1. Background
Chronic pain is the most common and annoying human experiences. Among the different types of pain, headache is one of the most commonly reported complaints in neurology clinics, which leads to heavy annual spending on health care systems (1).
In the recent decades, diagnostic criteria for a headache and beneficial drug and non-pharmacological treatments have been developed (2) and in this regard, the role of biological, psychological, and social factors has been recognized in the headache experience. Prior to treatment, informing factors influencing disease is very important and because chronic pain is a multi-dimensional structure, it is required to examine the various cognitive, emotional, and behavioral dimensions of chronic pain (3).
In understanding chronic pain control, emphasis of recent researchers is not on changing pain intensity, as past studies have noted in change in one’s relationship to pain, which includes pain interference (4).
In people with chronic pain, “interference” refers to the conflict with emotional and physical’s functions. Chronic pain can interfere with functions related to quality of life, daily routine activities, self-care, social activities, communication and learning new information and skills, while it could lead to in the absence of education, work, and inability of active social life (5, 6).
Recently, research on pain assessment has identified and distinguished between two types of emotional and physical pain interference (7). Although emotional interference (patient relations with others, enjoyment of life, and mood) and physical interference (problems associated with work, general activity, and walking) are often distinguished in practice (2, 8), they are not logically distinct in researches.
It is believed that differentiating between these two types of interference, helps the therapist apply more appropriate methods to pain control (9). Also, during the intervention, isolating these types of pain interference in comparison to pain conditions has led to the capacity to examine the possible advantages of the multimodal treatments in pain management.
In understanding chronic pain, using technology, such as functional MRI, studies have conclusively demonstrated that there is an inherent overlap between neural networks that are influencing the transmission of acute to chronic pain and brain regions involved in attention mechanisms (4, 5), and there is evidence that psychosocial constructions are efficacious in pain management (6, 7). Also, the role of top-down attention-centered mechanisms is the intermediate mechanism between headache intensity (8).
One top-down cognitive processing in pain regulation is mindfulness. “Mindfulness” is the brain’s complex mechanism focused on the present moment (9). Mindfulness has several neuronal mechanisms and with a “sustained attention” on a specific subject, disengages individuals from inconsistent information.
In this regard, studies have shown that mindfulness predicts pain intensity (10), while equally influencing pain interference (11).
For example, mindfulness-based intervention studies have found positive effects on pain interference (12, 13), yet these researches have not provided the separated result about emotional or physical pain interference. To better understand chronic pain management, examination of important structures in pain adjustment should be noted.
In order to accurately understand the role of mindfulness state in pain management, in the present study, the researchers examined the role of mindfulness in adjusting these patients with two types of pain interference.
2. Objectives
In this paper researchers investigated the relationship between pain intensity and mindfulness with emotional and physical pain interference and the ultimate aim was to answer the following research questions:
Does pain intensity and mindfulness influence emotional and physical pain interference in patients with primary headache? Does pain intensity by mindfulness influence these two types of pain interference, differently?
3. Methods
The study has been conducted descriptively and was approved by the Ethics Committee of Alborz Islamic Azad University of Medical Sciences.
This study was conducted during years 2017 to 2018 at Imam Hossein Hospital of Tehran province. The statistical society included 210 individuals with headache referring to the health care system of Tehran city, Iran. Using Morgan, Krejcie, and Cohen ((14) and via a purposive selection method, a sample of 132 patients was selected by a neurologist; from these people, after removing those, who were inconsistent with the inclusion criteria, 85 individuals completed the questionnaires as final samples. A clinical health psychologist evaluated the patients. Also, participants compensated an invitation card with Life skills workshop theme for each in-person assessment completed. The aim of the examination was described to the patients and their endorsement, the informed consent and researchers, was committed to protecting the privacy of respondents. The sample included 34% males and 66% females aged between 19 and 65 years old (M = 37.2, SD = 12.2), all of whom had at least three pain days per month (for more than three months) due to a primary headache pain type (i.e., tension-type headache, migraine, trigeminal autonomic cephalalgias, or other) as defined by the International Classification of Headache Disorders, 3rd edition (beta version) (15). None of them had ever had a history of epilepsy or head and neck neuralgia and their lack of cognitive impairment was screened by the mini-mental state examination (MMSE); also the research excluded from final sample any participant, who had experienced a history of addiction or headaches caused by a specific condition that was classified as secondary headache.
