1. Background
For relieving post-surgical pain, many patients and clinicians do not only rely on drugs yet also use non-pharmacological methods (NPMs). There is a large variety of NPMs that are supposed to help reduce pain. However, despite their frequent recommendation, only limited data on actual clinical use of NPMs is available. The aim of this observational study was hence to obtain a broad overview on the frequency of use and the effect of NPMs for post-surgical pain relief.
Non-Pharmacological Methods can be divided to four main groups:
1. Passively applied physical approaches, such as acupuncture, massage, transcutaneous electrical nerve stimulation (TENS), heat or cold packs.
2. Physical activities like walking, deep breathing or light to moderate sportive activities.
3. Psychological/spiritual approaches, such as praying, imagery, visualization, relaxation or meditation.
4. Distractions, like watching TV, listening to music or talking to people.
Use of NPMs for chronic pain is well-documented in the literature. However, little is published on the use of NPMs for post-surgical pain. Most articles focus on one or a few methods for very specific patient cohorts.
Group 1 (passively applied physical methods): The NPMs of this group were considered to be partly effective. Madsen et al. showed acupuncture’s (small) analgesic effect (1). However, they stated that the effect was not clinically relevant and that it might just be a bias. This is supported by Lee and Ernst’s study, which compared several systematic reviews and concluded that evidence is insufficient for acupuncture in surgical settings (2). For TENS, a recent meta-analysis showed improvements in pain intensity with a necessary number to treat for 50% pain reduction of 2.5 (3). Koc et al. proved that ice packs reduce postoperative pain after hernia surgery (4). On the other hand, patients, who had undergone exploratory laparotomy, did not benefit from cold therapy (5). In addition, cold packs were not more effective than pressure bandages for pain after total knee replacement (6, 7).
Group 2 (physical activities): No literature about methods from this group of NPMs for post-surgical pain was found.
Group 3 (psychological/spiritual approaches): The effect of this approach seems to be rather doubtful. Although some patients pray, the pain-easing effect seems to be poor (8). Guided imagery does not alter pain levels in total joint arthroplasty patients (9). Meditation, however, reduced pain levels in noxious situations by 40% after four days of meditation training (10).
Group 4 (distraction): Distraction can have analgesic effects, even additive to placebo treatment (11). Music can reduce acute post-surgical pain by about 0.5 on a 0 to 10 scale (12). Older patients also benefit from music after cancer surgery (13).
2. Objectives
The current analyses aimed at assessing frequency and effects of NPM use in daily routine by means of a large acute pain registry (the PAIN OUT project). These were the researcher’s main objectives:
• How often are different types of NPMs used?
• Does gender or age influence the frequency NPMs use?
• Is the use of specific NPMs associated with differences in patient-reported pain relief?
• Is NPM use associated with patients’ wish for more pain treatment?
3. Methods
3.1. The Acute Post-Operative Pain Registry PAIN OUT
The data used for this article was collected in the PAIN OUT study (14) (improvement in postoperative pain outcome, www.pain-out.eu, short: PO), a registry project initially funded within the 7th Framework Program of the European Commission. PAIN OUT is an international project with over 100 participating hospitals worldwide and over 60000 patient data sets (as of January 2018). It is registered with Clinical Trials.gov Identifier: NCT02083835.
