1. Background
One of the most commonly performed surgeries in ophthalmology is cataract surgery (1, 2). Different anesthesia protocols are introduced for cataract surgery including general anesthesia, local, topical, or combination of the above methods (3, 4). Recently, due to the emergence of new technologies in this field such as phacoemulsification, employing anesthetic regime properly is a challenging issue for anesthesiologists. The most commonly used technique in phacoemulsification is local anesthesia. Retrobulbar and peribulbar anesthesia, in addition to topical anesthesia, are the highly recommended protocols. Evidence indicates that using local anesthesia is associated with some complications and in order to prevent such complications, topical anesthesia is increasingly employed. Pain is one of the frequently reported complications of topical anesthesia (5-8); therefore, in order to alleviate patients’ pain and anxiety and also compliance with the procedure, different sedation protocols are recommended such as using opioids, propofol, benzodiazepines, and midazolam (9, 10).
A proper sedation method for such ophthalmic procedures under local anesthesia should have a rapid onset, but a short duration of action and the anesthetic and sedative agents should be non-toxic, non-accumulating, and have predictable activity with minimal side effects. Cost-effectiveness of the agent and method is also a matter (11).
Combination therapy is another recommended option in this field, which could have proper outcomes due to the synergistic effects of the agents in accordance with lower dosage of each agent alone (11). Documents demonstrated the effectiveness of different combination therapies to achieve conscious sedation during cataract surgery under local anesthesia (11).
Fentanyl is a highly lipid-soluble opioid commonly used for sedation/analgesia mainly in local or topical anesthesia. It has no anti-anxiety and anti-amnesia effects. Due to the mentioned characteristics and quick passage across the blood-brain barrier, it has a rapid onset and short duration of action. Since fentanyl has no histamine release effect, it is considered as a great intravenous anesthetic agent (12, 13).
One of the most preferred benzodiazepines for local or topical anesthesia is midazolam. The favorable characteristics of midazolam are its rapid and short-acting properties, wide margin of safety, and high therapeutic index. Its rapid onset of action is due to its higher solubility both in lipids and water (14).
Propofol is another important intravenous anesthetic and sedative agent used extensively in ophthalmic procedures. The favorable pharmacokinetic property of propofol regarding anesthetic effect is its large volume of distribution due to high protein binding. Though propofol is comparable to midazolam in terms of anesthetic effect, but it has some superiority to midazolam regarding less post-operative vomiting, lower intraocular pressure (IOP), and earlier return to-home readiness. Propofol has dose-dependent mild cardiovascular and respiratory depression effects, which make it a proper sedative agent. It has no residual effects on the central nervous system, which result in rapid recovery. Moreover, due to rapid metabolism and hepatic clearance as well as lack of cumulative effects, propofol has minimal effect on blood pressure and heart rate during induction of anesthesia. Due to lack of analgesic properties, propofol is commonly used in combination with opioids (15-17).
Another most common non-barbiturate, non-benzodiazepine, imidazole derivate agent used for ophthalmic surgeries is etomidate. Its properties are rapid onset of action, short duration of sedation, and fewer clinical hemodynamic alterations and respiratory effects. Etomidate has no analgesic effects; therefore, it is recommended to be used in combination with analgesic agents such as fentanyl (18, 19).
According to the favorable effects of combination therapy to provide better sedation during phacoemulsification (11), and lack of studies investigating the sedative effect of etomidate, propofol, and midazolam in combination with fentanyl during the procedure, the current study aimed at comparing the sedative properties of the mentioned three combination therapies in this field.
2. Objectives
The study findings would be helpful for selecting an appropriate anesthetic procedure for phacoemulsification cataract surgery.
3. Methods
The current double-blind randomized, controlled, clinical trial was conducted on patients referred to Feiz Hospital, a referral ophthalmologic center in Isfahan province, Iran, affiliated to Isfahan University of Medical Sciences, for elective phacoemulsification surgery under sedation. The study was conducted from November 2017 to June 2018.
The current study protocol was approved by the Anesthesiology Department and Ethics Committee of Isfahan University of Medical Sciences and registered at the Iranian Registry of Clinical Trials (code: IRCT20170809035601N10).
