1. Background
A migraine is a primary headache disorder characterized by severe, recurrent, unilateral, and pulsating headaches that last for four to 72 hours, which is associated with nausea and/or vomiting, photophobia, and phonophobia. Diagnosis of migraine is based on history and examination, although additional testing to rule out secondary headache disorders may be needed in presence of red flags (1, 2). Migraines have serious socioeconomic and personal health impacts. In 2010, the Global Burden of Disease Study, ranked migraines as the third most prevalent disorder in the world. Later in 2015, it was ranked the third-highest cause of disability worldwide in both males and females under the age of 50 years (3). Migraines have a high prevalence with a rate of 14.9% in the United States, and 8.4% to 12.7% in Asia (4). The 1-year prevalence of migraines in the Iranian general population was 27.6% (36.7% in women and 21.6% in men) (5).
Currently, non-steroidal anti-inflammatory drugs and combination analgesics containing paracetamol, ergotamine, or triptans are some of the common pharmaceutical options for management of acute migraine attack (6-8). However, there are some limitations in these therapies including patient’s intolerance due to potential side effects of drugs, contraindications such as pregnancy or breastfeeding or specific medical conditions and limitation of efficacies (1). Due to the limitations associated with these treatments, there is a growing interest in effective low-risk non-pharmacological interventions. Acupuncture is a method of traditional Chinese medicine with a history of over 2500 years. The procedure is to insert thin needles into specific points along energy meridians, which are called acupoints (9). Acupuncture has been utilized as a routine remedy in migraines in China for years and was suggested as an complementary or an alternative treatment for headaches by the National Institutes of Health in 1998 (6). The mechanism of acupuncture is not fully clarified yet and different mechanisms have been proposed. Some studies revealed that acupuncture could stimulate different types of afferent fibers, which cause inhibition in pain transmission within the central nervous system (10, 11). It also eases the release of some pain suppressors including opiate chemical substances (such as endorphin), serotonin, dopamine, neurotrophins, and nitric oxide in the central nervous system (9). This method also decreases serum matrix metalloproteinase-2, which causes relief in migraine headaches (6).
2. Objectives
There were studies using this method and in most, the effect of acupuncture on preventing migraine attacks has been investigated. In those several studies that surveyed the effect of acupuncture on the treatment of migraine headaches, the conclusion was not completely persuaded and they suggested further researches on this topic. The purpose of this study is to examine the effect of acupuncture on controlling acute migraine attacks.
3. Methods
3.1. Study Design
This study was a single blinded randomized clinical trial that was conducted from March 2015 until May 2016 at Imam Khomeini Hospital Complex, Tehran, Iran. The study protocol was approved by the Ethical Committee of Tehran University of Medical Sciences and investigators were adhered to the Declaration of Helsinki throughout the study. Patients enrolled after receiving a signed informed consent.
3.2. Study Population
The patients with diagnosis of acute migraine attack, aged between 18 to 65 years, were eligible. Those with a decrease in consciousness level, focal neurological symptoms, anti-convulsions or painkiller consumption in 24 hours before referral, and women during their menstruating period were excluded.
The diagnosis of a migraine was confirmed by an expert neurologist based on the international classification of headache disorders 3rd edition and patients who fulfilled the criteria were classified as migraine patients.
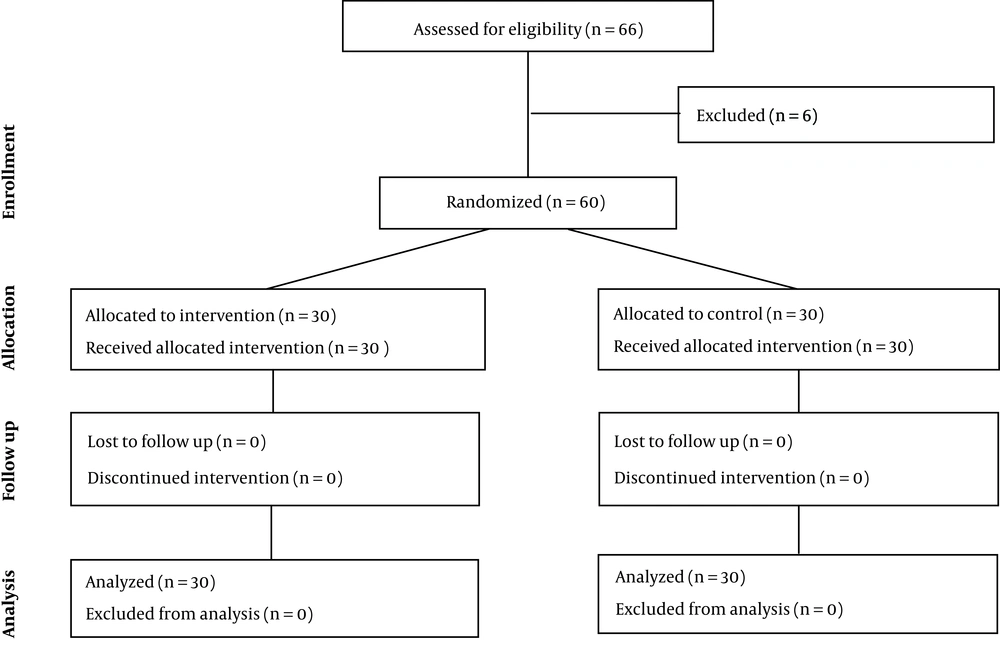
Considering α = 0.05, power of 90%, and using the formula below the sample size calculated as 10 in each group. Taking possible 200% error sample size, finally 30 patients enrolled in each arm of the study.
