1. Background
Intrathecal injection of plain local anesthetic solution demonstrates a rapidly profound nerve block (1). Although this is an easy and safe anesthetic technique, the greatest challenge is to control the spread of local anesthetics through the cerebrospinal fluid (CSF), sometimes producing a block that is insufficient due to narrow spread, resulting in additional anesthesia or change in anesthesia.
Predicting anesthesia spread based on a given dose of local anesthetic is challenging owing to the marked variability between individual patients (2). The physical characteristics of CSF, such as volume and density, can influence the spread of spinal anesthesia (3). However, it is not practical to preoperatively measure these values in each patient using magnetic resonance imaging. While some patient characteristics that are known before anesthesia, including age, height, and weight, may help determine the spread, linear regression analyses have revealed that these variables have low predictive value (4). In contrast, the handle direction of the needle and the tip position in the subarachnoid space can affect the sensory level of spinal anesthesia (5). Spinal anesthesia is commonly performed at the presumed L3 - L4 vertebral interspace in reference to Jacoby’s line. However, the needle is inserted either one space too high or one space too low in 30% - 70% of the patients (6, 7). One study demonstrated that spinal anesthesia may reach as high as T1 with injection at the L2 - L3 space, but only as high as T6 with injection at L4 - L5 (8). Ultrasound imaging may identify the correct level in as many as 80% of cases, but this requires more time and effort (7, 9). Therefore, several patient and anesthesiologist-related factors contribute to the extent of spinal anesthesia, and make the prediction of anesthetic levels challenging.
Anesthesiologists often focus on the objective assessment data involving physiological monitoring, radiographic imaging, and laboratory examinations, as well as clinician-reported outcomes before and after anesthesia. Recently, clinical trials evaluating medical treatments have increasingly incorporated self-reported measures from patients, often referred to as patient-reported outcomes (PROs) (10), which have important roles in various clinical trials.
Patients usually describe initial subjective sensory changes (ISSCs) as a warm sensation and numbness in their low back or lower extremities during or just after injection (11). We hypothesized that patients promptly notice the effects in the dermatome of the sensory nerve affected by local anesthetic solution and ISSCs at lower dermatomes are indicative of a narrower spread of anesthesia.
2. Objectives
The present study aimed to (1) assess the relationship between ISSCs (as PROs) and anesthesia spread and (2) examine the relationships between ISSCs and other factors that could contribute to anesthesia spread, including patient characteristics and the time course of anesthesia, using multi-level analyses.
3. Methods
3.1. Participants
The study was approved by the Toshiba Rinkan Hospital Ethics Committee and written informed consent was obtained from each patient. This trial was registered in the University Hospital Medical Information Network (Unique ID issued by UMIN: UMIN000013334). Additionally, this study followed the appropriate Enhancing the QUAlity and Transparency of health Research (EQUATOR) reporting guidelines.
The participants were 120 consecutive in-patients, with American Society of Anesthesiologists physical status I and II, scheduled for open repair surgery of inguinal hernias under spinal anesthesia. Patients were eligible for inclusion if they were ≥ 20 years of age and capable of proper self-assessment. We excluded patients with chronic pain or neurological disorders in their lower back and lower extremities that could affect anesthetic assessment, obvious spinal postural abnormalities, previous spinal surgery or treatment with intrathecal injection, and any contraindication to the neuraxial blockade.
3.2. Procedures
Following an examination of vital signs with standard monitors (three-lead electrocardiography, pulse oximetry, and noninvasive blood pressure) in the supine position, intravenous access was established in the forearm to infuse lactated Ringer’s solution at 10 mL/kg/h during spinal anesthesia. The patient was then placed in the left lateral decubitus position. The L3 - L4 intervertebral space was identified using the Jacoby line (the line between the top of the bilateral iliac crests), and then infiltrated with 2% lidocaine. Lumbar puncture was performed at the midline of L3 - L4 using a 25-gauge pencil-point needle (Unilever®, Unisis Corp., Japan). On reflux of clear CSF, 3 mL of isobaric 0.5% bupivacaine (0.5% Marcaine®, AstraZeneca, Japan) was injected at a rate of 0.25 mL/s into the subarachnoid space through a needle oriented with the orifice facing in the cephalad direction. The patient was immediately turned to the supine position and remained horizontal until the completion of surgery.
After at least 20 minutes of observation, surgery was performed under sedation with a continuous intravenous infusion of 1 - 2 mg/kg/h of propofol, as well as a face mask administration of 5 L/min of oxygen if the upper dermatome level of sensory loss was at or above T12. Patients who reported intraoperative pain were treated with an intravenous bolus of fentanyl, inhalation of sevoflurane, or infiltration of a local anesthetic in the surgical field. The selection of the type and dose was based on the attending anesthesiologist.
