1. Background
Laparoscopic surgery is getting more popular due to fast recovery. In addition, laparoscopic surgery needs smaller incision, has less postoperative pain, and lower rate of mortality in comparison with laparotomy (1, 2). The reports show that incidence of shoulder pain after laparoscopic gynecologic surgery is 80% (1). Shoulder pain can also be intense at 24 hours after laparoscopic hysterectomy (3).
Carbon dioxide (CO2) can be trapped in the space between liver and diaphragm after laparoscopic surgery. The trapped CO2 irritates phrenic nerve and causes pain in shoulder and upper abdomen (1). There are many ways to reduce postlaparoscopic shoulder pain including blowing low pressure gas, washing the diaphragm with local anesthetic, local anesthesia of peritoneal surface, and prescription of nonsteroidal anti-inflammatory drugs. However, these pain-reducing techniques have partial effects and there is no reliable method. Most of the available techniques are complicated and have limited clinical implications (4-6).
Recently, some techniques are introduced that can potentially alleviate various types of pain in patients after laparoscopic surgery. Intraperitoneal infusion of normal saline (NS), which washes out CO2 with physiologic buffer system, has long-time effect and may reduce pain in shoulder and upper abdomen after laparoscopic surgery (7, 8). The robust evidence indicates the potential beneficial effect of pulmonary recruitment maneuver (PRM) on reducing postoperative upper abdominal pain (9). The PRM may reduce pain by mechanically increasing intraperitoneal pressure to accelerate removing residual CO2 after operation (8, 10). However, the information about the potential beneficial effects of intraperitoneal infusion of NS and PRM is limited (1).
2. Objectives
The present randomized, controlled trial aimed at evaluating the effect of intraperitoneal infusion of NS and PRM on reducing pain in shoulder, upper abdomen, and incision site after laparoscopic gynecologic surgery.
3. Methods
3.1. Study Design
The current randomized, controlled, triple-blind trial was conducted on female patients undergoing gynecologic surgery from October 2013 to August 2015 in a referral hospital in Tehran, Iran. The study protocol was approved by the Ethics Committee of Tehran University of Medical Sciences (TUMS) and the study was also registered in the Iranian Registry of Clinical Trials (IRCT) prior to sample recruitment (IRCT201402022576N8).
3.2. Study Population
Patients aged 20 - 65 years with benign gynecologic diseases and ASA (American Society of Anesthesiologists) class I/II that underwent laparoscopic gynecologic procedures were included. Patients that underwent surgery for malignant indications were excluded. The subjects all signed an informed consent form before entering the study.
3.3. Interventions
Patients were randomly allocated to one of the four groups using a computer randomization program. The patients in the intervention groups received either (A) intraperitoneal infusion of NS, (B) PRM, or (C) simultaneously two former interventions. For group A, NS 1.5 - 2 mL/kg of body weight at 37°C was infused into left, middle, and right upper quadrants of abdomen at the end of the surgery. In group B, patients were placed in the Trendelenburg position and the anesthesiologist performed five manual pulmonary inflations at a maximum pressure of 60 cm H2O. PRM was performed mechanically using positive-pressure ventilation to inflate the lungs and lower diaphragm. Subjects in the control group (D) received the routine method by applying gentle abdominal pressure and residual CO2 was removed by passive deflation at the end of surgery.
3.4. Outcome Measures
Primary outcomes of the current study were pain in shoulder, incision site, upper abdomen, and adverse events such as nausea, vomiting, and distension. The outcomes were measured immediately after surgery as well as 2, 6, 12, and 24 hours after surgery. Visual analog scale (VAS) was used to evaluate pain intensity.
3.5. Statistical Analysis
Mean and standard deviation (SD) were calculated for the studied variables. The mean age and operation duration were compared among the intervention groups using the one-way analysis of variance (ANOVA). Multivariate repeated measures ANOVA adjusted for age was used to examine the effects of interventions and time on the outcome measures (i e, shoulder pain, upper abdominal pain, and incision site pain). Data were analyzed using SPSS version 19.0 (SPSS Inc., Chicago, IL, USA). The level of significance was P ≤ 0.05.
