1. Background
Chronic pain is the most suffering mind-body condition. The standard medical approach is still based on Descartes’s theory that does not work for many complicated conditions such as chronic pain (1). Among different types of pain, the headache is one of the most typical symptoms that causes patients come to clinics (2). After identifying the medical defect in headache management, there are growing numbers of people who have tendency to complementary and multi-dimensional therapies (3). But, even now, research is evolving to discover the role of mind and body in such treatments.
Ever since Melzak launched his widely known hypothesis about pain (4), scholars have discussed the relative competency of psychological and cognitive aspects in pain perception. Drawing on technology such as functional MRI, researchers conclusively investigated psychotherapies to alleviate pain (5, 6). In parallel with these studies, scholars have found an inherent overlap between neural networks involved in chronic pain and brain regions involved in attention mechanisms (7). The aforementioned evidence organizes a deep argument for identifying the importance of cognition (as the intermediate mechanism) in pain perception. In recent years, there has been considerable interest in the role of top-down attention-centered processes in pain control (8). These important studies on pain have found that attentional processes and cognitive components can change the way that painful stimuli are explicated by the brain and consequently have provided persuasive resources that cognitive psychotherapies have tremendous potential in the management of chronic pain (9).
Recently, in a new framework, a model of pain management has hypothesized that there is an important role in central attentional processes in the brain for pain. This model proposes that psychotherapies primary affect cognitive content and cognitive process in chronic pain control (10).
In pain management, mindfulness-based cognitive therapy (MBCT) is one of the innovative psychotherapies recently applied to chronic pain management (11) and preliminary evidence supports this approach (predominantly compared with inactive control conditions) for headache management (12). The MBCT protocol successfully targets the key cognitive mechanism because MBCT combines cognitive behavioral therapy with mindfulness-based techniques to produce an integrated method that could virtually lead to synergistic results (13). Because of its integrated nature, MBCT has the potential to improve upon the outcomes reported with subgroup approaches (CBT, MBSR). MBCT has been found to target pain catastrophizing, pain acceptance, and headache management self-efficacy (12).
Preliminary evidence has indicated that this method is acceptable, feasible, and well-tolerated and compared to TAU control conditions, is effective for pain management (13). However, the mechanisms through which these changes occur are still vague. A major defect in much of the empirical research using MBCT is that, most of them have only focused on cognitive content, and taken together, inquiry research about the pain-related cognitive processing has been neglected. Unless patients adopt appropriate cognitive processing, longstanding enhancement will not be attained. In order to analyze that how psychotherapies such as MBCT work, we need for the examination of mechanisms through which the MBCT affects chronic pain, including pain-related cognitive processing.
There is considerable ambiguity about the cognitive process during MBCT. Surely, the reason for this overlooked aspect is the lack of an integrated tool that incorporates different types of cognitive processing during pain experience.
Recently, based on a content review of attentional processing during pain perception and with the aim of providing a pure assessment of the pain-related cognitive process, Day et al. defined four categories of pain-related cognitive processes (14), as follows:
1. Pain diversion: This kind of cognitive processing includes attempts to divert attention from the pain (with clauses like, I divert my attention away from the pain to something else).
2. Pain distancing: It includes considering pain sensations, but with re-explaining to make them distant from oneself (Dissociate) or reinterpreting the pain more positively (Reappraisal) (with clauses like, I think about the pain in a different way so that it is more bearable).
3. Pain openness: This processing style involves two distinct adaptive attention processes; “Non-Judgment” processing or non-reactive and non-judgmental monitoring about pain sensations and “acceptance processing” or pain acceptance (with clauses like, I am aware of my pain but do not see it as good or bad).
4. Pain focus: Pain focus processing style involves two distinct processes; absorption or voluntary attentional focus and rumination or more-or-less involuntary attention focus on pain (with clauses like, I pay close attention to the pain I am experiencing) (15).
So far, no study has examined pain-related cognitive processing during MBCT and other psychotherapies.