3.1. Assessments
The brief pain inventory (BPI): This questionnaire contained items that was designed to evaluate pain. The data from BPI divided two principal scores: a pain severity score and a pain interference score. Because the BPI is fast response, it has recommended useful clinical features by IMMPACT (16). This questionnaire has two scales: pain interference and pain severity.
I. Pain interference was assessed using the BPI. This scale has been identified as the gold standard for pain interference and assessed pain interference with a seven-item questionnaire that consists of seven numeric rating scales zero (no interference) to ten (the interference completely), related to physical interference and mood-related or emotional interference (17). Test-retest reliability showed good reliability for pain interference (r = 0.8). In the interference BPI scale, internal consistency was elevated (0.88 < α < 0.95) (18).
II. Pain severity was assessed using the BPI. This questionnaire is applicable as a common question for all types of chronic pain. This scale assessed pain severity on a 0 (no pain) to 10 (the worst pain imaginable) numeric rating scale (19). Based on this scale, patients examined least, worst, average, and their current pain intensity in the past 24 hours. Test-retest reliability showed good reliability for pain intensity (r = 0.8). In the severity BPI scale, internal consistency was elevated (0.81 < α < 0.89) (18).
Mindful attention awareness was assessed using the MAAS scale. Researches represented a high value internal consistency in these scales and Cronbach’s alpha was 0.82 (20).
3.2. Statistical Analysis Methods
Data were analyzed using SPSS V. 16. The data normality was examined by Kolmogrov-Smirnove test. Pearson correlation analysis and hierarchical linear regression were applied to determine the relationships of the variables.
4. Results
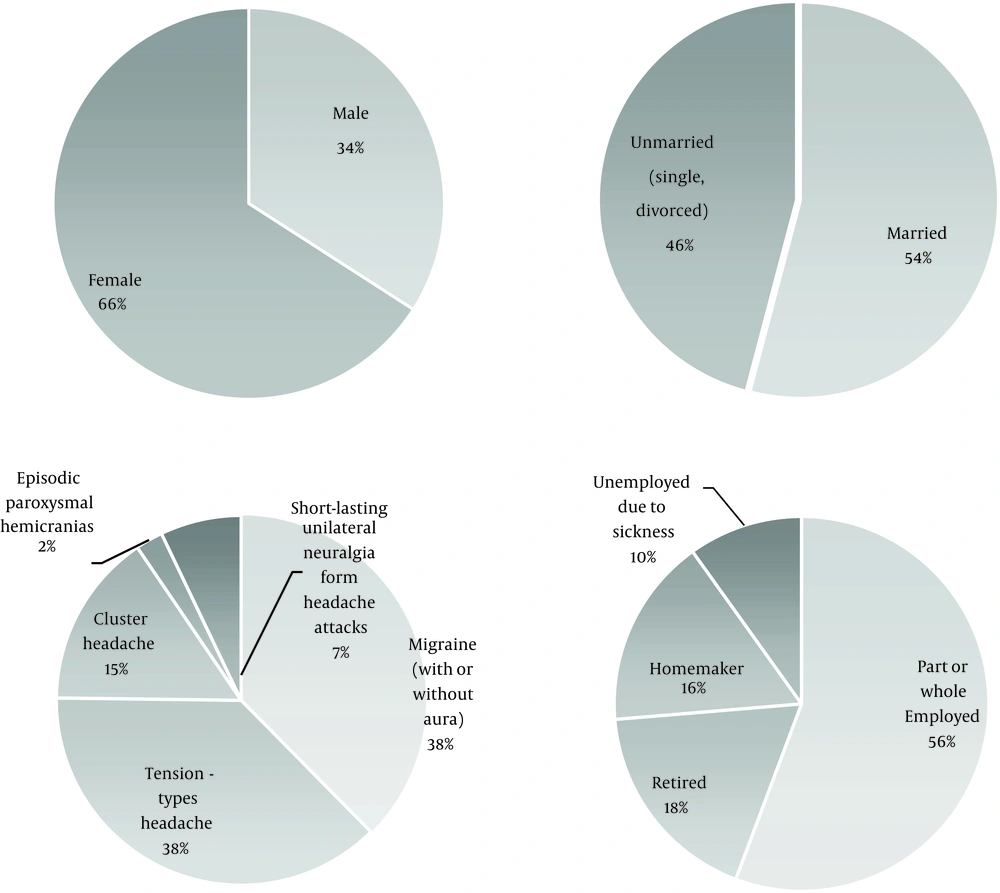
As shown in Figure 1, socio-demographic and descriptive statistics, indicate that 65.9% of the patients were women and 34.1% were men with a mean age of 37.24 years. Overall, 45.9% were single and 54.1% were married person with two levels of education including 37.6% non-academic and 62.4% academic graduate, who participated in the study (Figure 1).
