1. Background
Spinal epidural lipomatosis (SEL) is a rare disease, defined as diffuse hypertrophy of unencapsulated adipose tissue causing spinal canal compression and progressive neurologic deficits. Posterior epidural adipose tissue has been characterized as physical functional tissue that provides a sliding space. However, an excessive amount of adipose tissue in the epidural space can itself have a compressing effect and may lead to back and leg symptoms.
SEL patients may present with progressive and longstanding complaints of back pain, radiating leg pain, neurogenic claudication, decreased pinprick sensation, and rarely lower extremity weakness (1). It is frequently associated with exogenous steroid use, obesity, endogenous steroid excess, or Cushing’s syndrome. Since the first report of SEL in 1975 in a kidney transplant patient by Lee et al. (2), other cases of the disease have been reported. Recently, the prevalence of SEL was reported to be between 2.5% and 25% as magnetic resonance imaging (MRI) became more common (1, 3-6). SEL diagnosis methods include myelography, postmyelography computed tomography (CT), and MRI. The gold standard is T1-weighted MRI, and axial and sagittal images can show hyperintense epidural mass. T2-weighted images show intermediate intensity (7); fat suppression is the definitive diagnosis method.
SEL is known to occur mainly in men, mostly at the thoracic level, and is diagnosed at the 6 - 8th dorsal thoracic level when the extradural fat thickness is 7 mm or more. Cervical levels are rare and lumbar level is the single most frequently affected region (1). SEL can be idiopathic or secondary. Idiopathic SEL has been documented in association with cases without corticosteroid use or endocrine disorders. The differential diagnosis includes subacute epidural hematoma, spinal angiolipoma, epidural metastasis, and epidural abscess (1).
2. Objectives
However, there are few studies on SEL in Korea. The purpose of this study was to access the prevalence and clinical characteristics of SEL diagnosed by lumbar spine MRI performed in a single hospital.
3. Methods