Sampling was performed in convenient methods. In collaboration with a faculty member of the Imam Khomeini Hospital neurologist, at first, known cases of migraines referred to the headache clinic in Imam Khomeini Hospital were detected and after speaking with them on the phone and taking informed consent on the condition of acceptance, they were selected.
By using the four block method of randomization, patients were divided into two groups: Group A in which patients received actual acupuncture and group B in which patients took acupuncture-placebo. Then, these two groups were classified to six subgroups according to the rolling a dice method (block randomized). The patients and the investigator who had a responsibility for checking the pain score were blinded to the type of acupuncture.
3.3. Data Gathering and Intervention
At the time of reference, the patient’s pain intensity was measured based on visual analogue scale (VAS) and recorded in a written checklist. Thereafter, 15, 30, 45, and 60 minutes after acupuncture and also on two, three, and four hours after intervention, the pain intensity was also asked and compared with the reference time’s score.
Acupuncture was done with sterile metallic needles (made by Huan-Qiu®) with a width of 0.25 mm and length of 13 mm, which enter certain points in the ear’s skin. Ear acupoints associated with pain relief in migraine headaches are shen men, autonomic, thalamus, frontal, and temple (Figure 1). In the placebo group, similar needles were used, however, they were inserted into inappropriate acupoints such as stomach, spleen, etc. Proper information regarding the appropriate versus inappropriate acupoints are available in they studies of Romoli et al. and Allais et al. (12, 13).
In terms of pain management, decreasing of at least 13 mm in VAS was considered significant; although 30 mm would be clinically acceptable. Therefore, if any patients pain score did not decrease by at least 30 mm, they were considered as nonrespondent and were given rescue medicine. For those patients who did not have proper relief in pain 10 minutes after treatment, dexamethasone injection was done as a rescue medicine. The rescue medicine was chosen and prescribed by the neurologist advisor of the project.
After four hours of monitoring the patients, they were followed over the next 24 hours with a telephone and were examined in terms of severity and recurrence of headaches that need painkillers. All procedures were performed by one operator who had been trained during 1-month course prior to sampling.
3.4. Statistical Analysis
The gathered data were entered to a pre-designed excel sheet. Then, STATA-11 software was used for analysis. To describe the findings, descriptive statistics including mean ± standard deviation (SD) or frequency and percentage were used. Paired t-test was used for analytical analysis and P value < 0.05 was considered as significant level.
4. Results
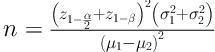
A total of 60 patients with the mean age of 31.4 ± 7.6 years were enrolled and 50 cases (83.3%) of them were women. CONSORT diagram of patients’ flow has been shown in Figure 2. Of the 66 eligible patients, six cases were excluded (one in the absence of acute migraine attack on admission, two had acupuncture fears, and three were on their menstruating period).
Based on the findings there were no significant differences between two groups in terms of the baseline characteristics of participants including age, sex, and pain duration before admission (P > 0.05).
Table 1 shows the mean ± SD of the pain score in various checkpoints. According to the results, there was a significant difference between the two groups on the checkpoints of 15, 30, 45, and 60 minutes after acupuncture; however, the pain scores were not statistically different between the two groups on two, three, and four hours after intervention (P > 0.05).