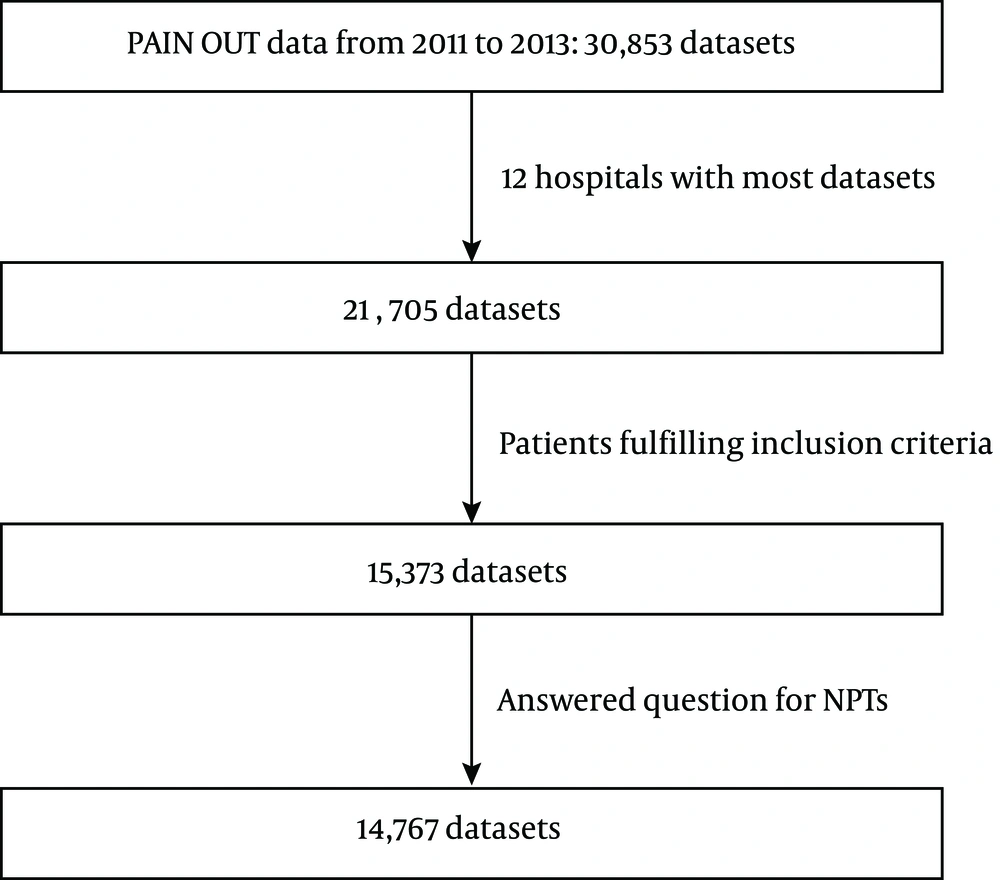
For this study, the researchers selected 12 hospitals with most data sets in order to decrease site-specific variation. These hospitals are located in France, Germany, Italy, Israel, Romania, Spain, Sweden, Switzerland, and the United Kingdom. The PAIN OUT study was approved by the IRB of Jena University Hospital (Reference number 2723/12-09) and all sites obtained approval for the PO study by their respective review boards/ethics committees. Informed consent was obtained from all subjects. The data used for this article was collected in the years 2011 to 2013.
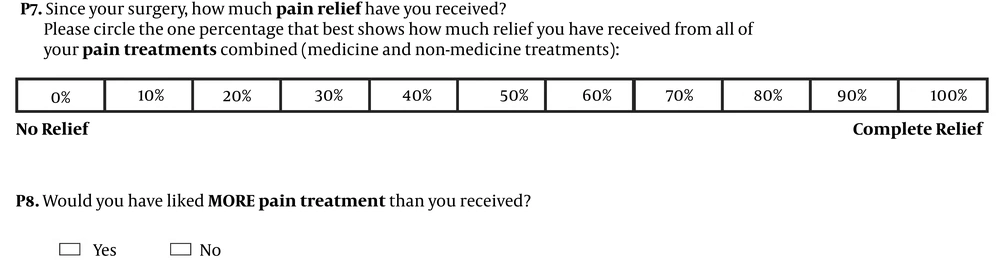
In PO, hospitalized patients were included if they were 18 years or older and were willing and able to participate. Upon participation, patients filled in the so-called international pain outcomes questionnaire IPO (15) in their respective language on the first day after surgery. This validated patient outcomes questionnaire is based on the Revised American Pain Society Patient Outcome Questionnaire (16). It includes a question about pain relief a patient has experienced and a question on whether the patient would have liked more pain treatment (Figure 1). The pain relief question had 11 categories in 10% - steps that defined the percentage of pain relief from 0% to 100%. The wish for more pain treatment question can be answered with “yes” or “no”.
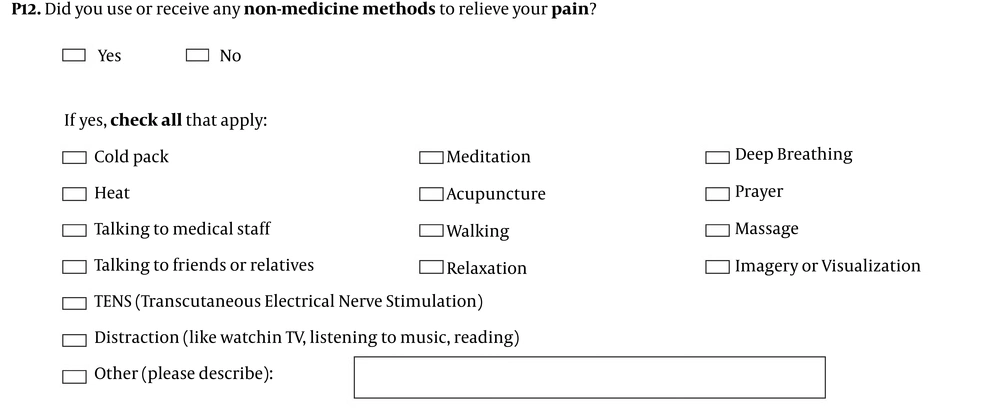
The use of NPMs was obtained by asking the patients if NPMs were applied for them since surgery, and the type used (Figure 2). The methods were thus not distributed randomly for patients. Instead, the patients reported NPMs they intentionally used on their own as well as methods that were applied/prescribed by the medical staff.
