1. Background
Postoperative nausea and vomiting (PONV) is a common anesthesia-related complication that can occur in many surgical procedures such as eye surgery (1-5). PONV is an unpleasant GI complication that exerts pressure on stitches and opens or leaks the surgical wound, thereby leading to bleeding (6-9). More than one-third of delays in postoperative patient discharge is caused by PONV (10-14).
Nowadays, various strategies including complementary medicine are used to control the condition (15-19). Herbal medicine has been used for thousands of years as a complementary treatment in different countries worldwide (20-22). According to the WHO, more than 80% of the world population is currently using herbal extracts, with more prevalence in undeveloped than in developed countries (23). Garlic, mint, and ginger are commonly used to treat nausea and vomiting (24). Moreover, Zingiber officinale rhizome (ginger) as the ginger root is an herbal plant containing many active biological compounds such as Gingerols and Shogaols. These compounds can have anti-nausea, sedative, anti-inflammatory, anticancer, and prostaglandin reducing effects (24).
Since a number of studies have shown that PONV commonly occurs after eye surgery (25, 26) and contradictory results exist about the ginger effects on PONV (6, 8, 18), as well as considering the sedative effects of ginger and its potential impact on vital symptoms such as hypotension, this study aimed to explore the effect of ginger on PONV and vital signs in patients undergoing eye surgery.
2. Methods
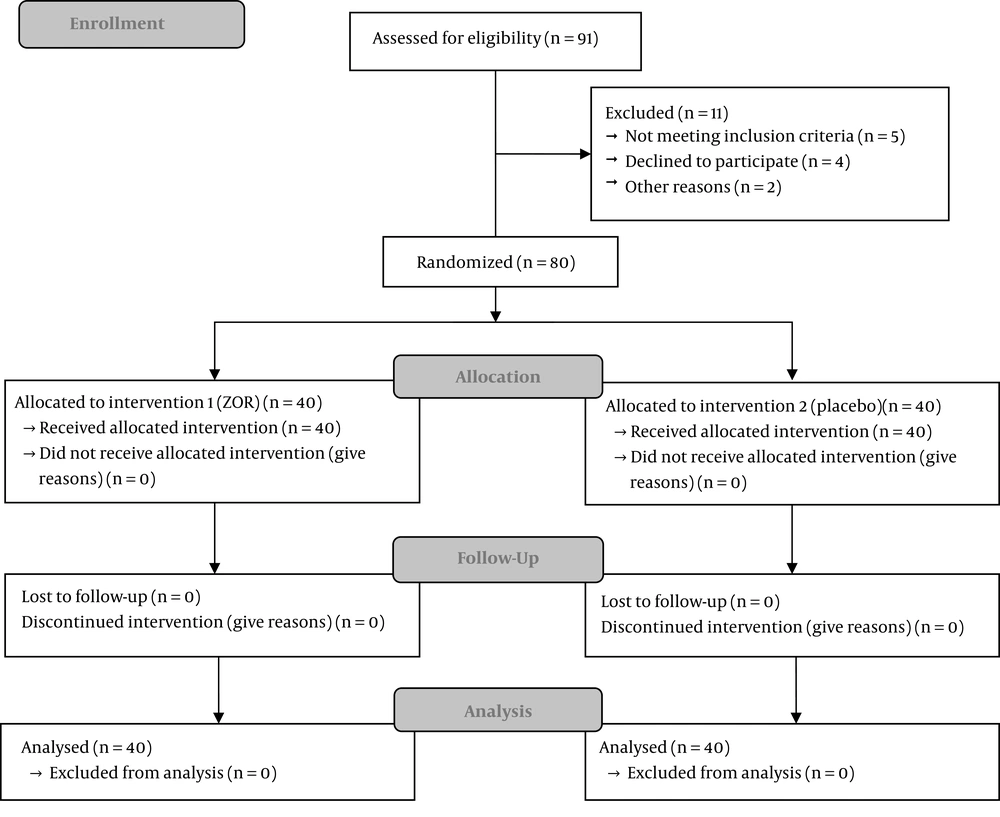
This was a triple-blind clinical trial. The inclusion criteria included the lack of cancer, an age of 18 - 60 years, lack of pregnancy, ability to take the capsules, platelets count of > 100000, free from conditions such as GI obstruction, seizure, hepatitis, diabetes, kidney disorders, allergy to the ginger root, voiding drugs for corticosteroid, nausea and vomiting, and no history of smoking. A total of 80 patients were randomly selected to undergo eye surgery, meeting the criteria and being willing to participate in the study. The study design was based on the consort 2010 flow diagram (Figure 1). Samples and medical consent were taken based on ethical code 101568 from the Iran University of Medical Sciences (IUMS) and IRCT code 2014060918020N1 from www.irct.ir.
