1. Background
The brachial plexus block is the method of choice of anesthesia for creating an arterio venous fistula (AVF) in patients with end-stage renal disease (1). In addition to preventing the risks of general anesthesia, it causes peripheral vasodilatation due to sympathetic block, resulting in a better clinical outcome (2, 3). Depending on the location of the surgery, four approaches for brachial plexus block could be used, including interscalene, supraclavicular, infraclavicular and axillary block (4). Many variants of infraclavicular block have also been reported by other researchers (5, 6). Infraclavicular block has been modified by Wilson (7), Kilka (8), and Bourget (9). These alternative approaches have a very low risk for pneumothorax or Phrenic nerve palsy, and make hand and distal upper limb surgeries possible. Furthermore, AVF has a high premature failure rate, which appears to be due to radial artery spasms in response to increased sympathetic activity (10, 11). The use of brachialis plexus block improves blood flow through the fistula by creating vasodilation of the arteries with regional sympathetic block, while providing minimal fluctuation blood pressure and heart rate (12, 13). With the aid of ultrasound, the infraclaviculare brachial plexus block has a low risk of complications and a high success rate (14). Measuring the concentration of pre-inflammatory cytokines (interleukin (IL)-6, IL-1, IL-2, IL10 and tumor necrosis factor (TNF)-alpha) in plasma can help quantifying the postoperative systemic inflammatory response. Specifically, IL-6 has been associated with surgical severity (15) and can be a predictor of postoperative recovery (16). Various mechanisms have been suggested for the analgesic effects of the drugs used in infraclavicular block, each of them has contributed extensively to pain relief. The direct suppression and production transmission of neuronal impulses as a result of the interaction of complex ions with ionic axonal channels and receptors, topical release of enkephalin-like substances, reduction of inflammatory mediators and an increase in anti-inflammatory cytokines are among these mechanisms.
Research on the safety effects of anesthesia has been done in laboratory studies, since human clinical studies are more complex and variables, such as the type and duration of surgery and the underlying diseases can affect the results. Although it is difficult to differentiate the contribution of the patient’s stress levels to perioperative inflammatory cytokine levels, anesthesiologists should not overlook the anti-inflammatory effects of anesthetic drugs (17). Ropivacaine is a long-acting local anesthetic. Its efficacy is similar to bupivacaine, while less cardiovascular and central nervous system complications may occur, after its use (18).
Liu et al. concluded that ropivacaine injection significantly reduced the levels of IL-1, IL-6, TNF-alpha in patient with severe trauma, while no significant differences in IL-4 and IL-10 between the treatment and control groups were observed (19).
2. Objectives
Given that a few studies have been conducted regarding the effects of ropivacaine and bupivacaine in patients undergoing AVF surgery, the aim of this study was to compare sympathetic block and TNF-alpha, IL-6 and IL-1 levels before and after the infraclavicular block with ropivacaine and bupivacaine in these patients.
3. Methods
The sample size was calculated considering 95% confidence interval, statistical power of 0.8 and standard error/standard deviation. The study had two groups with 24 patients in each group. The study was conducted descriptively and approved by the Ethics Committee of Shahid Beheshti University of Medical Sciences with code No: IR.SBMU.RETECH.REC.1396.1364.
Inclusion criteria in present study were as followed: ASA class two to three patients scheduled for AVF surgery, and age of 13 to 61 years. The exclusion criteria were as follows: Injection site infection, local anesthetic sensitivity, coagulation disorders, neuromuscular diseases, obesity, children, mentally retarded people, failed infraclavicular block, history of respiratory illnesses, uncontrolled diabetes, uncontrolled HTN, severe cardiovascular disease, and peripheral neuropathy.
The procedure was explained to the patients and informed consent was obtained from all participants. Patients were randomly divided to bupivacaine and ropivacaine groups. In the first group, the block was conducted with 30 mL of 0.5% bupivacaine while in the second group it was done with 30 mL of 0.5% ropivacaine. Infraclavicular block was performed in a vertical manner using ultrasound guide.