The study was designed as a retrospective investigation of the lumbar spine MRI performed at this hospital. After obtaining approval from our institutional review board (2018-03-009), of the 3702 patients (1575 males and 2127 females) who underwent lumbar spine MRI at the age of 20 years or older from January 2014 to December 2016, 42 patients (27 males and 15 females) diagnosed with SEL were selected. Medical records and telephone counseling were used to document sex, age, height, weight, clinical symptoms (i.e., low back pain, radiating leg pain, and weakness), coexistent spinal disease (i.e., spinal fracture, spinal stenosis, herniated disc disease, spondylitis, and spondylolisthesis), affected spine level, concomitant diseases (i.e., hypertension, diabetes, liver disease, kidney disease, lung disease, thyroid disease, and Cushing’s syndrome), and alcoholism and smoking status.
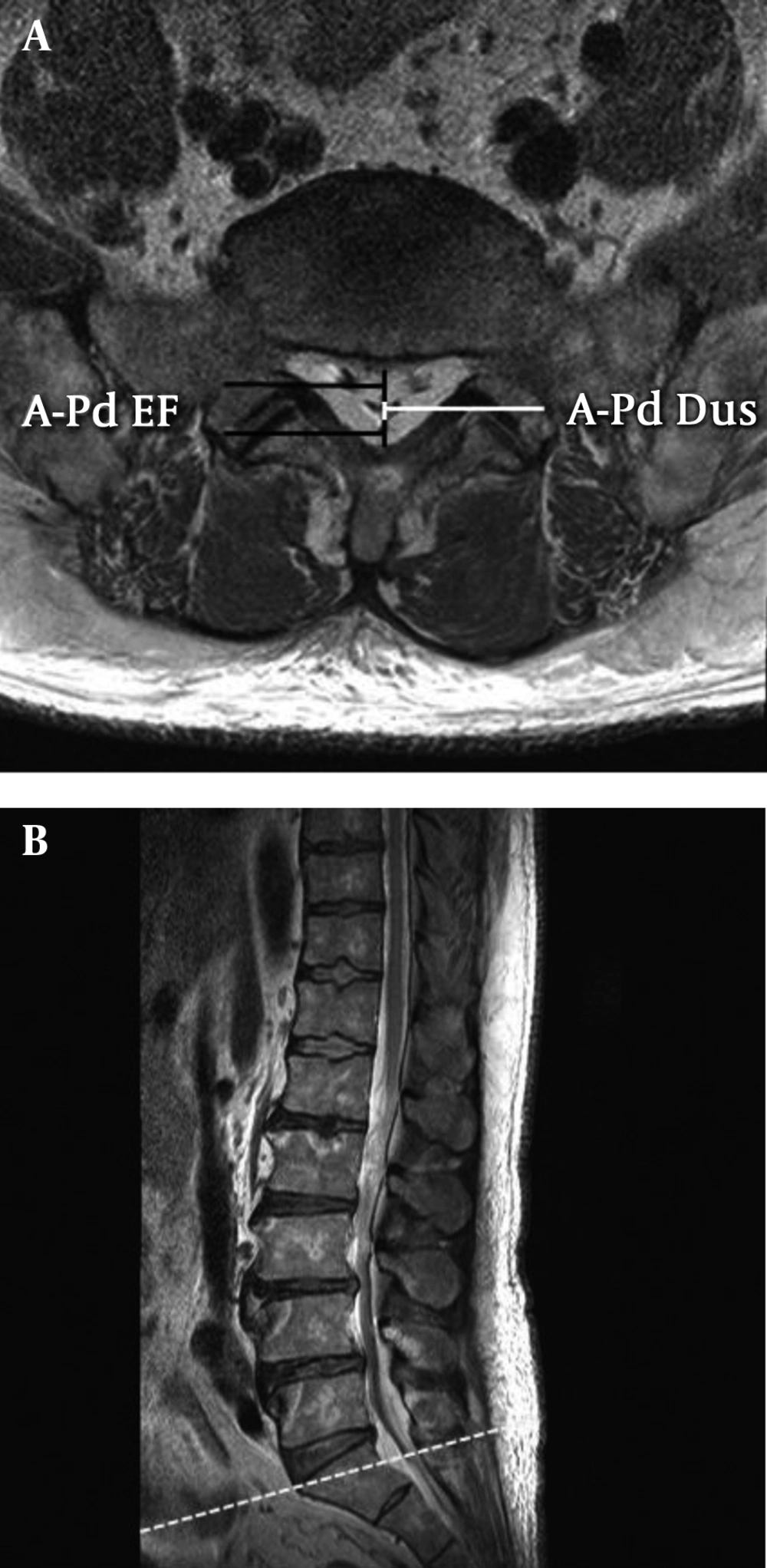
One radiologist classified the severity of epidural lipomatosis into three grades ranging from I to III using dura sac according to Borre et al. (6). We obtained four linear measurements at the axial plane parallel based in the narrowest on MRI image. We calculated (A) DuS/EF index and (B) EF/Spi C index.
SEL grade I: DuS/EF index 1.49 - 1, EF/Spi C index 41% - 50%;
SEL grade II: DuS/EF index 0.99 - 0.34, EF/Spi C index 51% - 74%;
SEL grade III: DuS/EF index ≤ 0.33, EF/Spi C index ≥ 75%.
A-Pd Dus: Antero-posterior diameter of the dural sac, A-Pd of EF: Antero-posterior diameter of epidural fat, DuS: Located ventrally and dorsal to the dural sac, and Spi C: Antero-posterior of the spinal canal.
The data are presented as mean ± standard deviation or number %. A t-test was used to analyze the parametric data within each group.
4. Results
In this retrospective analytic study, 42 patients (27 males and 15 females) were enrolled. The incidence of symptomatic SEL in the lumbar spine was 1.1%, which was 1.71% for men and 0.7% for women. Demographic data were compared between men and women (Table 1). The mean age of the patients was 69.4 ± 10.9 years; age in men was significantly lower than in women. The mean body mass index (BMI) was 26.4 ± 3.5 kg/m2, and there were no significant differences between men and women. BMI above 30 kg/ m2 was observed in two male and two female patients.
The most common clinical symptom was lower back pain and radiating leg pain (26 patients, 61.9%), followed by lower back pain (12 patients, 28.5%), leg pain (2 patients 4.7%), and weakness (2 patients, 4.7%). Coexistent spinal diseases included spinal fracture (15 patients, 35.7%), spinal stenosis (15 patients, 35.7%), herniated disc disease (6 patients, 14.2%), spondylitis (4 patients, 9.5%), and spondylolisthesis (2 patients, 4.7%).