4. Results
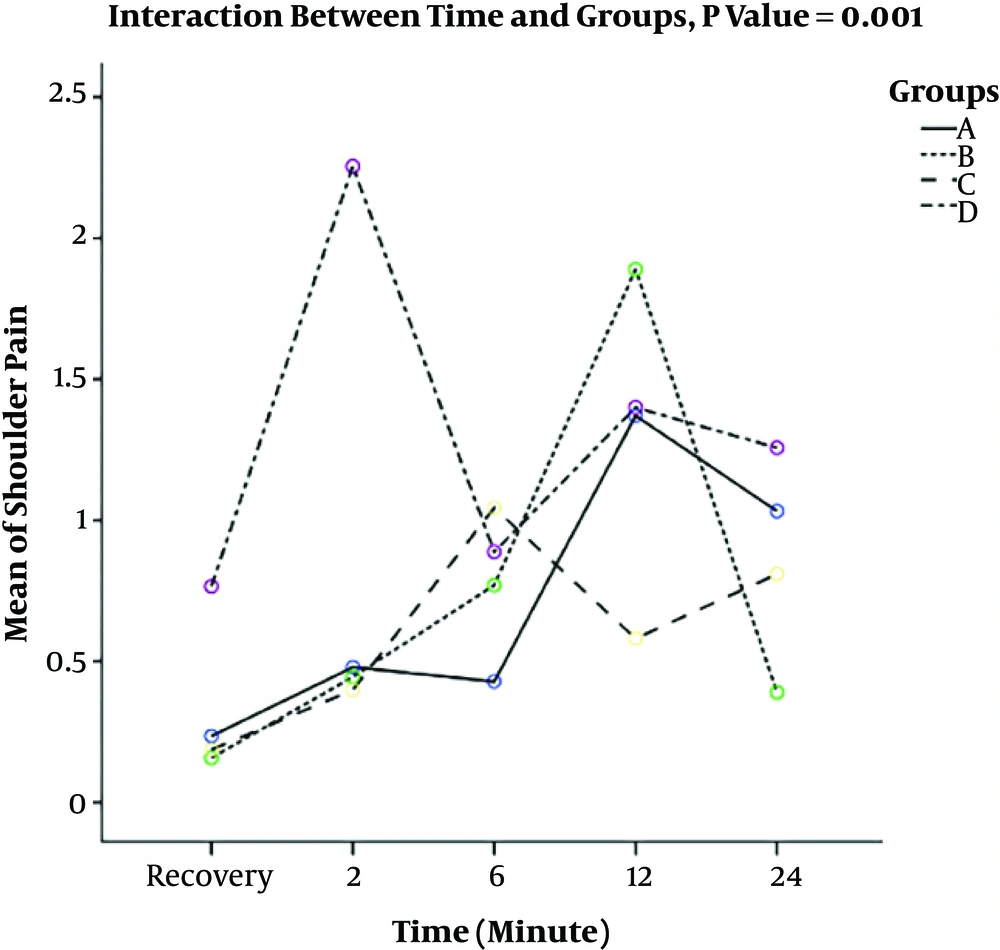