The current study was conducted on patients aged 35 - 86 years with ASA (the American Society of Anesthesiologists) physical status of I or II. Pregnant female patients, the ones with chronic pain syndrome, and known hypersensitivity to either medication or mentally disabled ones were excluded. In addition, the patients who used any analgesic or anesthetic drug 24 hours prior to surgery were also excluded.
The method of the trial and the study objectives were explained to the selected patients and written informed consent was obtained from participants.
Using random allocation software, the selected patients were randomly allocated to three groups to receive fentanyl and one of the following medications: propofol, midazolam, or etomidate.
Demographic characteristics and medical condition of all participants were recorded by an anesthesiologist blinded to the groups.
Hemodynamic parameters before, during, and after surgery, sedation level, anesthetic complications, sedation related adverse events, and patients’ and surgeons’ satisfaction were evaluated and recorded by the anesthesiologist and compared in the three studied groups.
3.1. Randomization and Blinding
A double-blind randomization was performed in the current study. Before surgery, using a computer-generated sequencing, the patients were randomly allocated into three groups. In the study, both the participants and the data collectors were blind to the grouping of participants.
The study drugs were prepared in four syringes covered with aluminum foil, by an anesthesiologist not involved in data collection.
3.2. Anesthetic Procedure
Electrocardiography (ECG), pulse oximetry, capnography, and automated noninvasive blood pressure monitoring was performed in patients before and during the procedure.
Patients received oxygen 4 L/minute via the nasal route. Systolic and diastolic blood pressure, heart rate, and blood oxygen saturation (SpO2) were measured and recorded prior to inducing sedation, every five minutes during surgery, and every 10 minutes in the recovery room. The patients from 35 to 65 years old received 1.5 µg/kg of fentanyl for pain relief. However, in the patients older than 65 years, the dosage was decreased to 0.75 - 1 µg/kg. After two minutes, in each group of patients the anesthetic agent was injected within 30 seconds until reaching the proper sedation level; in the propofol group, propofol titrated at a dose of 0.5 mg/kg, in the midazolam group, titrated midazolam at a dose of 0.04 mg/kg, and in the etomidate group, titrated etomidate at a dose of 0.1 mg/kg were injected. In patients older than 65 years, the anesthetic agent was injected in half of the recommended dosage.
The safe and effective sedation level in the present study was defined as patient's ability to maintain consciousness/responsiveness throughout the surgery.
Sedation level was measured using the Ramsay sedation scale classified 1 - 6 (1 = anxious, 2 = calm, 3 = lethargic, 4 = confused but responding to conversation, 5 = no response to speaking, 6 = no response to painful stimulation).
The study goal was to achieve a sedation level of 3 - 4 based on Ramsay sedation scale.
If the Ramsay sedation scale score was < 3, rescue medication with propofol 20 mg (at a concentration of 5 mg/mL), midazolam 2 mg (at a concentration of 0.5 mg/mL), and etomidate 4 mg (at a concentration of 1 mg/mL) was administered in the three groups.
Anesthetic complications including bradycardia, tachycardia, hypotension, hypertension, hypoxemia, apnea, myoclonus, SpO2 less than 90%, agitation, and postoperative nausea and vomiting were treated and recorded by the anesthesiologist blinded to the groups.
The interval between the end of the procedure and meeting the criteria to be discharged from the postanesthesia care unit (the recovery time) was recorded.
The recovery of the patients was evaluated using a modified Aldrete score. It was determined by scoring from 0 to 10, according to the patient’s activity, oxygen saturation, consciousness, respiration, and circulation.
Patients with an Aldrete score ≥ 9 were discharged from the postanesthesia care unit.
Bradycardia/tachycardia: Decrease or increase of heart rate by 20% of basal values,
Hypotension/hypertension: Decrease or increase of the blood pressure by 20% of baseline during intra- and postoperative period,
Hypoxemia (SpO2 < 90%),
Apnea: Complete cessation of breathing for 10 seconds or more.
Sedation-related adverse events including aspiration, laryngospasm, intubation, hospitalization, or mortality were treated and recorded also by the investigator blinded to the groups.
Desaturation were treated in operation or recovery room (SpO2 less than 92% were encouraged to breathe more, and less than 90% SpO2 were ventilated with mask) and results were recorded.
We used modified Aldret score for recovery time evaluation (20). Patients were discharged when achieving an Aldrete score of 9 - 10.