In addition to patient-reported pain outcomes, data on demographics (year of birth, gender, country of birth, weight, height, and questionnaire language), surgery type (ICD coding) and duration, co-morbidities, and analgesics (route, type, dosage) was collected in PAIN OUT. After the data was collected, it was anonymized and entered in a registry using a web mask.
3.2. Statistical Methods
First, the researchers analyzed how often different NPMs had been used. Then, they examined if there was an association between using NPMs and pain-related outcomes (pain relief and wish for more pain treatment). For this purpose, the researchers tested the pain relief variable (numerical rating scale from 0 to 10) for normal distribution. The Kolmogorov-Smirnov test with a Confidence Interval (CI) of 0.95 showed that pain relief is not normally distributed (P < 0.001). Hence, the researchers used Mann-Whitney U tests (CI = 0.95) and Kruskal-Wallis tests (CI = 0.95). For the dichotomous variable, “wish for more pain treatment”, the study used Pearson Chi-Square.
Gender and age have an impact on several variables of post-operative pain (17). However, their association with perceived pain relief and wish for more pain treatment has not been studied. The current study investigated this aspect by applying a general linear model to pain relief and logistic regression to the wish for more pain treatment (CI = 0.95). The study calculated models using age, gender, and NPMs as predictors. For logistic regression, the researchers applied forward stepwise and backward stepwise procedures, using likelihood-ratio tests to obtain the final model.
In the final step, variability in the cohort was decreased by filtering for patients with the three most frequent surgeries in PAIN OUT. These surgeries were laparoscopic cholecystectomy (ICD 51.23), total hip replacement (ICD 81.51), and total knee replacement (ICD 81.54).
The researchers used IBM Statistics SPSS 22.0.0 for the statistical analysis.
4. Results
See Figure 3 for information of included and excluded patient data sets. Overall, 14 767 patients answered the question for NPMs. Furthermore, 7 768 (52.8%) were female and 6 953 (47.2%) were male. Forty-six patients had missing gender information. Mean age of the patients was 54.5 ± 17.1 years with a median of 56 years. Eighty-eight patients had missing age information.
Women use NPMs significantly more often (Table 1) than men (P < 0.001). However, if patients use NPMs, neither pain relief (P = 0.225) nor wish for more treatment (P = 0.46) show significant differences between genders. Elderly patients used NPMs significantly less than younger cases (P < 0.001). Elderly had a significantly higher pain relief than younger patients (without NPMs: 73.3% ± 28.3% versus 69.0% ± 27.2%, P < 0.001; with NPMs: 69.7% ± 26% versus 67.6% ± 25.4%, P < 0.001) and a significantly lower wish for more pain treatment (without NPMs 11.6% versus 15.7%, P < 0.001; with NPMs: 13.4% versus 15.8%, P = 0.006).
| NPMs Used | Men | Women | < 56 Years | ≥ 56 Years |
|---|---|---|---|---|
| No | 3994 (57.4) | 4190 (53.9) | 3819 (53.5) | 4348 (57.6) |
| Yes | 2959 (42.6) | 3578 (46.1) | 3315 (46.5) | 3197 (42.4) |
aValues are expressed as No. (%).