| Checkpoint | Group | P | |
|---|---|---|---|
| Intervention (n = 30) | Placebo (n = 30) | ||
| At reference | 7.3 ± 1.5 | 6.4 ± 1.9 | 0.673 |
| After 15 minutes | 5.2 ± 1.6 | 5.6 ± 1.9 | 0.039 |
| After 30 minutes | 3.1 ± 2.0 | 2.2 ± 3.3 | 0.043 |
| After 45 minutes | 1.2 ± 1.7 | 1.6 ± 1.6 | 0.018 |
| After 1 hour | 0.6 ± 1.5 | 0.9 ± 0.4 | 0.002 |
| After 2 hours | 0.2 ± 1.1 | 0.0±0.2 | 0.136 |
| After 3 hours | 0.2 ± 1.1 | 0.0 ± 0.0 | 0.227 |
| After 4 hours | 0.2 ± 1.1 | 0.0 ± 0.0 | 0.227 |
Of the 30 patients in intervention group, 28 were completely painless at the end of the 4th hour. In the placebo group, 24 patients did not feel well within the first 10 minutes, and rescue medicine was started for them. Five patients had two score decreases in the first three minutes, however, due to the lack of recovery after 10 minutes, they asked for rescue medicine. One person felt pain relief during the first hour, however, after two hours due to the recurrence of pain, she asked for rescue medicine.During next 24 hours follow up, only one person from the intervention group suffered recurrence that cause analgesic consumption. On the other hand, headache recurrence in 13 patients of the control group lead to analgesic consumption.
5. Discussion
In our study, there was a decrease in pain intensity 15, 30, 45, and 60 minutes after the treatment in both acupuncture and placebo groups with a significant difference between the two groups. However, this difference was not found after two, three, or four hours. Comparison of the two groups showed no differences between acupuncture and placebo acupuncture on decreasing the pain score. A study was conducted by Linde et al., in 2005, on 320 patients with migraines to investigate the effectiveness of acupuncture in comparison with sham acupuncture and with no acupuncture in patients with migraines. It concluded that acupuncture reduced migraine headaches in comparison with no treatment. However, there was no significant difference in reduction of headaches between acupuncture and sham acupuncture, which was similar to our study (14). Another study by Yang and Liang in 2009, which measured VAS scores at 0.5, one, two, and four h after the acupuncture treatment among 180 patient suffering from migraine headaches also showed no significant benefit of verum versus sham MA. However, the effect of both methods was the same as our study and both methods decreased the intensity of pain (15).
Most of the studies that aimed to compare verum acupuncture versus sham acupuncture had different results from our study. By instance, in a study in 2012 done by Wang et al., on 150 patients, the efficacy of verum and sham acupuncture on migraines was examined. They found out that it is possible to apply acupuncture in treatment of acute migraine for pain relief and it also prevents relapse. The study also showed that verum acupuncture is more effective than sham acupuncture in reducing the pain severity, the number of patients with acute medications usage, and the accompanying symptoms (16). Another study in 2012 conducted by Wallasch et al., was done to investigate the prophylactic effect of acupuncture on 35 individuals with migraines. The patients were divided into two verum and placebo-acupuncture groups. The study showed a significant decrease in days with migraine headache in the verum group in comparison with the placebo-acupuncture group (17). A study by Allais et al., in 2011, aimed to compare the effect of ear acupuncture in appropriate acupoints versus inappropriate acupoints in patients with migraines. It was done on 84 patients with migraines who were put into two groups of appropriate and inappropriate acupoints. The study demonstrated that compared with inappropriate points, appropriate points are more efficacious in controlling any type of pain, including pain of migraine headaches. It also showed that the antitragus area appears to be more appropriate than the representation of the sciatic nerve for reducing the severity of migraine attacks. The study suggested that there are more areas to be treated with ear acupuncture to achieve a real prophylactic effect in migraine (13). As mentioned above, contrary to our study, most studies have showed that acupuncture on acupoints is more effective than on inappropriate points.
The comparison of these studies shows that there are still lots of controversies in effectiveness of acupuncture treatment on acute migraine attack. Although method of studies, sample size, data gathering, blinding system, and all other interfering items were almost similar in these studies, the results were different.
5.1. Limitation
Pain relief is found in both groups and the researcher attributes it to psychological effects. If a control group, without acupuncture treatment, were also studied along with these two groups, a better conclusion could be made.
5.2. Conclusions
Based on the findings of our study, although the pain score was lower in the intervention group than the control group during the first hour after the acupuncture, there was no significant change in pain score thereafter. The comparison of two groups showed no differences between acupuncture and placebo acupuncture on decreasing the mean pain score. These results may be due to the psychological effects of acupuncture and not for its physiological effects. As mentioned above, the pain intensity was decreased in both groups which can be due to the patient’s positive expectation of conventional medicine such as acupuncture and entering a needle itself made them feel relieved of pain. If there was a physiological effect, then the results must be different between two groups. Due to the fact that acupuncture has lower side effects and fewer contraindications and due to the patient’s tendency to conventional medicine, we concluded that acupuncture can be used in combination with medical treatments in treatment of migraine headaches.