At the end of the surgery (after full recovery) or before discharge, the patients’ and surgeons’ satisfaction were evaluated and recorded by the anesthesiologist using a five-point Likert scale (1 = strongly disagree, 2 = disagree, 3 = neither agree nor disagree, 4 = agree, 5 = strongly agree).
3.3. Statistical Analysis
Recorded data were analyzed with SPSS version 23. The quantitative and qualitative variables were reported as mean (SD) or median (range) and number (percentage), respectively.
4. Results
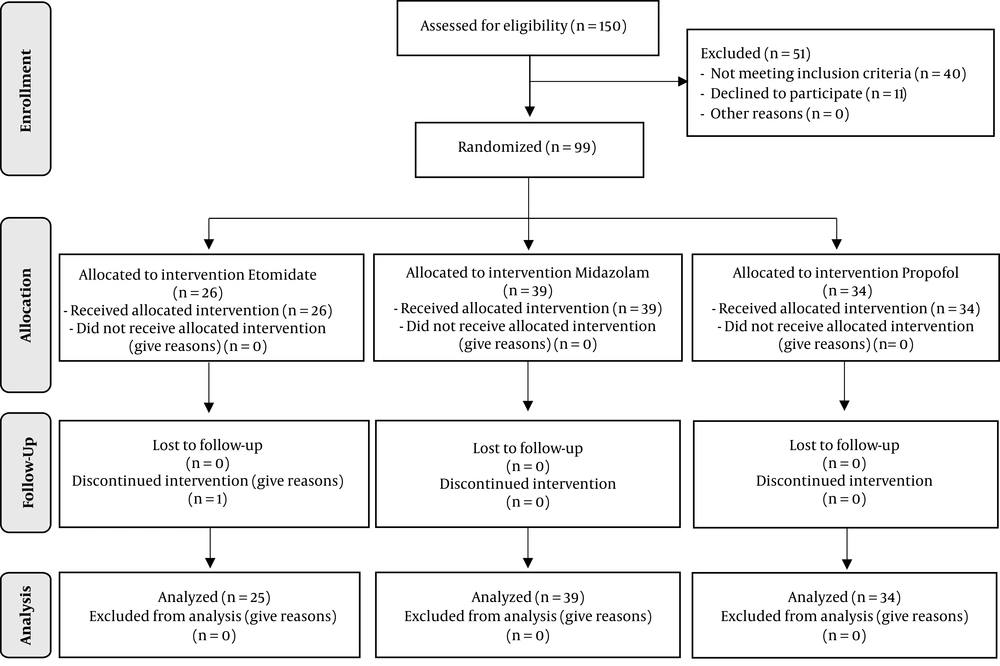
Out of the 150 initially enrolled patients, 51 participants were excluded (40 patients were not eligible, and 11 patients refused to sign the informed consent). Based on the inclusion criteria, 99 eligible patients were randomly allocated into three groups. During the procedural sedation, one patient from the etomidate group was excluded (twilight anesthesia was shifted to general anesthesia due to changed surgical plan (Figure 1).
In the current study, 98 patients (57 males and 48 females) completed the study. Mean age of the studied population was 69.68 ± 12.0 years. Demographic characteristics of the studied patients are presented in Table 1. There were no significant differences among the groups in terms of mean of age, weight, and height of the patients (P > 0.05).
| Variable | Etomidate, N = 25 | Midazolam, N = 39 | Propofol, N = 34 | P Value |
|---|---|---|---|---|
| Age, y | 69 ± 8.5 | 71.6 ± 11.0 | 67.7 ± 15 | 0.38 |
| Gender, female/male | 13/12 | 21/18 | 16/18 | 0.84 |
| Weight, kg | 67.4 ± 11.3 | 65.4 ± 15.4 | 69.8 ± 15.6 | 0.64 |
| Height, cm | 164.1 ± 7.2 | 163 ± 8.4 | 164.9 ± 19.5 | 0.66 |
Operative details of patients in the three studied groups before, during, and after procedure are presented in Table 2.
Frequency of different levels of Ramsay scores was not significantly different between the groups (P = 0.41). Frequency of Ramsay scores of 3 and 4 was 92%, 79.4%, and 88.2% in etomidate, midazolam, and propofol groups, respectively (P = 0.32).
The median recovery time was significantly higher in the midazolam group than the propofol group (P = 0.04).