4.1. Results of Pearson Correlation Analysis
The analysis showed that there was a strong negative correlation between pain intensity and mindfulness (P < 0.01 and r = -0.62), between mindfulness and activity interference (P < 0.01 and r = -0.33) as well as between mindfulness and emotional interference (P < 0.01 and r = -0.66).
Also, there were statistically significant positive relationships between pain intensity and physical interference (P = 0.002 and r = 0.33), and emotional interference (P = 0.002 and r = 0.35) (Table 1).
Means, Error Standards and Correlations for Research Variables
4.2. Regression Results
To specify the predictive relations and the contribution amount of two variable groups in explaining the headache activity and emotional interference, hierarchical linear regression was applied.
The pain intensity variable, which in the previous research was effective on pain interference, was analyzed as a control variable in the first stage. Mindfulness as well as other variables predicting variable regression analysis, was applied in the second stage. Physical interference and emotional interference were considered as dependent variables. The results of these analyzes are presented in the following tables.
By comparing the adjusted R square of the model 1 generated in horizontal column 1 with the adjusted R square of the model 2 generated in horizontal column 2, it is clear that adding mindfulness improves the model fit because the adjusted R square increases from 0.11 to 0.43 and the predictive power increased by 34% with the addition of mindfulness, which is an attention-focused cognitive processing. On the whole, these two variables (pain severity and amount of mindfulness) were able to predict 43% of the emotional interference with headache.
Based on Table 2, it was shown that pain intensity justifies 11% of the variance (adjusted R2 = 0.11), and a significant model appeared by adding MASS data: F (1, 83) = 44.38, P < 0.001 and the variance increased by 34% (R2 Change = 0.34). The recent model explains 43% of the variance (adjusted R2 = 0.43).
| Model | R | R2 | ΔR2 | Change Statistics | ||
|---|---|---|---|---|---|---|
| R2 Change | F Change | P Value | ||||
| 1 | 0.33 | 0.12 | 0.11 | 0.10 | 9.22 | 0.003 |
| 2 | 0.67 | 0.45 | 0.43 | 0.34 | 44.38 | < 0.001 |
Summary of Hierarchical Regression Model for Prediction of Emotional Interference
With two explanatory variables in the model, the regression line will be in the form of y = a + b1x1 + b2x2, where x1 is pain intensity and x2 is mindfulness. Substituting the variables and the unstandardized coefficients from the coefficients table, the equation for the model is as follows:
Emotional interference = 10.46 + (20 × pain intensity) - (15 × mindfulness)
The coefficients table shows that “mindfulness” with a standardized coefficient of 0.758 is a more significant predictor of emotional interference than “pain intensity” with a standardized coefficient of 0.335. Also, the standardized coefficients showed that both predictors are not of equal importance in predicting “emotional interference” (Table 3).