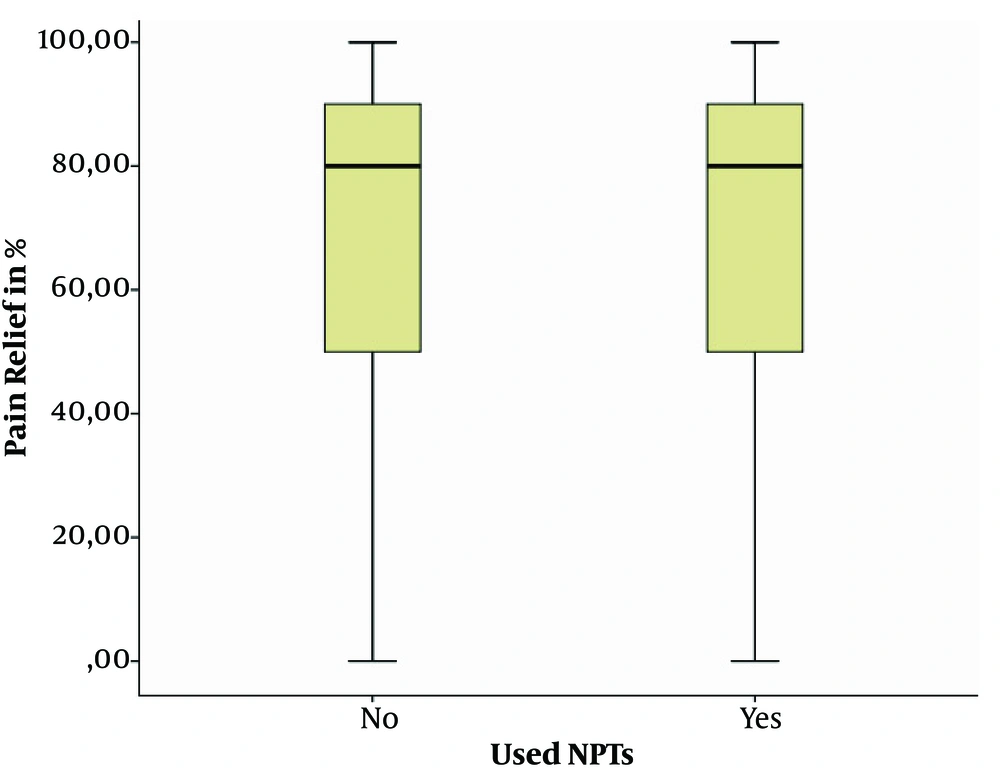
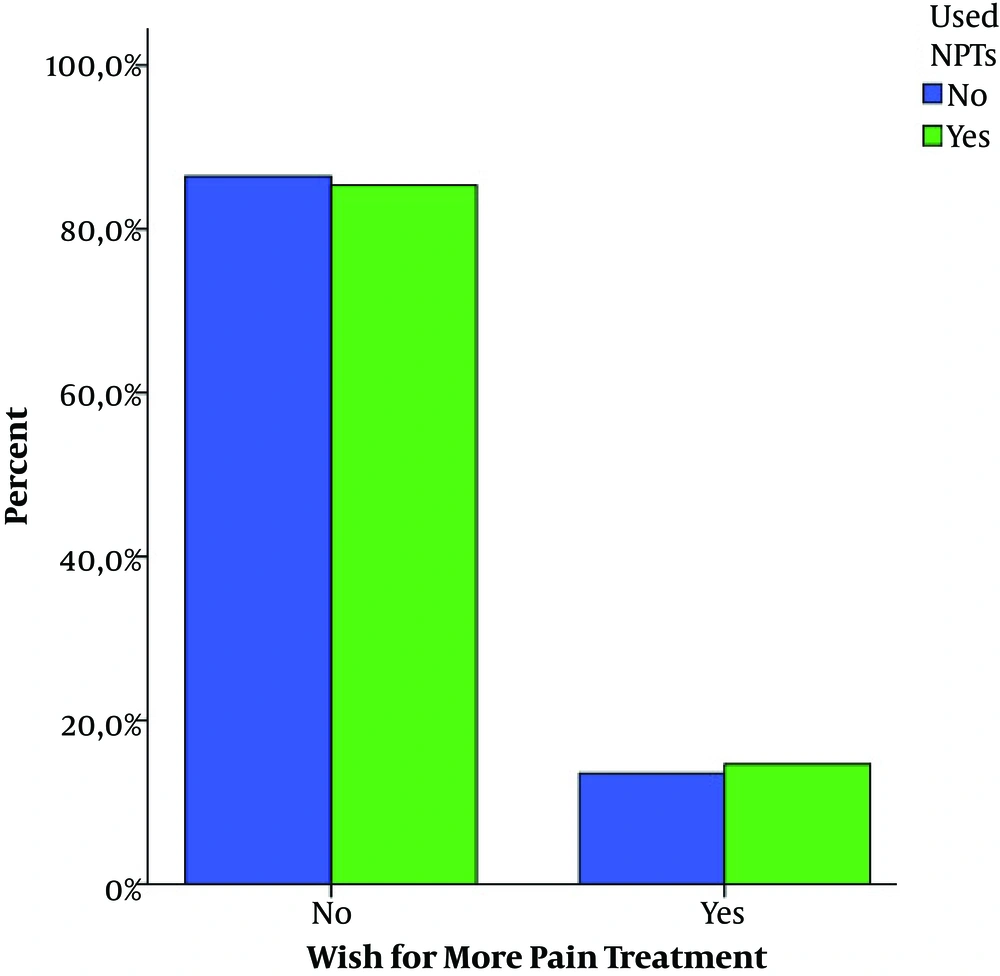
Overall, 6563 (44.4%) patients used at least one NPM while 8204 (55.6%) did not. Overall, patients, who did not use NPMs had little yet significantly more pain relief than patients, who used them (means 71.2% ± 27.9% versus 68.6% ± 25.7%, P < 0.001, Figure 4). The difference in the percentage of patients over all NPMs, who wished for more pain treatment was not significant (Figure 5). Tables 2 and 3 present the usage of every single NPM method and its effect on outcomes.