Before surgery, the hemodynamic characteristics of the patients were not different in the three groups. During surgery and recovery, mean systolic and diastolic blood pressure and mean arterial blood pressure were significantly lower in the midazolam group than others (P > 0.05). Intragroup comparison indicated that pulse rate, systolic and diastolic blood pressure, and mean arterial blood pressure significantly decreased during procedure until recovery time (P < 0.001) in three groups. There was no significant difference among the groups in arterial oxygen saturation during the procedure.
Rescue dose was administrated to eight, eight, and seven patients from the etomidate, midazolam, and propofol groups, respectively. The differences between groups was insignificant (P = 0.506).
There were no significant differences between the groups regarding different anesthetic complications except for nausea, which was significantly higher in the etomidate group than the others (P < 0.001).
There was no report on sedation-related adverse events in all studied groups.
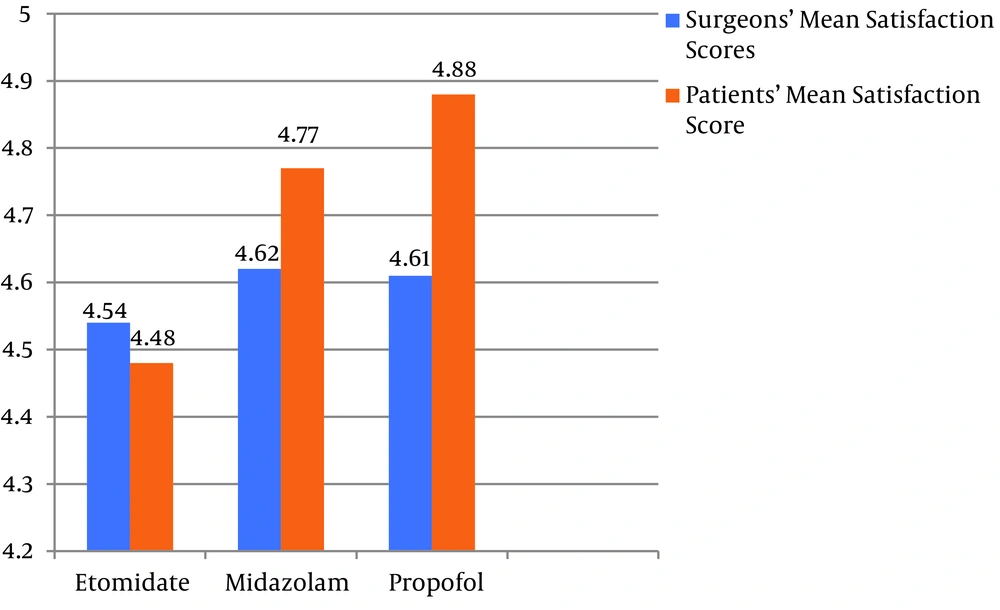
The patients’ and surgeons’ mean scores of satisfaction in the three studied groups are presented in Figure 2. There was no significant difference in surgeons’ mean score of satisfaction among the groups (P > 0.05).Intergroup comparisons indicated that the patients’ mean score of satisfaction was significantly higher in the propofol group than that of the etomidate group (P = 0.006; post hoc Tukey test).