3.3. Outcomes
Blood pressure and heart rate were measured automatically at least every 5 minutes. The ISSCs in the dermatomeduring or after intrathecal injection was assessed via patient interviews (12). The elapsed time from the start of intrathecal injection to the ISSCs was also recorded. The ISSCs were based on the patient reports of sensation changes in the skin (PROs). We instructed patients to verbally indicate when they began to feel sensations such as warmth, numbness, or dysesthesia in their lower back or lower extremities during or after injecting local anesthetics, to remember the skin site where the sensation was noticed, and then to indicate the location with their finger immediately after returning to the supine position.
The extent of sensory loss to pinprick (pain) and ice (cold) was examined on the anterior midline of the body at 5-minutes intervals for 20 minutes after intrathecal injections. We used a plastic container filled with ice to assess the loss of cold sensation and a blunt needle to assess pain sensation. Motor block of the lower extremities was evaluated using the Modified Bromage Scale (0, full movement; 1, inability to raise extended leg; 2, inability to bend the knee, can flex ankle; 3, inability to bend ankle) at time intervals identical to the sensory block examination.
Patients were unaware of the relationship between the ISSCs and the anesthetic effect. A technician skilled in intrathecal injections asked each patient to report the site of ISSCs. The experienced assessors were blinded to ISSCs in the dermatome, as well as to the patient characteristics.
3.4. Statistical Analyses
The spread of sensory loss, as measured by segmental dermatomes, was predicted to be consistent with the results of previous studies. The sample size was calculated based on a one-sample comparison of continuous variables to hypothesized values from 11.4 ± 2.5 to 15.3 ± 3.4 segments, as demonstrated in previous studies (13, 14). A difference of 1 - 3 segments was considered clinically relevant. The number of participants required for a power of 80% using a two-sided alpha of 0.05 to detect a difference of 1 - 3 segments ranged from 8 to 99. Power analysis can calculate the minimum sample size required to reasonably detect an effect under given conditions. We predicted an attrition rate of 20% - 30%, and thus recruited 120 participants for this study.
Multi-level linear regression analysis was used to identify factors associated with PROs, specifically the ISSCs. The random effect was allowed for a random parameter of slope and intercept. Interpatient reliability was estimated using an intraclass correlation coefficient (ICC). The proportion of variance at each level was also assessed by ICC.
Two-sided P values of < 0.05 indicated statistical significance. All statistical analyses were performed using Stata/MP version 14.2 (Stata Corp., College Station, TX, USA).
4. Results
Patients characteristics are reported in Table 1. Reflux of clear CSF was noted in all 120 patients. All patients reported the site of ISSCs following the injection of local anesthetic solution. The elapsed time to ISSCs (onset) was 9 (4, 18) seconds [median (minimum, maximum)]; 116 (96.7%) patients indicated ISSCs during intrathecal injections (within 12 seconds after the beginning of injections) and the remaining 4 patients indicated ISSCs after intrathecal injection (within 18 seconds and within 6 seconds after the end of injections). In 66.7% of the patients, ISSCs occurred in the L1 - L5 dermatomes.
| Patients’ Characteristics | |
|---|---|
| No. | 120 |
| Male gender, No. | 109 (90.8) |
| Age, y | 68 (21 - 86) |
| Height, cm | 165 (144 - 189) |
| Weight, kg | 62 (40 - 91) |
| ASA category | |
| I | 62 (51.7) |
| II | 58 (48.3) |
| Therapy information | |
| Initial subjective sensory change | |
| Onset (time to sensory change, s) | 9 (4 - 18) |
| Dermatome | |
| L1 - L5 (anterior surface of lower extremity) | 80 (66.7) |
| S1 - S2 (posterior surface of lower extremity) | 32 (26.7) |
| S3 - S4 (perianal) | 8 (6.7) |
| Side | |
| Left | 25 (20.8) |
| Right | 71 (59.2) |
| Bilateral | 24 (20.0) |
| Number of patients with intraoperative pain | 3 (2.5) |
| Number of patients who stopped therapy during the study period | 0 (0) |
| Number of patients with missing values | 0 (0) |
Patient Characteristics and Therapy Informationa
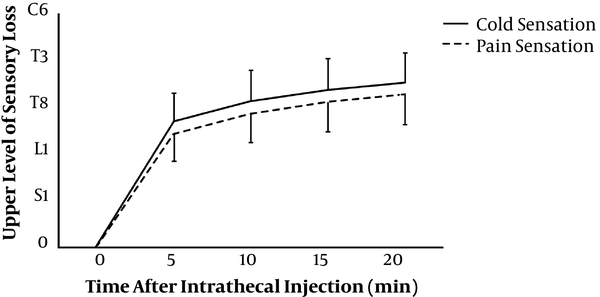
The preoperative levels of sensory loss to pinprick and ice stimuli appeared to increase progressively during the 20-minutes period (Figure 1). Three patients experienced pain during the early intraoperative period and required additional anesthesia. These patients, who experienced ISSCs in sacral dermatomes S2 - S4, did not experience sensory loss at levels higher than T10 after 20 minutes of intrathecal injection.