Ginger capsules (1000 mg) were prepared at a pharmacology lab and placeboes were made with identical shapes such that they could not be differentiated easily. Both ginger and placebo capsules were administered randomly. Patients were divided into two groups of A and B. Group A received a single ginger dose of 1000 mg and group B received a placebo with 30 mL water before surgery. Based on anesthesia expertise, conditions such as medication type, administration, and duration of anesthesia were the same among all participants. The medication of anesthesia induction included midazolam 2 mg, fentanyl 2 µg/kg, thiopental 5 mg/kg, and atracurium 0.5 mg/kg. Moreover, 50% oxygen, 50% N2O were used for the maintenance of anesthesia. We did not use medications that could cause nausea and vomiting such as morphine. Also, all patients received 500 mL of normal saline. Injectable ondansetron was used if patients needed anti-nausea medication.
To evaluate nausea, we used a 10 cm linear analog scale that ranged from 0 to 10; scores 0, 1 - 3, 4 - 6, 7 - 9, and 10 were assigned to no, mild, moderate, severe, and very severe nausea, respectively. Vomiting was defined as a severe gastrointestinal stimulation, which caused the forceful discharge of the contents of the digestive tract from the mouth (20). The number of vomiting episodes was recorded (21). Using a premade checklist, the severity and frequency of PONV were measured by an investigator, unaware of the treatment regimen, immediately, 15 min, 30 minutes, and 2 hours after recovery. Additionally, the vital signs included the heart rate, systolic and diastolic pressure, respiratory rate assessed 30 minutes before anesthesia induction and 30 minutes after recovery. All collected data were analyzed by SPSS V. 21, using a t-test and chi-square test.
3. Results
Overall, 80 subjects participated in the study. The study results indicated that 40% of the participants in group A were female and 60% were male, and in group B, 51.5% of the participants were female and 48.5% were male. The mean age was 36.24 ± 2.17 in group A and 36.24 ± 2.49 in group B. The mean weight was 70.68 ± 2.09 in group A and 70.06 ± 2.22 in group B. No significant difference was found concerning age, gender, and weight between the two groups (P > 0.001).
As shown in Table 1, four patients (10%) in group A reported nausea compared to 10 patients (40%) in group B (P < 0.005). The visual analog scores of nausea immediately, 15 minutes, 30 minutes, and 2 hours after recovery were lower in group A than in group B. The differences were statistically significant at immediate (P = 0.03) and 2 hours after recovery (P = 0.02) between the two groups. The number of patients with vomiting was significantly lower in group A (n = 0, 0%) than in group B (n = 10, 40%) (P < 0.001) (Table 2).
| Nausea | After Recovery | After 15 Minutes | After 30 Minutes | After 2 Hours |
|---|---|---|---|---|
| Ginger group (n = 40) | 1.05 ± 2.04, 2 (5) | 1.28 ± 2.47, 1 (2.5) | 0.50 ± 1.40, 0 (0) | 1.37 ± 2.24, 1 (2.5) |
| Placebo group (n = 40) | 2.03 ± 2.89, 4 (10) | 2.07 ± 2.78, 4 (10) | 0.53 ± 1.33, 2 (5) | 2.43 ± 2.72, 0 (0) |
| P value | 0.03 | 0.1 | 0.8 | 0.02 |
aValues are expressed as mean ± SD, No. (%).
| Vomiting | After Recovery | After 15 Minutes | After 30 Minutes | After 2 Hours | Total |
|---|---|---|---|---|---|
| Ginger group (n = 40) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) |
| Placebo group (n = 40) | 4 (10) | 2 (5) | 2 (5) | 0 (0) | 10 (40) |
| P value | < 0.001 | > 0.05 | < 0.001 | 1 | < 0.001 |
aValues are expressed as No. (%).