| Variable | Etomidate, N = 25 | Midazolam, N = 39 | Propofol, N = 34 | P Value |
|---|---|---|---|---|
| Before Surgery | ||||
| Pulse rate | 75.1 ± 15.2 | 76.7 ± 15.4 | 73.6 ± 10.1 | 0.917 |
| Blood pressure | ||||
| Systolic | 154.6 ± 18.5 | 150.6 ± 22.9 | 157.7 ± 20.1 | 0.35 |
| Diastolic | 88.8 ± 8.9 | 84.6 ± 13.1 | 90.8 ± 10.6 | 0.63 |
| Mean arterial blood pressure | 109.8 ± 8.8 | 106.3 ± 14.2 | 112.8 ± 12 | 0.087 |
| Arterial oxygen saturation | 95.4 ± 2.4 | 94.6 ± 5.3 | 95.3 ± 2.5 | 0.659 |
| During Surgery | ||||
| Ramsay score | 0.41 | |||
| 1 | 1 (4) | 5 (12.8) | 1 (2.9) | |
| 2 | 1 (4) | 3 (7.7) | 3 (8.8) | |
| 3 | 9 (36) | 7 (17.9) | 7 (20.6) | |
| 4 | 14 (56) | 24 (61.5) | 23 (67.6) | |
| Pulse rate | 71.1 ± 13.6 | 70.7 ± 10.4 | 69.9 ± 11.2 | 0.911 |
| Blood pressure | ||||
| Systolic | 155.1 ± 22.0 | 136 ± 18.5 | 145.1 ± 19.7 | 0.001 |
| Diastolic | 91.1 ± 9.4 | 78.2 ± 11.7 | 84.8 ± 11.6 | 0.000 |
| Mean arterial blood pressure | 111.6 ± 12.2 | 97.2 ± 12.8 | 104.6 ± 13.3 | 0.000 |
| Arterial oxygen saturation | 97.2 ± 2.8 | 96.7 ± 5.7 | 97.2 ± 2.2 | 0.807 |
| After Surgery and Recovery | ||||
| Recovery time | 12 (5 - 24) | 20 (5 - 40) | 5 (5 - 10) | 0.04 |
| Pulse rate | 66.8 ± 13 | 68.5 ± 12.4 | 69.4 ± 11.7 | 0.713 |
| Blood pressure | ||||
| Systolic | 143.4 ± 24.3 | 129 ± 20.8 | 140.1 ± 18.7 | 0.016 |
| Diastolic | 85.8 ± 14.1 | 74.1 ± 13.1 | 82.2 ± 11.7 | 0.001 |
| Mean arterial blood pressure | 105.8 ± 17.3 | 92.1 ± 14.7 | 101.2 ± 13 | 0.001 |
| Arterial oxygen saturation | 98 ± 1.4 | 95.4 ± 11.0 | 97.9 ± 3.5 | 0.245 |
| Anesthetic complications | ||||
| Dizziness | 0 (0) | 1 (2.6) | 0 (0) | 0.89 |
| Restlessness | 2 (8) | 4 (10.26) | 1 (2.9) | 0.47 |
| Vomiting | 0 (0) | 0 (0) | 0 (0) | 0.48 |
| Nausea | 13 (52) | 2 (5.2) | 0 (0) | < 0.001 |
| Hypoxemia | 1 (4) | 0 (0) | 2 (5.8) | 0.61 |
| Bradycardia | 8 (32) | 10 (26) | 7 (20.6) | 0.33 |
| Tachycardia | 3 (12) | 2 (3.2) | 1 (2.9) | 0.67 |
| Hypotension | 5 (20) | 13 (33.3) | 11 (32.35) | 0.47 |
| Sedation adverse event | 0.96 | |||
| Aspiration | 0 (0) | 0 (0) | 0 (0) | |
| Laryngospasm | 0 (0) | 0 (0) | 0 (0) | |
| Intubation | 0 (0) | 0 (0) | 0 (0) | |
| Hospitalization | 0 (0) | 0 (0) | 0 (0) | |
| Mortality | 0 (0) | 0 (0) | 0 (0) | |
aValues are presented as mean ± SD or median (range) and No. (%).
5. Discussion
In the current study, the sedative quality of etomidate, propofol, and midazolam was evaluated and compared in phacoemulsification cataract surgery. The findings indicated that all three agents had appropriate quality of sedation (≥ 80%).The frequency of Ramsay sedation scores of 3 - 4 was higher in etomidate and propofol groups, respectively.
The sedation rate for propofol was 88% that was significantly higher than those of previous reports (20) and even higher than the rate reported for midazolam (79%). The finding could be explained by deeper levels of sedation for propofol and more prolonged sedation for midazolam. The current study findings were similar to previous reports in this field (21-23).
In addition, the half-life is shorter in propofol than midazolam (24).
The sedation rate of etomidate and propofol was almost similar in the current study.
Toklu et al., in Turkey demonstrated that frequency of Ramsay sedation scores of 3 - 4 was similar in the two group of patients undergone elective colonoscopy with etomidate-remifentanil and propofol-remifentanil combinations (25).
In another study conducted by Dickinson et al., the effectiveness of etomidate and midazolam for pediatric orthopedic surgeries was compared; they demonstrated that etomidate provided shorter, but more effective, sedation than midazolam (26).
In the current study, median of recovery time in the propofol group was significantly lower than those of the other two groups.
The current study results were in contrast with those reported by Banihashem et al. They indicated that recovery time in the etomidate-fentanyl group was significantly lower than that of the propofol-fentanyl group (18). Toklu et al., also reported shorter recovery time for etomidate than propofol during colonoscopy (25).