Table 2 presents data from the multi-level analyses, describing the spread of sensory loss for pain and cold sensations following spinal anesthesia. Higher height and mean blood pressure (MBP) values, as well as faster onset, lower dermatome, and left-sided ISSCs, were significantly correlated with less sensory loss. A lower dermatome was the most important indicator (P < 0.001) among factors affecting ISSCs. The proportional change in variance was 35.7% for pain and 50.3% for cold; therefore, the goodness of fit was superior in the model. Significant differences were observed in the analyses of individual data, as indicated by Z-scores of > 2. Additionally, both variances of intercept and slope were significant, indicating variability between individuals. Furthermore, higher ICC values indicated the greater influence of intraindividual variability.
| Sensation of Pain | Sensation of Cold | |||||
|---|---|---|---|---|---|---|
| Coef. | SE | P Value | Coef. | SE | P Value | |
| Time, min | ||||||
| 0 | Reference | Reference | ||||
| 5 | 5.595 | 1.457 | < 0.00 | 6.426 | 1.397 | < 0.001 |
| 10 | 7.425 | 1.469 | < 0.001 | 8.354 | 1.408 | < 0.001 |
| 15 | 8.570 | 1.473 | < 0.001 | 9.470 | 1.412 | < 0.001 |
| 20 | 9.251 | 1.480 | < 0.001 | 10.166 | 1.418 | < 0.001 |
| Gender | -0.273 | 0.420 | 0.27 | -0.473 | 0.428 | 0.52 |
| Age | 0.008 | 0.011 | 0.89 | -0.002 | 0.012 | 0.48 |
| Height | -0.058 | 0.022 | 0.005 | -0.062 | 0.022 | 0.007 |
| Weight | 0.008 | 0.017 | 0.54 | 0.011 | 0.018 | 0.66 |
| ASA | -0.229 | 0.239 | 0.35 | -0.229 | 0.243 | 0.34 |
| MBP | -0.021 | 0.008 | < 0.001 | -0.029 | 0.008 | 0.009 |
| Heart rate | -0.004 | 0.010 | 0.55 | -0.006 | 0.010 | 0.69 |
| Modified bromage scale | ||||||
| Grade 0 | Reference | Reference | ||||
| Grade 1 | 0.105 | 1.310 | 0.97 | -0.046 | 1.253 | 0.94 |
| Grade 2 | 0.171 | 1.305 | 0.90 | 0.158 | 1.250 | 0.90 |
| Grade 3 | 0.679 | 1.321 | 0.72 | 0.459 | 1.265 | 0.61 |
| Initial subjective sensory change | ||||||
| Onset | 0.161 | 0.061 | 0.002 | 0.180 | 0.059 | 0.008 |
| Dermatome | 0.614 | 0.065 | < 0.001 | 0.719 | 0.063 | < 0.001 |
| Side | ||||||
| Left | Reference | Reference | ||||
| Right | 1.435 | 0.311 | 0.001 | 0.987 | 0.300 | < 0.001 |
| Bilateral | 0.127 | 0.384 | 0.42 | -0.298 | 0.371 | 0.74 |
| Constant term | 11.541 | 3.234 | < 0.001 | 13.751 | 3.287 | < 0.001 |
| Random-effects parameter | ||||||
| Var (time) | 0.012 | 0.002 | < 0.001 | 0.010 | 0.002 | < 0.001 |
| Var (constant term) | 0.696 | 0.196 | 0.20 | 0.818 | 0.212 | 0.44 |
| Var (residual) | 1.396 | 0.097 | < 0.001 | 1.257 | 0.088 | 0.001 |
| Z-score | 3.6 | 3.9 | ||||
| ICC, % | 33.3 | 39.4 | ||||
Multilevel Analysis of Pain and Cold During 20-Minutes Observationa
5. Discussion
Our findings suggest that the dermatome and time to the onset of ISSCs could predict the spread of spinal anesthesia with plain local anesthetic solutions. Early patient reports of ISSCs in the perianal area (S2 - S4) may produce insufficient anesthesia and analgesia. The clinical importance of this prediction is emphasized by the fact that minimal time and effort are required for judgment and it is a non-invasive assessment for patients; a short interview during anesthesia occurs, no other medical practice is added, and the judgment is completed by the time the injection ends.