Patients were positioned in the supine position and their head was rotated towards the opposite side to the block. The arm was abducted 90 degrees while the forearm was flexed. The linear 8 - 14 MHZ ultrasound probe was placed in parasagittal plane medial to coracoid process under the clavicle to provide the best cross sectional view of the axillary artery. After sterilizing the skin, the block site was numbed with 2 mL of 2% lidocaine. A 22 gauge Vigon Sono Visible needle with 85 mm length was used to perform the block. Aspiration was done to detect possible intravascular injection and then a test dose was injected, observing the U-shaped drug diffusion (Cephalad, Caudal, and Cavity) around the axillary artery under ultrasonic guide (13, 20). After one minute, if there were no complications, the injection of the whole dose with the above-mentioned dosage was done. During the operation, ECG monitoring, blood pressure, and oxygen saturation level measuring was performed. Sensory block was assessed with pinprick test and motor block was assessed using the modified Bromage scale (0 without paralysis, 1 loose wrist, 2 loose elbows, and 3 complete block). The adequacy of anesthesia was assessed with the need for sedition. The brachial artery diameter was measured at antecubital fossa with ultrasonography before and after the infraclavicular block by the same vascular surgeon in all cases. Blood samples were drawn before the block and one hour after the block to measure IL-1, IL-6, and TNF-alpha.
In analyzing the data, the means, standard deviations, frequency, tables, and charts were used to categorize and summarize the collected data. In the study of statistical assumptions, considering the number of observations in each distribution, the Kolmogorov-Smirnov test was used to verify the normal distribution of the data. Regarding the confirmation of statistical assumptions, covariance analysis test at 95% confidence level and the SPSS software version 22 were used.
4. Results
In this study, 48 patients were randomly divided to two equal groups for infraclavicular block with ropivacaine and bupivacaine drugs. There were no conflicts of interest
The mean age of the ropivacaine group was 44.3 ± 8.8 years while it was 43.74 ± 2.9 years in the bupivacaine group, which was not significantly different (P > 0.05). Twenty-two patients were male and the rest were female, yet there was no significant difference between the two groups in terms of gender (P > 0.05) due to synchronization.
The results of Kolmogorov's test showed that data distribution was normal (P > 0.05). To analyze the data, covariance analysis was used. Table 1 shows the results of covariance analysis comparing the levels of IL-1, IL-6, and TNF-alpha before and after infraclavicular block with ropivacaine and bupivacaine.
| Dependent Variable | Source of Change | SS | df | MS | F | P Value | η2 |
|---|---|---|---|---|---|---|---|
| IL-6 | |||||||
| Pre-test | 0.004 | 1 | 0.004 | 0.66 | 0.421 | 0.014 | |
| Group | 0.001 | 1 | 0.001 | 0.167 | 0.685 | 0.004 | |
| Error | 0.291 | 45 | 0.006 | ||||
| Modified total | 0.297 | 47 | |||||
| TNF | |||||||
| Pre-test | 0.057 | 1 | 0.057 | 259.0 | 6130 | 0.006 | |
| Group | 0.363 | 1 | 0.363 | 1.638 | 0.2 | 0.035 | |
| Error | 9.979 | 45 | 0.222 | ||||
| Modified total | 10.373 | 47 | |||||
| IL-1 | |||||||
| Pre-test | 0.005 | 1 | 0.005 | 2.557 | 0.117 | 0.059 | |
| Group | 0.001 | 1 | 0.001 | 0.091 | 0.765 | 0.022 | |
| Error | 0.09 | 45 | 0.002 | ||||
| Modified total | 0.097 | 47 | |||||
| Arterial diameter | |||||||
| Pre-test | 4.26 | 1 | 4.26 | 59.765 | 0.00 | 0.24 | |
| Group | 2.881 | 1 | 2.881 | 40.421 | 0.00 | 0.473 | |
| Error | 3.207 | 45 | 0.071 | ||||
| Modified total | 11.119 | 47 |
Abbreviations: IL, interleukin; TNF, tumor necrosis factor.