The most frequently affected levels were found to be L5 - S1, L4 - L5, L3 - L4, and L2 - L3 (Table 2). Accompanying diseases were hypertension, diabetes, hepatic diseases, renal diseases, and pulmonary diseases (Table 3). Thyroid disease and Cushing's syndrome were each found in two patients. BMIs of the patients with Cushing's syndrome were 26.5 (Borre grade I) and 26.4 kg/m2 (Borre grade II). There were 16 patients who consumed alcohol and 14 patients who smoked.
| The Affected Level | No. (%), Total = 42 |
|---|---|
| L2 - L3 | 2 (4.8) |
| L3 - L4 | 9 (21.4) |
| L4 - L5 | 10 (23.8) |
| L5 - S1 | 21 (50) |
The Level of Affected Spinal Epidural Lipomatosis
| Variables | No. (%) |
|---|---|
| Hypertension | 26 (61.9) |
| Diabetes mellitus | 12 (28.5) |
| Hepatic disease | 7 (16.6) |
| Renal disease | 6 (14.25) |
| Pulmonary disease | 4 (9.5) |
Accompanying Diseases of Spinal Epidural Lipomatosis Patients
The most common SEL grade was type III (21 patients, 50%), followed by type II (17 patients, 40.4%) and type I (4 patients, 9.5%). In men, type III (15 patients, 55.6%) was the most common followed by types II (17 patients, 37%) and I (4 patients, 9.5%). In women, type II (7 patients, 46.7%) was the most common, followed by types III (6 patients, 40%) and I (2 patients, 13.3%).
5. Discussion
In our study, the prevalence of symptomatic SEL in lumbar spine MRI was 1.1%, and SEL was most common at the L5 - S1 level, and grade III was the most common type. The disease was more common in male patients.
In this study, the prevalence of the disease (1.1%) was lower than other studies. The reason for this result is that in our study MRI was performed mainly in patients with back pain and leg pain. Recently, Theyskens et al. (1) classified SEL as incidental SEL (without any spine related symptoms), SEL with spine related symptoms, and symptomatic SEL (symptoms specific to SEL). According to their classification, SEL in this study is similar to SEL with spine related symptoms; they also showed a prevalence of about 1.8%, which is similar to our finding.
Back and leg radiating pain was the most common clinical symptom of the patients, but it is difficult to speculate that it is caused by SEL alone considering the coexistent spinal diseases. In this study, MRI showed many cases of fracture, but the cause of this phenomenon is not known. SEL was most prevalent at L5 - S1, which is similar to other studies (7).
The etiology of SEL is not completely understood yet. Previously, long-term exogenous steroid use, epidural corticosteroid injection, metabolic diseases such as Cushing’s syndrome and hypothyroid disease, obesity, and male gender were known as the risk factors for SEL (8, 9). We tried to find out the relationship between known risk factors and SEL, but the number of patients was insufficient to obtain statistically significant results. This study was similar to other studies with regards to the higher prevalence of the disease in men (64%) and patients’ mean age (69.4 ± 10.9 years). However, BMI was 26.4 ± 3.5 kg/m2, which is lower than other studies (1).
We found that hypertension was the most prevalent disease along with diabetes, hepatic disease, and pulmonary disease (1). The frequency of alcohol consumption was high in this study similar to other studies (9). Smoking has not been reported in previous studies and thus further work is needed. It has recently been shown that these diseases and lifestyle can affect lipid metabolism and can be involved in the development of idiopathic SEL (10).
SEL grading was based on axial images by evaluating the morphologic appearance of the dural sac and by assessment of the obliteration of the cerebrospinal fluid space in front of the cauda equina according to Ishihara et al. (10). Borre et al. (6) used dural sac, epidural fat, and spinal anteroposterior diameter to divide SEL into three grades ranging from I to III. In the case of severe SEL, the thecal sac is small and oval or Y-shaped in the axial image (Figure 1). Based on Borre et al.’s method, type III (50%, 21 patients) was the most common type in our patients, which was not similar to Borre et al.’s study (6). They reported that patients with EF/Spi C of ≥ 75% (type III) exhibited neurological symptoms such as neurological claudication and cauda equina syndrome.
As of yet, no definitive treatments have been reported for SEL (3, 11). Treatment of SEL ranges from conservative management to surgery. Conservative care includes medication therapy, weight reduction, and activity modification. Nonsteroidal anti-inflammatory drugs (NSAIDs) and opioids can be administered in these patients (8, 9, 12). Surgical decompression is performed when paraparesis, urinary retention, or neurologic deficit are severe or if the patient cannot stop steroids (12).
Our findings are inconclusive as it was a retrospective study conducted in only one hospital. Because of the limited number of patients, our findings are not generalizable. Further studies with larger sample sizes are needed in the future.
In conclusion, lumbar spine MRI showed that the incidence of symptomatic SEL was 1.1%; SEL is more common at the L5 - S1 level and in male patients, and severity grade is often severe.