The current study findings were similar to those reported by Moerman et al. They found that during recovery after cardioversion procedure, time recorded for propofol was shorter than that of etomidate (27).
It seems that higher sedation score is associated with lower recovery time. However, in the midazolam group, the frequency of Ramsay scores of 3 - 4 was lower than those of the other groups, and recovery time was longer than those of the others.
Hemodynamic evaluation at baseline in the current study did not show any significant differences between the studied groups, but during and after surgery, the mean systolic and diastolic blood pressure and mean arterial blood pressure were significantly lower in the midazolam group than others.
Intragroup comparisons indicated that pulse rate, systolic and diastolic blood pressure, and mean arterial blood pressure decreased significantly during procedure until recovery time in three groups (P < 0.001).
In a study conducted by Aghadavoudi et al., in order to compare the effects of etomidate infusion with those of fentanyl-midazolam-ketamine on quality of sedation during cataract surgery, the results showed that the hemodynamic changes and the pulse rate increased significantly after recovery. They also reported that the hemodynamic fluctuations significantly decreased in the group receiving etomidate and fentanyl, which were not consistent with the results of the present study (28). The results of the current study were also inconsistent with those of the studies by Choi et al. (29) and Vinson and Bradbury (30). Different results can be attributed to differences between the applied dosages, duration of surgery, and administration of a sedative drug in bolus or infusion.
Regarding mean systolic and diastolic blood pressure and mean arterial blood pressure, the current study results were in contrast to those reported by Di Liddo et al. They investigated the effects of etomidate and midazolam on pediatric outpatient surgeries and demonstrated that the systolic and diastolic blood pressure levels were not significantly different in the group receiving etomidate, but significantly different from those receiving midazolam (31).
In current study, inter- and intragroup comparisons showed no significant changes in arterial oxygen saturation during the procedure. In the study of Aghadavoudi et al., the oxygen saturation percentage was significantly higher in the etomidate-fentanyl group, especially after recovery, than that of the fentanyl-midazolam-ketamine group, which was not consistent with the results of the present study (28).
The current trial did not report any sedation-related adverse events in the three studied groups. The results were similar to those of previous studies demonstrating no sedation adverse events such as aspiration, laryngospasm, need for intubation, hospital admission, or death from midazolam or propofol complications (32).
There were no significant differences between groups regarding different anesthetic complications except for nausea, which was significantly higher in the etomidate group than others (P < 0.001).The most common reported complication in the three groups was hypotension. Though it was not statistically different, its frequency was lower in the etomidate group. It may be due to the point that etomidate does not suppress sympathetic tone or myocardial function (33).
In the current study, there was no significant difference among the study groups regarding surgeons’ mean score of satisfaction. Banihashem et al., also reported similar satisfaction scores for the propofol-fentanyl and etomidate-fentanyl groups during elective colonoscopy (18).The current study finding in this regard was similar to those reported by Aghadavoudi et al. (28), and Vinson and Bradbury (30). Some studies demonstrated that the method of sedation had no significant impact on the physicians’ or patients’ satisfaction (25, 34, 35).
Regarding patients’ mean score of satisfaction, the current trial results indicated that the score of the propofol group was significantly higher than that of the etomidate group.
Aghadavoudi et al. (36), and Lee-Jayaram et al. (37) compared the efficacy of etomidate-fentanyl versus ketamine-midazolam in procidural sedation for cataract surgery and pediatric orthopedic reductions, respectively. Both studies indicated that patients’ satisfication score was significantly higher in the ketamine-midazolam group than that of the etomidate-fentanyl group. In the present study, though the difference was not significant, patients’ satisfication score was higher in the midazolam group than the etomidate group.It is suggested that the pain caused by the etomidate injection could explain lower satisfaction score of the patients.
The limitation of the current study was the small sample size. The strength of the study was its novelty.
5.1. Conclusions
The current study findings indicated that though the quality of sedation during phacoemulsification cataract surgery was acceptable in the three agents and showed no significant differences between the groups, considering other studied factors including recovery time, hemodynamic evaluation, sedation-related complications, and patients’ satisfication score, it is suggested that propofol was superior to other two studied agents. However, further studies with larger sample sizes are recommended to obtain more conclusive results in this field.