There is yet no research evaluating pain-related cognitive processing during MBCT intervention in a randomized controlled trial (RCT). The complicated analysis of research evidence showed that the psychotherapies are nearly twice as effectual as “nonspecific” or placebo treatments, which seek to induce positive expectations in clients (16). Based on the cognitive approach, the therapeutic connection between the therapist and the client is one of the prerequisites for treatment (16). to obtain pure therapeutic results, such therapeutic relationships should be deleted from final outcomes.
Some researchers declare that the psychosocial treatment research should not only depend on the traditional design of psychotherapy group versus delayed or waitlist control group, but should comprise an attention placebo control (APC) arm to evaluate the specific effects of intervention (17). However, no scholars have designed to examine on a properly controlled trial into the accurate MBCT efficacy.
2. Objectives
On the basis of MBCT’s theory of chronic pain and the current key points mentioned above, we designed an RCT to compare MBCT with an APC group in a headache pain population. The objectives of this study were to (a) assess the net and specific effect of MBCT on pain outcome with deduction attention placebo effect and (b) measure the effect of MBCT on pain-related cognitive processing from baseline to follow-up.
3. Methods
3.1. Study Design and Sample
This was a randomized single-blind study with parallel design, comparing MBCT with an APC group in a sample with primary headache.
This study was conducted in 2017 - 2018 in Emam Hossein Hospital in Tehran province. The statistical population included 210 patients with chronic headache, referring to hospitals and clinics in Tehran city, Iran. Using a purposive sampling method from among 210 people with primary headache, after removing those who were inconsistent with the inclusion criteria, 85 participants were selected (by a neurologist). Then, via a web-based random number sequencer (http://www.randomizer.org) participants were randomly assigned into two groups: MBCT (43 patients) and APC (42 patients). Next, participants completed a baseline assessment. A clinical health psychologist evaluated patients at three stages (baseline, posttest, and follow up).
The study inclusion criteria were age of 19 years or older, having a headache experience at least for three days per month (for more than three months) due to a primary headache (diagnosed based on the International Classification of Headache Disorders, third edition (beta version) (16), Reading and writing skills to understand and complete worksheets, and any secondary factor that was the cause of the headache (in order to distinct secondary headache diagnosis).
The study exclusion criteria included a history of epilepsy, facial or neck neuralgia, the cause of the headache being a factor such as addiction, intracranial mass or another condition, cognitive impairment screened by the Mini-Mental State Examination (MMSE), engaging in other psychotherapies for pain condition, diagnosis of personality disorder, and affective disorder, schizophrenia, and seizure disorder not managed enough by psychiatric medicines and current drug use.
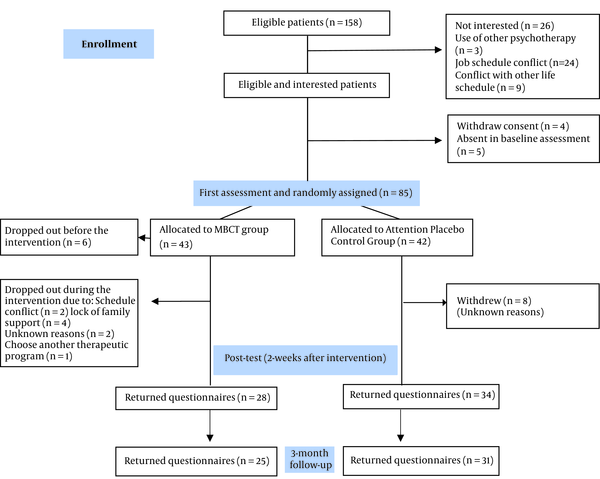
This research was approved by the Ethics Committee of the Alborz Islamic Azad University of Medical Sciences in Iran (ethical code: IR.IAU.K.REC.1397.26 and pre-registered at https://www.irct.ir/ [IRCT registration number: IRCT20141012019511N4]). Figure 1 represents the CONSORT diagram, which describes the RCT design (18).