As shown in Table 3, the comparison of vital signs (heart rate, systolic and diastolic pressure, and respiratory rate) revealed no significant difference between the two groups (P > 0.5).
| Variable | Ginger Group (N = 40) | Placebo Group (N = 40) | P Value |
|---|---|---|---|
| Systolic blood pressure (mmHg) | |||
| Before | 128.84 ± 11.94 | 127.36 ± 13.15 | 0.61 |
| After | 124.21 ± 13.25 | 127.71 ± 12.50 | 0.24 |
| Diastolic blood pressure (mmHg) | |||
| Before | 76.71 ± 7.20 | 76.39 ± 8.30 | 0.86 |
| After | 74.81 ± 8.27 | 77.95 ± 7.62 | 0.09 |
| Heart rate | |||
| Before | 80.74 ± 11.69 | 80.24 ± 9.31 | 0.84 |
| After | 78.08 ± 9.47 | 80.79 ± 9.34 | 0.21 |
| Respiratory rate | |||
| Before | 20.24 ± 2.29 | 18.74 ± 1.85 | 0.25 |
| After | 19.61 ± 2.47 | 19.67 ± 2.47 | 0.06 |
aValues are expressed as mean ± SD.
4. Discussion
PONV has always been regarded as the most unpleasant sequel of anesthesia, especially after eye surgery. This study was conducted to evaluate the effect of ginger on PONV and vital signs after eye surgery.
The present study results indicated that ginger could significantly reduce the incidence of nausea (P < 0.005). Also, ginger significantly reduced the severity of nausea immediately and 2 hours after recovery in patients undergoing eye surgery (P < 0.005). Seidi et al. in 2017 (18) and Albooghobeish et al. (20) in 2018 demonstrated that the incidence and severity of PONV were significantly lower in the ginger group than in the placebo group. These studies are similar to our study. Also, Nanthakomon and Pongrojpaw similar to our study showed that the most statistically significant differences occurred at 2 hours after recovery (21).
According to the results of the study, the frequency of vomiting after eye surgery was significantly lower in the ginger group than in the placebo group (P < 0.001). A study by Bameski et al. indicated that the ginger extract may play a role in reducing the frequency of vomiting (27) and another study by Hajbaghery et al. showed that ginger could reduce the frequency of vomiting in post-nephrectomy surgery, which coincide with the current study (28). Vousooghian et al. demonstrated that ginger could decrease vomiting but was ineffective in the onset of PONV (29). However, another study by Morin indicated that the ginger extract did not affect PONV in the first 24 hours post-surgery (30). It is very important to know that the ginger dose in Vosoghian et al. study was 500 mg (29) and in Bameshki et al study, the frequency of vomiting was almost equal in both ginger and placebo groups with no significant difference (27). The ginger dose in the present study was 1000 mg while a meta-analysis study performed by Chaiyaknaprak et al. in 2006 demonstrated that a minimum dose of 1 g prevented the PONV (23).
Nonetheless, based on the guideline provided for PONV management after surgery in 2013 and the previous meta-analysis, the ginger treatment did not show to be effective in preventing PONV but a recent meta-analysis proved that the administration of a minimum dose of 1 g an hour prior to anesthesia was more effective than placebo (15-18). Therefore, our study used capsules containing 1 g ginger and showed the effectiveness of ginger in reducing PONV.
According to the literature, there has been no study of changes in the vital signs of patients before and after ginger administration. This may be a strong point for the present study. The results showed that ginger had no adverse effects on the vital signs of patients undergoing eye surgery.
4.1. Conclusions
Based on the results obtained in this study, it is concluded that ginger can be used as a prophylactic herbal medicine to prevent PONV after eye surgery. Also, considering the absence of adverse changes in vital signs, its low cost, and easy access, ginger can be suggested as a proper PONV prevention candidate for patients with eye surgery by considering other health conditions.