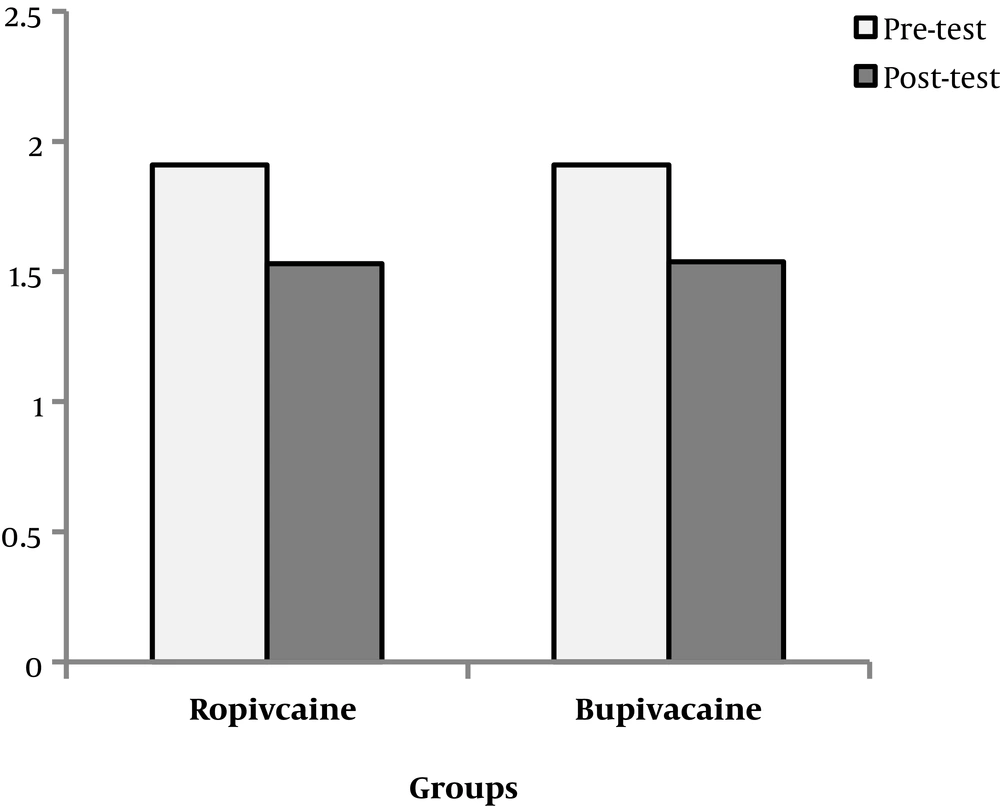
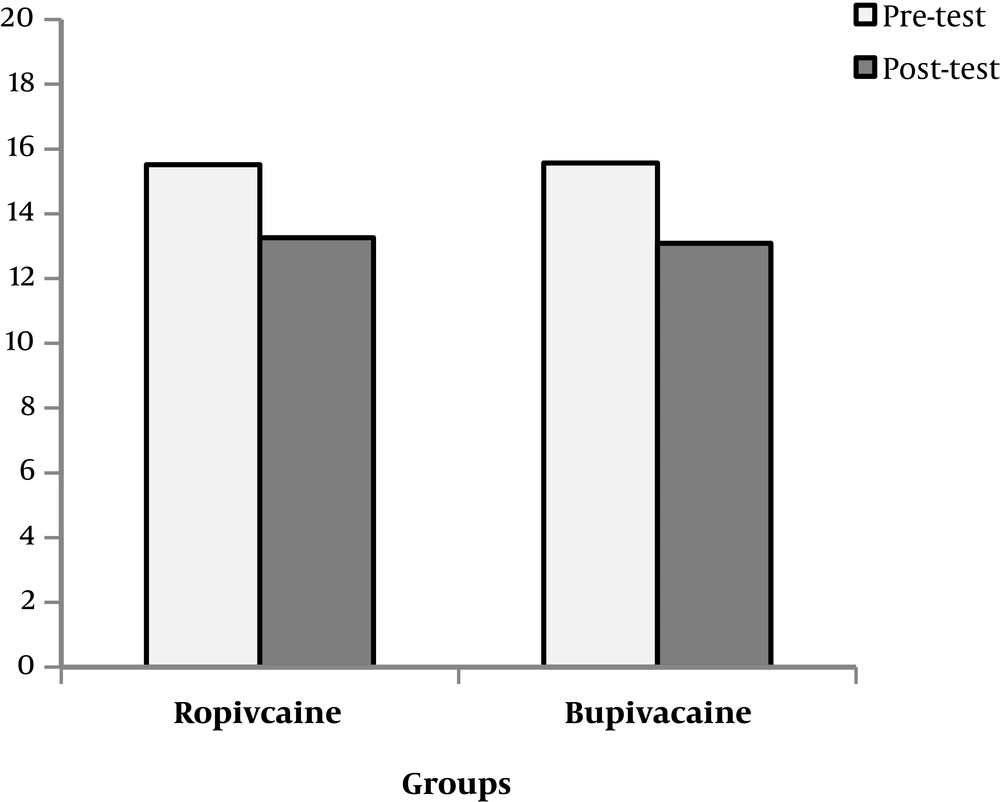
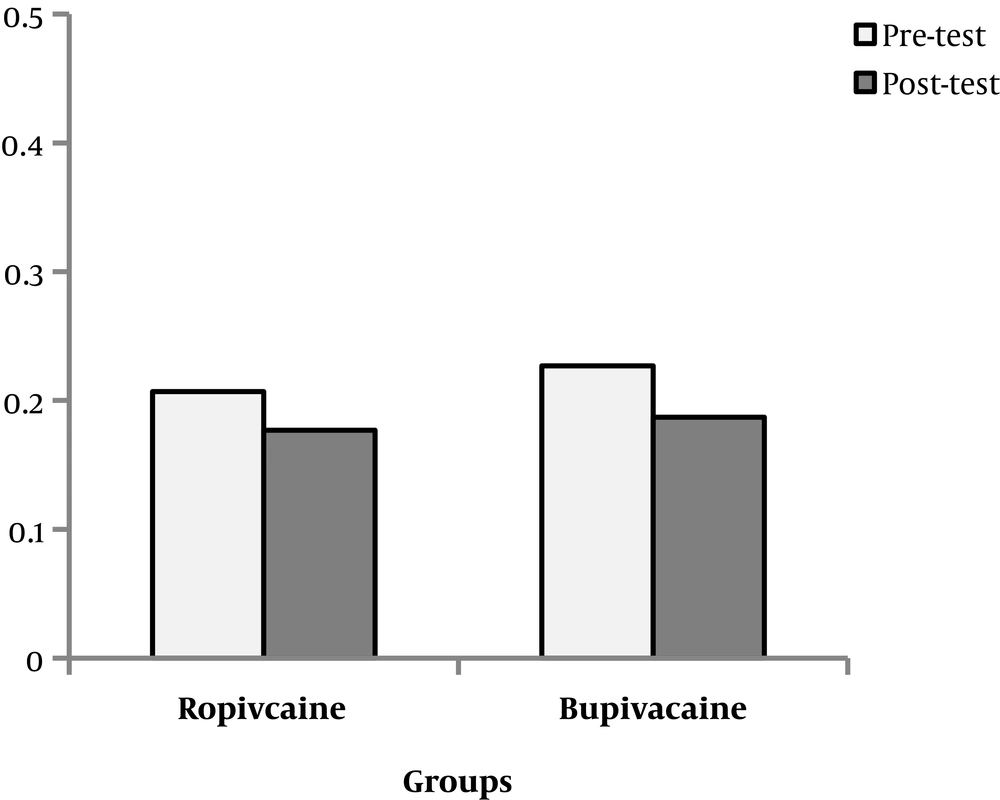
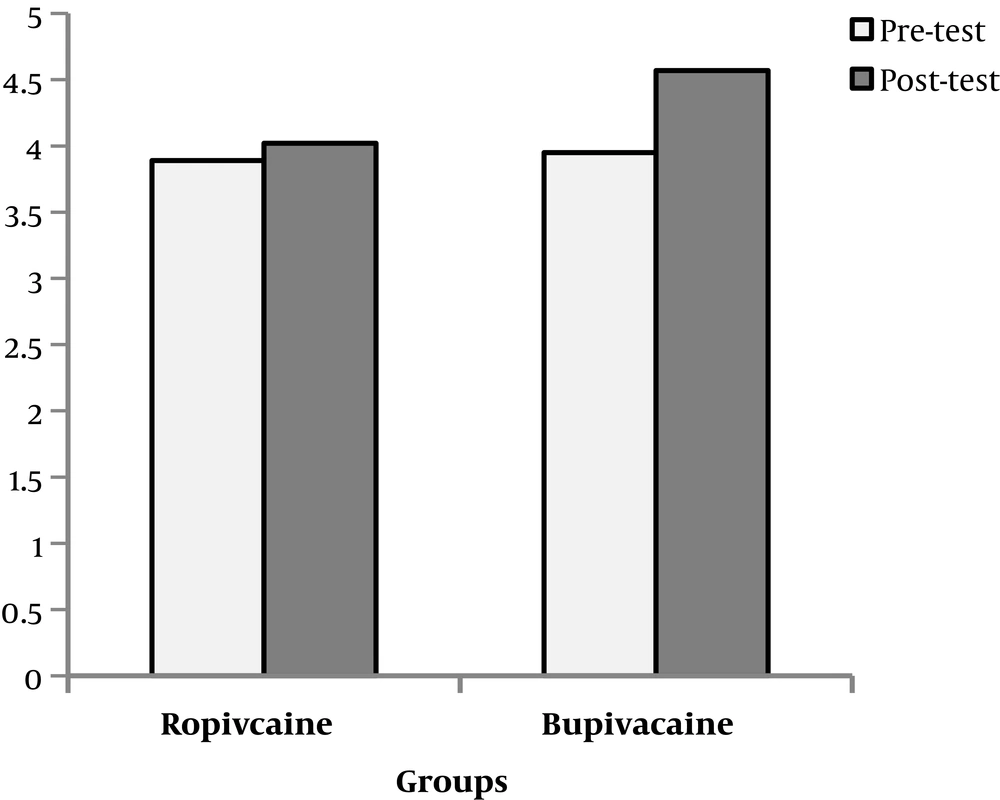
Based on the data in Table 1, after controlling the effect of pre-test (η2 = 0.014, P = 0.421, F (1, 45) = 0.66), the effect of the group on the IL-6 scale was not statistically significant (η2 = 0.004, P = 0.685, F (1, 45) = 0.66). After controlling the pre-test effect (η2 = 0.006, P = 0.613, F (1, 45) = 0.259), the effect of the group on TNF-alpha was not statistically significant (η2 = 0.035, P = 0.2, F (1, 45) = 1.638). After controlling the pre-test effect (η2 = 0.054, P = 0.117, F (1, 45) = 2.557), the