3.2. Procedures
Recruitment lasted from December 2017 to June 2018. Eligible and interested participants after completing consent forms and baseline questionnaires (first step) were assigned via a web-based random number sequencer (http://www.randomizer.org) into MBCT or APC groups. At the posttest and follow-up, questionnaires were administered two weeks after (second step) and three months after (third step) the eight-week intervention. In the MBCT group, six participants dropped out before the intervention, nine participants dropped out during the intervention, and three participants dropped out before the follow-up. Therefore, 25 participants completed the questionnaires three months after the eight-week intervention. In the control group, eight participants dropped out before posttest and three participants dropped out before the follow-up. Therefore, 31 participants remained in this group and completed the questionnaires at follow-up. Figure 1 shows the CONSORT diagram (18).
3.2.1. MBCT and Attention Placebo Control Group
3.2.1.1. MBCT Group
The MBCT intervention comprised 8 weekly, 2-h sessions with 11 to 15 participants (n = 43) and one therapist who was superior in MBCT.
In MBCT, the first half of the protocol focused on the preferment of awareness of patients about mind default mode; then, in the second half of treatment, enhanced awareness converted to automatic skills and patients learn to choose intentionally to respond to their experiences rather than to react.
Every session included practical techniques, guided inquiry, and discussion between individuals. Participants were encouraged to meditation practice as homework, during the week and between the sessions. Other CBT and mindfulness components were also assigned for homework. treatment details are presented in the clinical manual and guide. Table 1 presents a brief sessions’ description of MBCT for chronic pain (13).
| The Order and Session’s Title | Brief Session’s Description |
|---|---|
| Session 1: stepping out of automatic pain habits | This session included psychoeducation about the Gate Control Theory, awareness and learning about automatic pilot, and guided inquiry around these topics. The first formal meditation, the body scan, was used to begin training the mind to have the capacity to move attention at will. Finally, the three‐minute breathing space was taught as a means to further generalize the practice. |
| Session 2: facing the challenge | One focus of this session was to continue to enhance the client’s awareness of the connection between stress, thoughts, pain, and functioning through CBT‐oriented exercises. Getting rid of the perceptions that were automatically connected to these inefficient patterns was taught through mindfulness meditation. |
| Session 3: the breath as an anchor | In this session, further training was provided to understand the aspects of the pain-stress model through the practice of “Stressful Experiences Diary”, and the usual functions of the body (such as breathing) were introduced as means for the separation from negative stress-related thoughts. |
| Session 4: learning to stay at present | In this session, thinking related to stressful experiences was examined by the practice called “Unhelpful Habits of Mind” and clients learned, when thoughts or difficulties seem “too much”, bringing awareness to the body in mindful movement and mindful walking as a way to step out of their heads and into their bodies, tuning into the contrasts between stillness and movement. Both of these techniques were taught in this session. |
| Session 5: active acceptance | In this session, the process of acceptance was introduced as a way to actively train how to learn to stay with experiences, without a need to rush in and try to immediately change it, push it away, or hold on to it. |
| Session 6: seeing thoughts as just thoughts | The core theme of this session was to learn how to see thinking as just thinking, with thoughts ultimately being simple secretions of this thinking mind, not facts, and not the truth. |
| Session 7: taking care of myself | The emphasis of this session was on the development of a mindfulness maintenance plan for on‐going self‐care following the conclusion of the program. |
| Session 8: harnessing the power of the mind for chronic pain management | In this session, a discussion of the take‐home activity targeted identifying red flags for stress and pain flare‐ups and identifying options of nourishing activities, and using these was as a way to prevent relapse following the program. |
Brief Sessions Description of MBCT for Chronic Pain
3.2.1.2. APC Group
In the APC group, during 8 weekly, 2-h sessions, participants received attention and therapist’s empathy and participated in group discussion. As is usual in social research (19, 20), a rational therapeutic approach was provided in the APC group. The rational information presented in the APC group was to understand the importance of receiving social support in pain management, as well as the importance of receiving the experience of other people with similar pain and emphasis on finding a consultative solution to a problem with common ground.