| Model | Unstandardized Coefficients | Standardized Coefficients | t | P Value | |
|---|---|---|---|---|---|
| B | S.E. | Beta | |||
| Step 1 | |||||
| Stability | 2.42 | 0.700 | 3.466 | 0.001 | |
| BPI (pain intensity) | 0.46 | 0.152 | 0.335 | 3.037 | 0.003 |
| Step 2 | |||||
| Stability | 10.46 | 1.32 | 7.881 | 0.001 | |
| BPI (pain intensity) | -0.20 | 0.157 | -0.151 | -1.326 | 0.001 |
| MASS × BPI (pain intensity) | -0.15 | 0.023 | -0.758 | -6.662 | 0.001 |
The Unstandardized and Standardized Regression Coefficients for the Variables Entered in the Model of Emotional Interferencea
In predicting the level of activity interference, hierarchical regression showed that the effect of the first stage variable (pain intensity) was significant in predicting the amount of the physical interference (P = 0.01). In the second stage, the predictive power was increased by 4% with the addition of mindfulness (R2 Change = 0.04). On the whole, these two variables (pain severity and amount of Mindfulness) were able to predict 10% of the physical interference with headache (adjusted R2 = 0.103), and these models in the prediction of pain interference with daily activities were not significant (P = 0.08). Although the severity of pain can predict headache interference with daily activities, separately (P = 0.01). However, in interacting with the mindfulness was not possible to such prediction and the interactive model is more important for us (Table 4).
| Model | R | R2 | Δ R2 | Change Statistics | ||
|---|---|---|---|---|---|---|
| R2 Change | F Change | P Value | ||||
| 1 | 0.298 | 0.089 | 0.076 | 0.089 | 7.089 | 0.01 |
| 2 | 0.357 | 0.127 | 0.103 | 0.040 | 3.196 | 0.08 |
Summary of Hierarchical Regression Model for Prediction of Physical Interference
These results indicate that mindfulness, which is attention-focused cognitive processing after control of pain intensity, explains 0.03% of total score changes (R2 Change = 0.039) in physical interference in patients with primary headache (P = 0.08 and ΔF (4 and 79) = 3.19, ΔR = 0.103).
The coefficients table showed that “Mindfulness” with a standardized coefficient of 0.256 and “pain intensity” with a standardized coefficient of 0.298 are not significant predictors of physical interference (Table 5).
| Model | Unstandardized Coefficients | Standardized Coefficients | t | P Value | |
|---|---|---|---|---|---|
| B | S.E. | Beta | |||
| Step 1 | |||||
| Stability | 2.35 | 0.714 | 3.293 | 0.002 | |
| BPI (pain intensity) | 0.413 | 0.155 | 0.298 | 2.66 | 0.01 |
| Step 2 | |||||
| Stability | 5.087 | 1.68 | 3.02 | 0.003 | |
| BPI (pain intensity) | 0.185 | 0.199 | 0.133 | 0.929 | 0.05 |
| MASS × BPI (pain intensity) | -0.052 | 0.029 | -0.256 | -1.788 | 0.05 |
The Unstandardized and Standardized Regression Coefficients for the Variables Entered in the model of Physical Interference
5. Discussion
Ideally, the type of pain interference in clients is one of the most important dimensions for planning treatment and determining the method of intervention.
The research question asked whether there is a difference in the effect of mindfulness and pain intensity on two types of pain interference (emotional and physical interference).
Analysis of data revealed that the mindfulness feature considerably influences emotional interference. Therefore, the answer to the research question is affirmative, and the first null hypothesis is rejected.
Based on the present descriptive study, there is a difference in mindfulness feature and pain severity composite in predicting two types of pain interference.
This finding supports previous studies that claim for the efficacy of mindfulness on emotion regulation (21).
The findings also lend support to the previous studies which have demonstrated the benefits of mindfulness for pain interference in the whole pattern (22).
Cleeland and Ryan (23) found that distinguishing different types of pain interference was more effective to choose the appropriate treatment.
The findings can be summarized that aforementioned variables (emotional and physical interference) correlated with pain intensity. Also, these findings contained important knowledge about emotional interference in people with primary headache in the patients, whose headache pain often have interfered with their mood, sleep, the pleasure concept, and interpersonal communication.
Results also indicated significant and positive relationship between pain severity and pain activity and emotional interference.
Results about emotional interference in the current study were in proportion to some researches. For example, Ortner et al. in 2007 (19) demonstrated that mindful awareness is correlated with lower emotional pain interference, while the result of Day et al. in 2014, showed meditation mindfulness reduced pain severity and pain interference in patients with primary headache (12). Recently, other results from cross-sectional survey of Senders et al. in 2018 suggested a clinically significant association between mindfulness and pain interference in chronic diseases (24).
