain at day four, all had either pain (Laparoscopic cholecystectomy) or no pain (brachytherapy, umbilical/epigastric/cicatricalic hernia repair, strabismus surgery) at baseline.
c Values represent the number of patients per surgical procedure [missing data, imputed for logistic regression].
d A significance level of P < 0.05 was used.
4. Discussion
The results of the present study indicate that 28.4% of adult patients, which underwent various types of day surgery still experience moderate to severe APSP (NRS > 3). Furthermore, a procedure-related variation in severity of APSP was noted where shoulder surgery, anal surgery, and dental surgery were associated with the highest pain levels.
In line with the second aim of the current study, the researchers observed that preoperative pain is a predictive factor for acute postoperative pain on the fourth day only after certain defined types of day surgical procedures, and that the predictive value showed a procedure-specific variation.
The observed high prevalence (28.4%) of moderate to severe APSP on the fourth postoperative day in the current study was rather unexpected, given the efforts made over the last decades to improve postoperative pain management. These results seem to be conflicting with those reported by Gramke et al. in 2007 (1). They concluded that, since APSP intensity decreases with time, only 14% of patients experience moderate to severe pain levels on the fourth day after day surgery (1). A reasonable explanation for this apparent inconsistency is that the landscape of day surgery is rapidly changing: Because of economical motives, many governments encourage to carry out more complicated and painful surgical interventions and to perform surgery on older and higher risk patients in a day surgery setting (1). Indeed, both patient characteristics and surgical procedure characteristics differed significantly: The population in the present study included more patients with preoperative pain (38.7%) as compared to the previous study (6%) (2). Furthermore, a relatively low percentage of ophthalmological procedures were performed in the present study (7% as compared to 14% previously reported) (2). Ophthalmological procedures are known to be amongst the least painful procedures, and result in lower postoperative pain scores (1). Finally, the proportion of more complex and painful procedures, such as inguinal hernia repair, laparoscopic cholecystectomy, and shoulder surgery was higher in the present study.
Obviously, some procedures are more painful than others. Orthopaedic procedures for instance, are known to cause moderate to severe acute postoperative pain in the vast majority of patients (1, 11, 16, 17). From the data, it could be concluded that shoulder, dental, anal, tendon, bursae, and fascia surgery are associated with the highest pain scores on the fourth postoperative day. These findings may be explained by the assumption that many of these patients already experienced significant preoperative pain, which is often the indication for the operation itself, and by the dense innervation of periost tissue. Furthermore, the high postoperative pain scores after dental procedures are a result of a disproportionately greater sensory nociception in the oral cavity compared to other parts of the human body (18). Remarkably, after some more invasive procedures, such as mamma reconstructions, lower pain levels were reported compared with less invasive procedures, such as anal procedures. Recently, Gerbershagen also demonstrated that many “minor” surgical procedures are associated with higher pain levels on the first postoperative day compared to some major procedures (5). This might be explained by the fact that for more invasive surgical procedures, better perioperative pain management is provided (5).
The second aim of this study was to assess the predictive value of preoperative pain for the development of moderate to severe postsurgical pain after a wide range of surgical procedures. Overall, preoperative pain significantly predicted postoperative pain on the fourth day (OR 4.45). However, the predictive value of preoperative pain shows a procedure-specific variation and is not noted after well-defined procedures, such as anal and scrotal surgery, mamma surgery, laparoscopic sterilization/ovariectomy, dental surgery, and nose or ear surgery. Preoperative pain, in general, is known to be a strong predictor of APSP (7-12). However, the mechanism by which preoperative pain influences postoperative pain is not fully understood. A hypothesis that has been described in the literature involves a process of preoperatively-induced central sensitization of nociceptive spinal dorsal horn neurons due to chronic noxious afferent input from the area, which will be operated upon (9, 10, 19). The preoperative release of inflammatory mediators as well as damage to peripheral nerves in the (later) surgical area, may also lead to a higher sensitivity of local nerve cells, known as peripheral sensitization. Both peripheral and central sensitization are known to underlie hyperalgesia and allodynia (20, 21). In addition to preoperative inflammation-induced peripheral and central sensitization processes, psychological effects, in particular those associated with anxiety for upcoming surgery, may play an important role in postoperative pain experience. (8, 9). Interestingly, the predictive value of preoperative pain shows a clear procedure-specific variation: The association between pre- and post-operative pain varies considerably, depending on type of surgical procedure. An explanation could be that some types of surgery, performed because of significant preoperative pain, are very effective in reducing postoperative pain. It has been demonstrated that this may be the case in women undergoing a hysterectomy because of chronic pelvic pain (22). Another explanation might be that the prevalence of acute pre- or postoperative pain for certain types of procedures may be so low or high, that any association with post- or pre-operative pain fades out. For example, anal surgery is known to be associated with a very high prevalence of APSP and patients for shoulder surgery often have a high level of preoperative pain (5, 23-25). However, a post-hoc logistic regression analysis suggests that procedure-specific variability in impact of preoperative pain level on postoperative pain can only partly be explained by procedure-specific preoperative pain prevalence.
A major strength of this study was that it compared postoperative pain between different procedures rather than between surgical disciplines for day surgery. Another strength was that only surgical procedures containing at least 20 procedures were analysed. A more complete picture of postoperative pain as well as the relationship with different procedures within the same specialty may result in superior pain treatment at home by promoting the implementation of procedure-specific pain-protocols (5, 26).
There were several limitations in the study design. First, the researchers only analysed APSP in surgical patients treated at one single hospital of the Netherlands. Therefore, the generalizability of the results can be questioned since cultural influences on pain perception might affect and interfere with the results as presented in this study (27). Second, the results are based on a questionnaire-survey with a response ratio of 51% for the baseline and follow-up questionnaire. This might result in a selection bias, although the response ratio is comparable to other questionnaire-based surveys (28). Third, some similar or closely related surgical procedures were combined in a surgical group to create groups of at least 20 patients to make comparison of pain outcomes after various types of surgery, statistically meaningful. Finally, some surgical procedures could not be included in the analysis due to the small number of patients, which resulted in very large confidence intervals.
4.1. Conclusion
In conclusion, as the prevalence of moderate to severe APSP at home is high four days after day surgery and as a strong relationship between preoperative pain and postoperative pain exists after well-defined procedures of day surgery, future studies should focus on the efficacy of a more extensive follow-up after day surgery per individual surgery type.