3.3. Assessments
3.3.1. Brief Pain Inventory
It is a self-administered questionnaire designed to assess pain. The Brief Pain Inventory (BPI) gives two main scores including a pain severity score and a pain interference score. Because the BPI is quick to answer, it has demonstrated good clinical properties and is recommended by IMMPACT (21).
I. Pain interference was assessed using the BPI. This scale has been identified as a golden standard for pain interference. Test-retest reliability showed it good reliability (r = 0.8). Internal consistency of the BPI was high for the interference subscale (0.88 < α < 0.95) (22).
II. Pain severity was assessed using the BPI. This questionnaire was used as a generic pain questionnaire for other chronic pain conditions. This scale assessed pain severity on a numeric rating scale from 0 (no pain) to 10 (the worst pain imaginable) (22). In this scale, participants evaluated least, worst, average and their current pain intensity in the past 24 hours. Test-retest reliability showed its good reliability (r = 0.8). The internal consistency of the BPI was high for the severity scale (0.81 < α < 0.89).
3.3.2. Pain-related Cognitive Processes Questionnaire
This questionnaire with 53 items mixed the questions of four different styles of cognitive processing about pain or four composite scales, including pain diversion, pain focus, pain distancing, and pain openness as developed by Day et al. (15). This questionnaire is scored based on a 5-point Likert scale and includes the degree to which persons respond cognitively to pain. The composite scales have acceptable internal consistency, high test-retest reliability, and convergent validity (23). In composite scales, Cronbach’s alpha was high for pain diversion (0.92), pain focus (0.91), pain distancing (0.90), and pain openness (0.78) (23). In the present study, the amount of content validity was 0.79 and Cronbach’s alpha was high for pain diversion (0.89), pain focus (0.99), pain distancing (0.77), and pain openness (0.87).
3.4. Statistical Analysis
To measure changes related to treatment, participants were evaluated at three stages from the onset of treatment (pretest) to the end of the eight weeks (posttest) and three months after the eight-week intervention (follow-up). The statistical software IBM SPSS version 21 was used for data analysis. To evaluate the efficacy of pain intensity, pain interference and pain-related cognitive processes and its comparison with the APC group, the statistical method of mixed linear models was used. At first, the interactive effect of time (3 steps) × group (MBCT and APC group) was obtained to evaluate the effectiveness of MBCT. Then, the post hoc Bonferroni adjustment for multiple comparisons was used.
4. Results
Table 2 provides the sociodemographic and clinical characteristics of the study sample at baseline. The normal distribution of the two groups’ scores on all variables was tested in terms of skewness and kurtosis via the Jarque-Bera test statistic using the EViews program. The hypotheses related to the normal distribution of data in all variables were approved.
| MBCT, No. (%) | APC, No. (%) | |
|---|---|---|
| Sociodemographic Characteristics | ||
| Age, y (mean ± SD) | 36.70 ± 9.69 | 38.2 ± 2.86 |
| Sex | ||
| Male | 14 (32.6) | 15 (35.71) |