Considering the time course of anesthesia, the current multi-level analysis revealed that MBP and height could predict the level of anesthesia, which had not been reported earlier. However, ISSCs were the strongest predictors. Therefore, the PROs are useful for evaluating spinal anesthesia.
Puchalski and Morison reported that the mean time to the onset of ISSCs was 34 + 2 seconds (11). They performed spinal anesthesia for the caesarian section using 2.5 mL of 0.5% plain bupivacaine although they did not describe the injection method and sensory symptoms in detail. We instructed patients to identify the site of ISSCs as soon as possible and repeatedly asked patients whether sensations in the leg, hip, or lower back had changed during the injection of 3 mL of 0.5% plain bupivacaine. The differences in protocol, including a prior description of ISSCs, type of spinal needle, and dose of local anesthetics between the two studies may have produced differences in the onset of ISSCs.
In the present study, the multi-level analysis revealed a highly significant correlation in the cephalad level between ISSCs and sensory loss (anesthesia). In patients for whom ISSCs occurred in the perianal area (S2 - S4 dermatomes), further studies are needed to examine whether strategies such as altering the direction or position of the needle (5, 8) or increasing the dose of local anesthetic (15) are necessary. Patients with obvious spinal postural abnormalities and previous spinal surgery were excluded from the present study. In all patients, except three who experienced intraoperative pain, complete anesthetic spread and analgesia occurred. Therefore, the position of the needle or inadequate flow of local anesthetics was the possible factors contributing to the ISSCs observed in the S2 - S4 dermatomes.
The early onset of ISSCs is associated with reduced anesthesia spread. Insufficient anesthesia may be noticed more rapidly than sufficient anesthesia; thus, failure can easily be prevented if patient self-reporting is utilized. If ISSCs occur after completing the injection of a local anesthetic, there is a high possibility of achieving successful anesthesia. Regarding the injection of local anesthetic into the subarachnoid space, the unidirectional flow concentrating in a small part of the nerves may lead to the rapid onset of ISSCs, but not for the entire diffusion (delay of onset) (5, 16).
This is the first study investigating the regions in the lower back and lower extremities where the ISSC onset occurs initially following spinal anesthesia. Local anesthetic solutions within the subarachnoid space can block sympathetic nerve fibers, resulting in vasodilation and elevated skin temperature in the legs, which may produce a warm sensation. However, skin temperature measurements and thermography have demonstrated marked temperature elevations only in the feet and a negligible change above the ankle (17, 18). In contrast, ISSCs occurred in other parts of the foot. Additionally, during spinal anesthesia, the time to a detectable rise in skin temperature (> 1°C) may be approximately 3 minutes (18), whereas ISSCs may occur within 20 seconds. Therefore, we hypothesize that ISSCs originate in the sensory nerve fibers that are exposed to local anesthetics in the subarachnoid space and dysesthesia or paresthesia originates in the sensory nerves.
ISSCs were reported on the right side of the body 3 times more often than on the left side. The cauda equina, including the sensory nerve fibers, moves dynamically in the subarachnoid space with changes in body position (19). The cauda equina is, therefore, shifted to the left side (the floor side) of the subarachnoid space by gravity when a patient is placed in the left lateral decubitus position. We propose that a local anesthetic solution injected at the midline is likely to affect sensory nerve fibers on the right side, possibly leading to increased ISSCs on the right side.
Our study has some limitations. First, to the best of our knowledge, no previous study had investigated the site and onset of ISSCs. Therefore, we did not prepare a control group in this pilot study. Second, without fluoroscopy, it was not possible to be certain that all intrathecal injections occurred at L3 - L4. Hence, correlations between the intervertebral level, ISSCs, and the spread of anesthesia could not be demonstrated. We intend to prepare a general clinical setting to assess ISSCs while considering bias due to the injection site. We also predict that ISSCs may correspond to different interspaces and variance in anatomy. Third, we selected patients with inguinal hernia, most of whom were older men. This factor may have a significant effect on our results. Further studies with larger populations and more varied patients are, therefore, required.
In conclusion, the multi-level analyses considering the time course of anesthesia showed that ISSCs reported by patients following intrathecal injection of isobaric bupivacaine are major predictors of subsequent anesthesia spread. Although patient height and MBP after intrathecal injection also predicted the extent of anesthesia, ISSCs were the most important predictors. The present study demonstrated that lower dermatomes, faster onset, and floor side of ISSCs were associated with less sensory loss.