effect of the group on IL-1 scale was not statistically significant η2 = 0.002, P = 0.765, F (1, 45) = 0.091). After controlling the pre-test effect (η2 = 0.24, P = 0.005, F (1, 45) = 59.765), the effect of the group on the diameter of the arteries was statistically significant (η2 = 0.473, P = 0.00, F (1, 45) = 40.421). It can be concluded that there was no significant difference between IL-1, IL-6, and TNF-alpha post-test levels in ropivacaine and bupivacaine groups, while the diameter of the arteries was different among the two groups (Figures 1 - 4).
To compare the effect of ropivacaine and bupivacaine, the t-test was used. The results are presented in Table 2. In the ropivacaine group, mean IL-6 in the post-test data was 0.024 lower than its mean in the pretest data, which was statistically significant (P = 0.001, t (23) = 23.684). The mean TNF-alpha levels in the post test data was 0.132 lower than the mean in the pretest results. This difference was statistically significant (P < 0.001, t = 17.1). The mean IL-1 levels in the post-test results was 0.011 lower than its mean in the pre-test data, which was statistically significant (P = 0.018, t (23) = 2.543). The mean arterial diameter in the post-test results was 2.7 times greater compared to the pre-test data, which was statistically significant (P = 0.01, t (23) = 2.7).