| Female | 29 (67.4) | 27 (64.28) |
| Marital status | ||
| Married | 24 (55.8) | 22 (52.4) |
| Unmarried (single, divorced) | 19 (44.2) | 20 (47.6) |
| Educational level | ||
| Academic | 26 (60.5) | 27 (64.3) |
| Non-academic | 17 (39.5) | 15 (35.7) |
| Employment status, % | ||
| Employed | 21 (48.8) | 13 (31.0) |
| Retired | 4 (9.3) | 7 (16.7) |
| Homemaker | 3 (7.0) | 7 (16.7) |
| Unemployed | 12 (27.9) | 12 (28.6) |
| Unemployed due to sickness | 3 (7.0) | 3 (7.1) |
| Clinical Characteristics | ||
| Type of headache diagnosis, % | ||
| Migraine (with or without aura) | 14 (34.9) | 16 (40) |
| Tension-type headache | 16 (34.9) | 18 (41) |
| Cluster headache | 8 (18.6) | 5 (11.8) |
| Episodic paroxysmal hemicranias | 1 (2.3) | 1 (2.4) |
| Short-lasting unilateral neuralgia form headache attacks | 4 (9.3) | 2 (4.8) |
| Time since the first onset of headache, y (mean ± SD) | 17.28 ± 4.04 | 17.38 ± 4.37 |
| Co-morbidity, % | ||
| Fibromyalgia | 10 (23.3) | 13 (31.0) |
| Low back pain | 22 (51.2) | 24 (57.1) |
| Neck pain | 20 (46.5) | 14 (33.3) |
| Inflammatory joint diseases (arthritis, lupus erythematosus) | 9 (20.9) | 9 (21.4) |
| Gastrointestinal disorders (inflammatory bowel disease, IBS, etc.) | 10 (23.3) | 15 (35.7) |
| Other | 6 (14.0) | 6 (14.3) |
Sociodemographic, Clinical, Pain-related Characteristics
The independent t-test was used to compare the mean scores of all questionnaire items at baseline in two groups. No significant difference was found between the two experimental and control groups in the baseline mean scores. Since the groups were not significantly different at baseline, the Mixed Linear Models (MLMs) analysis and Bonferroni post hoc comparison test were run to determine the effect of treatment.
In the MLMs, “Group” was an inter-subject independent variable with two levels of MBCT and APC and “Time” was an intra-subject independent variable with three levels of baseline, posttest, and follow-up. Also, in the MLMs, as noted in Table 2, the reference category group was the APC group and for the time variable, the reference was time 3 or changes at 3 months after the 8-week intervention (follow up). Therefore, in this table, time 1 showed changes from baseline to follow-up and time 2 showed changes from posttest to follow-up.
There was a significant interaction between time 1 and group 1 with a P value of < 0.0001 in pain intensity, pain interference, pain reappraisal, pain focus, and pain openness, indicating that the difference in the slope between the APC group and the MBCT group was significantly different from baseline to three months after the eight-week intervention (follow-up) (Table 3).
| Dependent Variable | Parameter | Estimate | Std. Error | df | t | P Value |
|---|---|---|---|---|---|---|
| BPI (pain severity) | ||||||
| [Time = 1] * [Group = 1] | 0.894 | 0.13 | 62.66 | 6.39 | < 0.001 | |
| [Time = 2] * [Group = 1] | 0.207 | 0.11 | 56.62 | 1.85 | 0.068 | |
| [Time = 3] * [Group = 1] | 0a | 0 | ||||
| BPI (pain interference) | ||||||
| [Time = 1] * [Group = 1] | 3.08 | 0.26 | 59.79 | 11.47 | < 0.001 | |
| [Time = 2] * [Group = 1] | 1.22 | 0.18 | 48.30 | 6.77 | < 0.001 | |
| [Time = 3] * [Group = 1] | 0a | 0 | ||||
| PCPQ (pain diversion) | ||||||
| [Time = 1] * [Group = 1] | 1.53 | 0.41 | 59.19 | 3.65 | 0.089 | |
| [Time = 2] * [Group = 1] | 1.41 | 0.41 | 57.03 | 3.44 | 0.075 | |