| Method | No. of Not Used | No. of Used | Pain Relief if Not Used in % | Pain Relief if Used in % | P Value |
|---|---|---|---|---|---|
| Acupuncture | 13294 | 27 | 70 | 59.3 | 0.037 |
| Cold pack | 10795 | 2526 | 70.5 | 67.8 | 0.000 |
| Distraction | 10112 | 3209 | 70.4 | 68.8 | 0.000 |
| Deep breathing | 12466 | 855 | 70.1 | 68.1 | 0.000 |
| Heat | 13025 | 296 | 70.1 | 65.4 | 0.001 |
| Imagery | 13114 | 207 | 70 | 69.6 | 0.367 |
| Massage | 13124 | 197 | 70 | 65 | 0.003 |
| Meditation | 13092 | 229 | 70 | 66.4 | 0.019 |
| Music | 13321 | 70 | . | ||
| Prayer | 12752 | 569 | 70.1 | 67.6 | 0.005 |
| Relaxation | 12712 | 609 | 70.1 | 67.3 | 0.000 |
| Walking | 12700 | 621 | 70.1 | 68 | 0.079 |
| Talk to medical staff | 11423 | 1898 | 70.5 | 67.1 | 0.000 |
| Talk to friends and relatives | 11217 | 2104 | 70.2 | 68.9 | 0.001 |
| TENS | 13271 | 50 | 70 | 63.2 | 0.041 |
| Method | No. of Not Used | No. of Used | Wish for More Pain Treatment if Not Used in % | Wish for More Pain Treatment if Used in % | P Value |
|---|---|---|---|---|---|
| Acupuncture | 14509 | 29 | 14.0 | 17.2 | 0.619 |
| Cold pack | 11805 | 2733 | 16.6 | 15.8 | 0.001 |
| Distraction | 11135 | 3403 | 13.9 | 14.5 | 0.422 |
| Deep breathing | 13654 | 884 | 14.0 | 15.4 | 0.235 |
| Heat | 14230 | 308 | 14.0 | 15.9 | 0.340 |
| Imagery | 14321 | 217 | 14.0 | 17.1 | 0.198 |
| Massage | 14329 | 209 | 14.0 | 17.2 | 0.182 |
| Meditation | 14297 | 241 | 14.0 | 17.8 | 0.087 |
| Music | 14538 | ||||
| Prayer | 13932 | 606 | 14.0 | 14.9 | 0.556 |
| Relaxation | 13903 | 635 | 14.0 | 14.2 | 0.921 |
| Walking | 13871 | 667 | 14.1 | 12.4 | 0.225 |
| Talk to medical staff | 12446 | 2092 | 14.3 | 12.4 | 0.018 |
| Talk to friends and relatives | 12220 | 2318 | 14.0 | 14.2 | 0.867 |
| TENS | 14487 | 51 | 14.0 | 15.7 | 0.734 |
The general linear model showed that age (η2 = 0.006, P < 0.001), gender (η2 = 0.001, P < 0.01), and the usage of NPMs (η2 = 0.002, P < 0.001) explain only 0.006 of the variance of pain relief. Logistic regression results showed the significant impact of age and gender on the wish for more pain treatment. Usage of NPMs does not have a significant impact in either backward or forward analysis.