| Group | Variable | Mean | SE | Difference of the Means | t | df | P Value |
|---|---|---|---|---|---|---|---|
| Rupiovacaine | |||||||
| IL-6 | 3820 | 0.119 | 0.024 | 15.64 | 23 | 0.00 | |
| TNF | 2.262 | 0.64 | 0.132 | 17.1 | 23 | 0.00 | |
| IL-1 | 0.03 | 0.057 | 0.011 | 2.543 | 23 | 0.018 | |
| Arterial diameter | -0.0125 | 0.22 | 0.044 | -2.7 | 23 | 0.02 | |
| Bupiovacaine | |||||||
| IL-6 | 0.37 | 0.089 | 0.018 | -2.7 | 23 | 0.00 | |
| TNF | 2.473 | 0.267 | 0.054 | 45.228 | 23 | 0.00 | |
| IL-1 | 0.041 | 0.05 | 0.01 | 3.995 | 23 | 0.001 | |
| Arterial diameter | -0.61 | 0.3 | 0.06 | -9.996 | 23 | 0.00 |
Abbreviations: IL, interleukin; TNF, tumor necrosis factor.
In bupivacaine group, the mean IL-6 in the post-test data was 0.018 lower than its mean in the pre-test results, which was statistically significant (P = 0.00, t (23) = 20.7). The mean TNF-alpha in the post test data was 0.054 lower than its mean in the pretest results, which was statistically significant (P = 0.00, t (23) = 45.228). The mean IL-1 in the post test results was 0.01 lower than its mean in the pretest data, which was statistically significant (P = 0.001, t (23) = 3.995). The mean arterial diameter in the post test results was 0.06 greater than the mean in the pretest data, which was statistically significant (P = 0.00, t (23) = 9.996).
5. Discussion
The aim of this study was to compare sympathetic block and measure the levels of TNF-alpha, IL-6, and IL-1 before and after the infraclavicular block with ropivacaine and bupivacaine in patients undergoing AVF surgery. The findings showed that the two drugs had similar effects on inflammatory factors. The results of t-correlation analysis showed that in both ropivacaine and bupivacaine groups, the TNF-alpha, IL-6, and IL-1 levels decreased after the block while ropivacaine significantly increased the diameter of the artery compared to the bupivacaine group.
This finding suggested that both drugs were effective in reducing inflammatory factors. Rathod et al. compared brachial plexus block with 0.5% ropivacaine and bupivacaine. They concluded that the quality of anesthesia was similar in the two groups, however, the duration of motor block using bupivacaine was significantly longer (21). Raeder et al. showed that using 0.75% ropivacaine for axillary block provided better anesthetic effects in comparison with the same volume of 0.5% bupivacaine, although the onset and duration of the block were similar in both groups (22). Findings of this study were not consistent with the results of Pongraweewan et al. (23). They showed that adding 2% lidocaine to 0.5% bupivacaine in the brachial plexus block (BPB) did not increase the duration of the sensory block while increasing the satisfaction of the patient and the surgeon (23). Sahin et al. concluded that Infraclaviculare block of brachial plexus increased the radial artery flow at primary and late stages compared with local anesthetic infiltration, resulting in a remarkable vasodilation resulting from the sympathectomy (24).
Anti-inflammatory effects of local anesthetics directly affect the function of the polymorphonuclear leukocytes (PMNS), macrophages, and monocytes. In laboratory studies using ropivacaine and lidocaine (100 to 300 mM), local anesthetics decreased TNF-alpha levels by increasing the levels of CD11b/CD18 (25). Therefore, it could be concluded that local anesthesia can reduce the adhesion, migration, and accumulation of PMNs at the inflammation site. Furthermore, local anesthesia is well known for inhibiting excessive inflammatory responses without significant impairment in the immunity of the host (26).
5.1. Limitation
The major limitation of the current research was the low sample size. Further researches are recommended with a larger sample size in future studies.
5.2. Conclusions
In general, the present study showed that each of the drugs alone could reduce the pre-inflammatory factors. Ropivacaine significantly increased the arterial diameter compared to the bupivacaine group.