| [Time = 3] * [Group = 1] | 0a | 0 | ||||
| PCPQ (pain distancing) | ||||||
| [Time = 1] * [Group = 1] | -5.72 | 0.81 | 67.37 | -6.99 | < 0.001 | |
| [Time = 2] * [Group = 1] | -0.27 | 0.31 | 57.56 | -0.85 | 0.394 | |
| [Time = 3] * [Group = 1] | 0a | 0 | ||||
| PCPQ (pain focus) | ||||||
| [Time = 1] * [Group = 1] | 9.88 | 1.53 | 75.94 | 6.45 | < 0.001 | |
| [Time = 2] * [Group = 1] | 4.19 | 0.77 | 60.22 | 5.40 | < 0.001 | |
| [Time = 3] * [Group = 1] | 0a | 0 | ||||
| PCPQ (pain openness) | ||||||
| [Time = 1] * [Group = 1] | -8.77 | 0.71 | 70.06 | -12.33 | < 0.001 | |
| [Time = 2] * [Group = 1] | -2.57 | 0.39 | 56.88 | -6.54 | < 0.001 | |
| [Time = 3] * [Group = 1] | 0a | 0 |
Estimates of Fixed Effects (Dependent Variables)
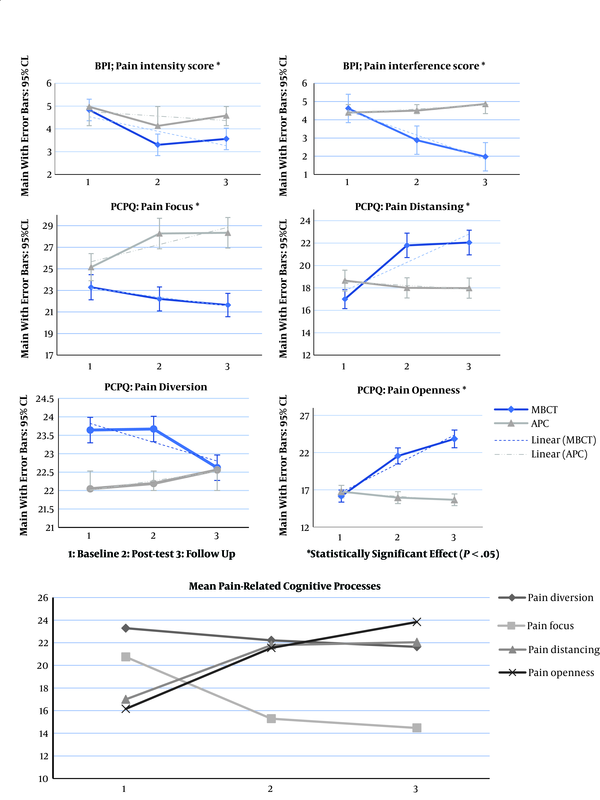
There was no significant interaction between time 3 and group 1 with a P value of 0.068, 0.075, 0.394, respectively, in pain intensity, pain diversion, and pain reappraisal, indicating that the rate of change over time from two weeks after (posttest) and three months after (follow-up) the eight-week intervention was similar between the two groups. This is shown better in Figure 2, where the lines from posttest to follow-up are approximately parallel (Figure 2).
There was also a significant interaction between time 2 and group 1 with a P value of < 0.0001 in pain interference, pain focus, and pain openness, indicating that the difference in the slope between the APC group and the MBCT group was significantly different over time from two weeks after (posttest) and three months after (follow-up) the intervention. The significant interaction between time and group is shown in Figure 2, indicating that the two groups had very different changes over time.
5. Discussion
The aim of the present study was to examine the effect of MBCT on pain perception and pain-related cognitive processing. The first research question investigated the pure effect of MBCT on chronic pain by means of a placebo control group. The mixed liner analysis of predictor variables included in the model showed that there was a significant interaction between time and group. These results revealed a significant difference in the change of scores across the two groups over time (for pain severity: F (2, 62.66) = 26.11; P < 0.001 and for pain interference: F (2, 48.30) = 66.64; P < 0.001).
This will come as a pleasing result for researchers who claim that MBCT can affect pain perception. This finding corroborates the findings of Day et al. who found that the MBCT affected chronic pain (11, 12). Our study also demonstrated that distinctly and without the therapist's attention effect, MBCT can work in patients with primary headache.
Concerning the second research question that dealt with the efficacy of MBCT in pain-related cognitive processing, the results of data analysis indicated that MBCT resulted in a higher rate of pain openness (P < 0.001) and a lower rate of pain focus (P < 0.001) compared to the APC group from baseline to follow-up. The results also showed that MBCT resulted in a higher rate of pain distancing compared to the APC group from baseline to posttest and the reappraisal scores decreased in the follow-up. Regarding pain diversion, data analysis indicated that MBCT was likely ineffective and could not make any changes.