4.1. Specific Surgeries
Tables 4 - 6 showed the results for the three most frequent surgeries in the PAIN OUT registry. For total hip replacement, the numbers were similar to the global population. For total knee replacement, a different outcome was observed. More NPMs were used (nearly 70% in contrast to around 50% for all patients) and they were associated with higher pain relief (69% for individuals, who used NPMs versus 63% for the others). The wish for more pain treatment did not differ significantly. For laparoscopic cholecystectomy, the numbers changed again. Here, the percentage of usage was lower. Only every third patient used NPMs for pain relief. However, using NPMs or not did not show significant differences.
| NPMs Used | No. (%) | Pain Relief in % | Wish for More Pain Treatment in % |
|---|---|---|---|
| No | 554 (52.6) | 70.7 ± 26 | 13.5 |
| Yes | 500 (47.4) | 69.4 ± 21.5 | 15.7 |
| P value | 0.017 | 0.327 |
| NPMs Used | No. (%) | Pain Relief in % | Wish for More Pain Treatment in % |
|---|---|---|---|
| No | 238 (30.8) | 63.2 ± 28.1 | 22.3 |
| Yes | 535 (69.2) | 69.4 ± 25.8 | 17.5 |
| P value | 0.008 | 0.121 |
| NPMs Used | No. (%) | Pain Relief in % | Wish for More Pain Treatment in % |
|---|---|---|---|
| No | 437 (65.8) | 75 ± 24.8 | 9.4 |
| Yes | 227 (34.2) | 71.7 ± 25 | 11.9 |
| P value | 0.062 | 0.315 |
5. Discussion
Half of the PAIN OUT patients reported that they tried NPMs for pain relief. Women used more methods from groups 2 and 3, and elderly patients used less NPMs overall. However, absolute differences were relatively small.
The literature shows that some NPMs are associated with less postoperative pain. On the whole, this could not be confirmed by the current findings from a large acute pain registry. For some NPMs, there was no association between usage and positive outcomes. Some NPMs were even associated with negative results. Patients, who used them had less pain relief and wished for more pain treatment than those, who did not use NPMs. However, differences were very small and lacked clinical relevance. Observing the subgroups of the three most frequent surgeries in the PAIN OUT registry, the general results were only partly replicated. After total knee replacement, NPMs were indeed associated with a moderate improvement in pain relief.
There seems to be a certain disproportion between the widespread use of NPMs and its lacking association with improved patient-reported outcomes in clinical routine. There are several possible reasons for this finding. First, it might reflect the missing effectivity of most NPMs. Only very few NPMs have been studied by high-quality RCTs and results are ambiguous, as reported above. However, for a few NPMs like TENS, a considerable evidence of analgesic efficacy is documented, yet this was not replicated by the current data. Second, use of NPMs in clinical routine might not always meet the high standards and skills provided in RCTs. Third, the somehow positive findings in knee surgery in the current study might indicate that the efficacy of (some) NPMs is related to specific surgeries. Fourth, standard pain management (e.g. drugs or regional analgesia techniques) was not controlled for or restricted. Therefore, effectiveness of these techniques might have masked the small effect of NPMs. Furthermore, some NPMs might have been used only by patients with severe pain. In other words, the level of pain might have caused use of NPMs, and not vice versa.
Should NPMs therefore be abandoned? Considering the arguments from above and the low side-effect profile of most NPMs, they might still offer benefits for some patients. However, state-of-the-art application should be ensured, and NPMs should not replace analgesic interventions with proven effectiveness. The NPMs might furthermore improve communication and relationship between patients and clinical staff and increase overall patient satisfaction. Future research should study patient as well as surgery-specific conditions associated with improved outcomes, in detail.
The current study had some limitations: First, the PAIN OUT registry was not a randomized controlled trial. For this reason, it is prone to confounding variables, some of which the researchers did not even know about. The researchers controlled for age and gender, which are well-known confounders for acute post-operative pain. Moreover, patients might have chosen NPMs on demand and thus the use of NPMs might characterize a subgroup of patients with more severe pain than in the group with no NPM use. Second, patients tend to use more than one NPM at a time. Hence, any analysis of single methods is influenced by other methods. Third, the analyses might suffer from the multiple testing problem. Since the analyses showed few statistically significant differences and only minor absolute differences, the researchers opted not to correct for multiple testing.
Another concern was that patients might have used NPMs, yet not for pain relief. This could lead to a wrong report of usage patterns. For example, no patient selected music as a NPM for pain relief. It is possible that patients did not have access to music or that they listened to music without knowing that music can be used for analgesia.