In the current study, mindfulness in comparison with pain severity had a considerable prediction in emotional interference. With regards to evidence that confirmed mindfulness leads to emotion regulation in the central nerve system (25, 26) and with attention to negative correlation between emotional interference and mindfulness, can be assumed that, the likely low level of mindfulness in patients playing a major role in disrupted attention and led to negative emotions and movement towards emotional interference.
Along with previous studies and in explaining the results of this study it could be said that in patients with chronic pain, automatic though and critical emotions about pain were more available and individuals, who not are mindful, absorb into their worries emotions and thinking about their unresolved life problems. In such circumstances in pain experience, the person’s mood falls down (27).
Patients with more mindful awareness could better decouple their focus from pain-related negative emotions and have less emotional interference with pain (28). Also, this can be explained by the fact that sustained attention due to mindful awareness has caused less negative cognitions and emotions about self, word, and others, and then the better mood in persons caused to less emotional interference with pain (28).
The present study confirms previous findings and contributes additional evidence that suggest both emotional and physical interference should be taken into account distinctly in pain management.
The results of the present study suggest that application of mindfulness-based interventions presumably results in better performance in emotional interference than physical interference.
The results are a clear rebuttal of the claims that attention focused state impacts physical interference in the chronic pain population (29).
The fact that physical interference did not predict mindfulness and pain severity is important in showing that mindfulness is not sufficient for decreasing physical interference.
Such different results showed that in these cases, mindfulness is not sufficient for coping with pain interference with daily activities. This result is parallel with longitudinal cohort study of Oosterling et al. (30).
Also, the researchers found that there was a strong and positive relationship between pain severity and pain interference. Pain severity works in contrast to well-being and similar to the current findings, positive relationship between pain severity and pain interference is supported by evidence from previous studies (30, 31).
As mentioned earlier, mindfulness influences pain perception (32), and some parallels can be drawn between the current study and Lima’s research in 2014 (33) as well as the results that de Jong (13), and Day et al. have achieved; they concluded that reduction in pain severity leads to a reduction in pain interference (34). In other words, baseline pain intensity significantly mediated the motivation for treatment and pain interference in their clinical trial.
The present study cleared the points of pain interference type that may help choose the appropriate medical and psychosocial treatment in people with primary headache. This was one of the advantages of this study compared to previous studies; because this study provides the rationale for consideration of pain interference type in empirical trials, thus, it is recommended to use a mindfulness-based intervention for reducing emotional interference in populations with chronic pain.
Although a number of clinical recommendations and robust implications can be placed fourth in accordance with the findings of this study, it should be noted that the implications gleaned from this research must be treated with caution because chronic pain is a complex phenomenon and benefits cannot be considered without giving due attention to a myriad of variables.
However, the current findings add substantially to the understanding of pain interference. An implication of these findings is that both emotional interference and physical interference should be taken into account in pain management, and taken together, these findings do not support recommendations to application of mindfulness-based intervention to physical pain interference.
Though this study provides evidence that mindfulness plays a significant role in emotional pain interference, the reader should note its limitations and ways, in which future research might be enhanced. First, this study was conducted with a small group of people with primary headache. Additional studies with greater number of patients are needed to fully understand the effect of mindfulness and pain severity in prediction of pain interference. A second limitation of the study is that only two predictive variables were used in the study. In future studies, application of different types of variables will shed light on the differential effects of other variables on two types of pain interference. A third limitation was that all types of primary headache were used in the present study while the focus on a specific type of headache could have been more clarifying about above-mentioned statistical prediction.
Further research, which looks at the amount of mindfulness effect on emotional interference in other chronic pain is therefore needed.
5.1. Conclusions
In conclusion, the current study suggests important points to the significant role of mindful awareness in pain-related emotional interference management.
The main conclusion to be drawn from this study was the importance to distinguish between types of pain interference and considering this distinction in choosing appropriate treatments for chronic pain management. In addition, this result can explain the role of mindfulness and attention-focused cognitive processing in adjustment to headache.