Concerning pain diversion, patients in the APC group also showed slightly increased scores from baseline to follow-up, which can be attributed to the attention-placebo effect. It seems that due to the relationship between practitioners in group therapy sessions, behavioral avoidance converted to cognitive avoidance in the APC group. This cognitive processing includes attempts to divert attention from the pain. This finding contradicts the Windich-Biermeier et al. study that reported the effects of distraction on pain in children and adolescents with cancer (24). Wiederhold et al.’s study in 2014 also was in contrast with the results related to pain diversion processing in the present study (25). One explanation for this different finding is that diverting attention needs to ignore a significant part of the information and requires information selection with inverse emotional and cognitive direction. Theoretically, MBCT extends the awareness moment to moment (26). Therefore, MBCT did not lead to pain diversion. Pain is part of awareness. Therefore, attentional processes during MBCT did not distract the pain.
Pain focus involves two distinct processes (absorption or voluntary attentional focus process and rumination or involuntary attention focus to pain) (23). Pain is one of the biggest anxious subjects and attention models describe that anxious individuals (as stress responses) have involuntary attention biases toward stress-related information (27, 28). Also, based on the theory of mindfulness, interventions lead to decrease in stress responses (29). Therefore, MBCT could regulate the alerting attention system and orienting system and result in reduced pain focus.
In explaining pain openness processes (including cognitive processes with acceptance and without judgment) and long-standing changes in MBCT, it can be stated that during MBCT sessions, participants learned to accept the pain condition and this gave them the opportunity for responding without judgment instead of surrendering to negative beliefs about pain (13). Other authors obtained similar results in pain openness processing (30, 31).
In explaining pain distancing processes (including cognitive processes with reappraisal and dissociation) and short-term changes in MBCT, it can be stated that using cognitive techniques, participants learned to challenge with negative automatic pain cognitions and thus they changed their attitude toward pain.
An implication of these findings is in cognitive-based interventions (32), especially those that are combined with mindfulness skills such as MBCT that can lead to higher levels of cognitive processing such as pain openness, pain reappraisal, and lower level of pain focus. However, this method does not affect pain diversion processing. Taken together, the findings showed that over time, the effect of the treatment will decline in pain distancing process, pain severity and therapeutic changes such as pain openness, pain focus, and pain interference will be maintained over time. These findings support researchers’ recommendations for empirical examination of cognitive mediators of MBCT to promote and complete the comprehensive theoretical model (13).
The findings in this study are subject to at least three limitations. First, longer follow-ups could have been more revealing the durability and effectiveness of MBCT in pain-related cognitive processing. The second limitation was that the current researcher administered all the treatment sessions in the study by herself. This can be considered as an advantage and disadvantage at the same time. The advantage lies in the fact that therapy variability as an extraneous variable was controlled. Despite that, the researcher tried her best not to influence patients’ performance but this research may have suffered from “researcher expectancy”, because the researcher might have influenced the patients based on the predictions that she had flowing the review of related literature. Considering the fact that there was no integral protocol for the APC group, the third limitation of this study is the lack of coherent logic during the APC sessions.
Finally, these findings stated nothing about the effect of MBCT on daily headache medications. Therefore, the evidence that MBCT may have affected medication use justifies the pursuit of additional research to identify whether MBCT can be effective in reducing prescribed headache medications. There is a need for further research to ascertain what mediators are involved in the efficacy of MBCT.
5.1. Conclusions
In this paper, four types of pain-related cognitive processing were subjected to investigation, including pain diversion, pain focus, pain distancing, and pain openness. The results indicated a statistically significant difference between the two groups in pain openness and pain focus from baseline to follow-up. Our findings also suggested that the therapeutic effects were not maintained in pain distancing until the follow-up. However, the results revealed that MBCT did not affect pain diversion processing, suggesting that MBCT did not divert and distract attention.