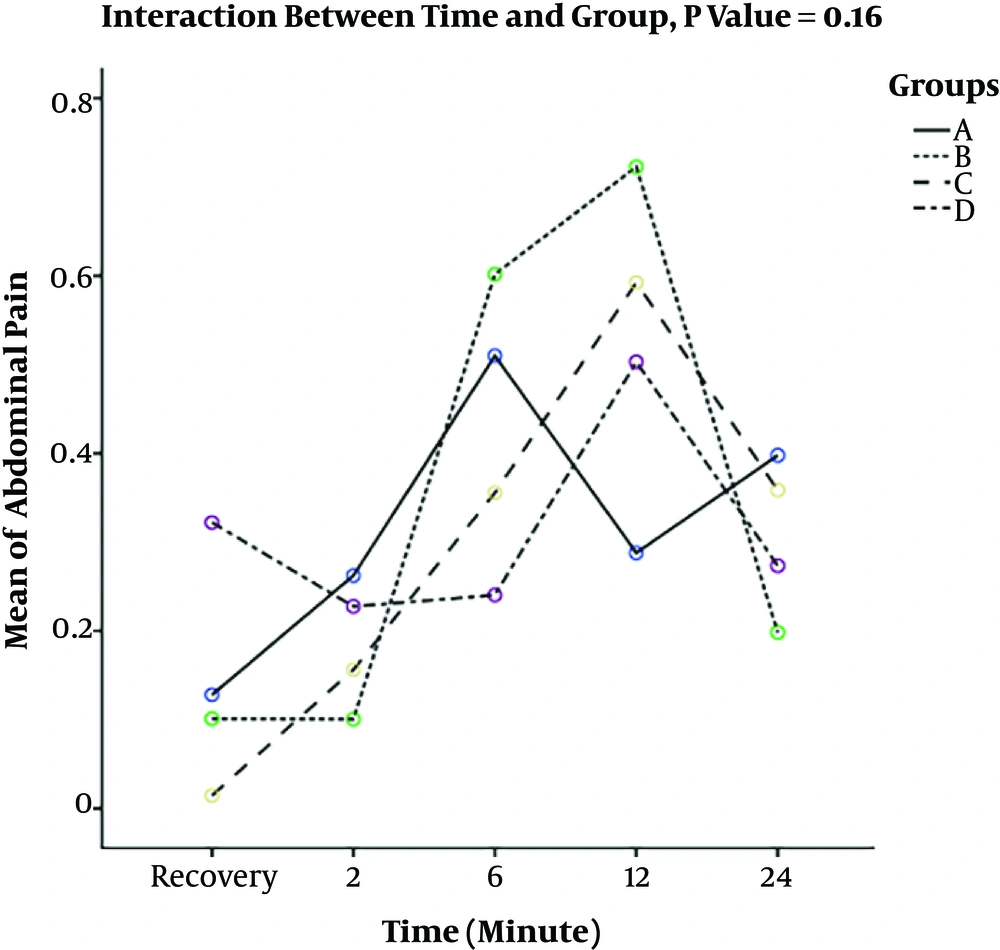
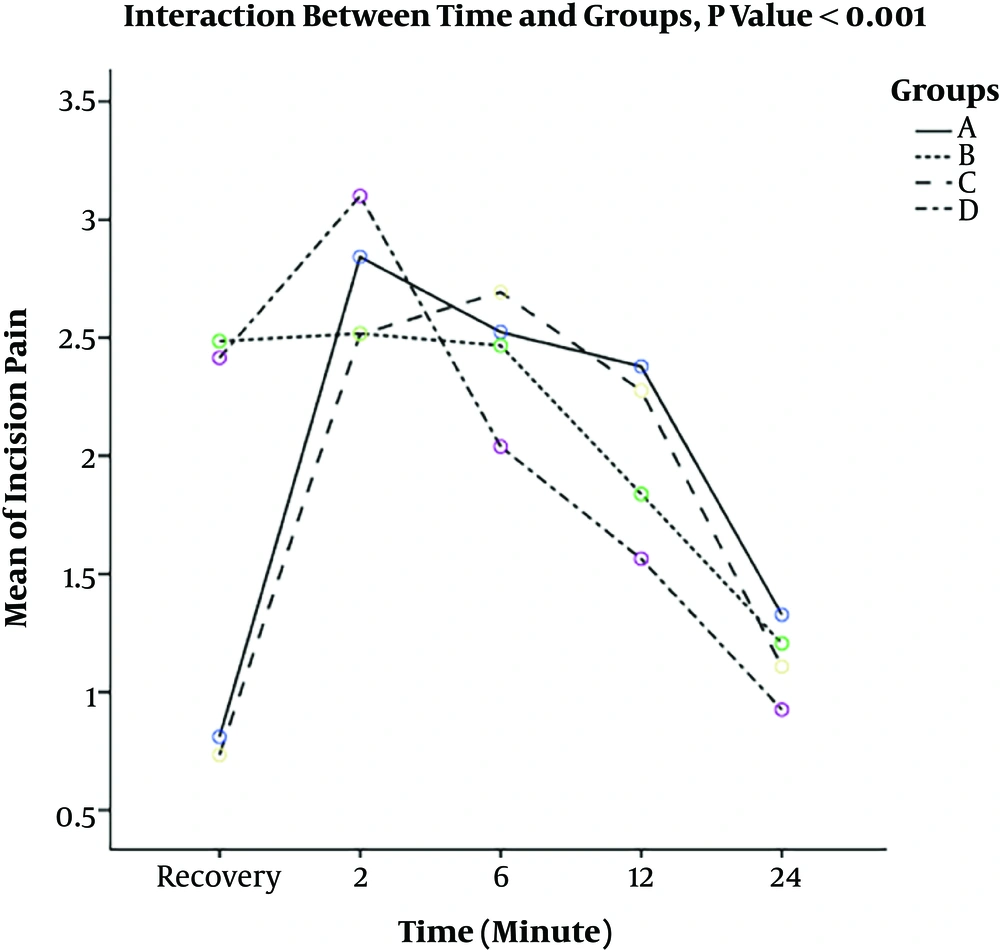
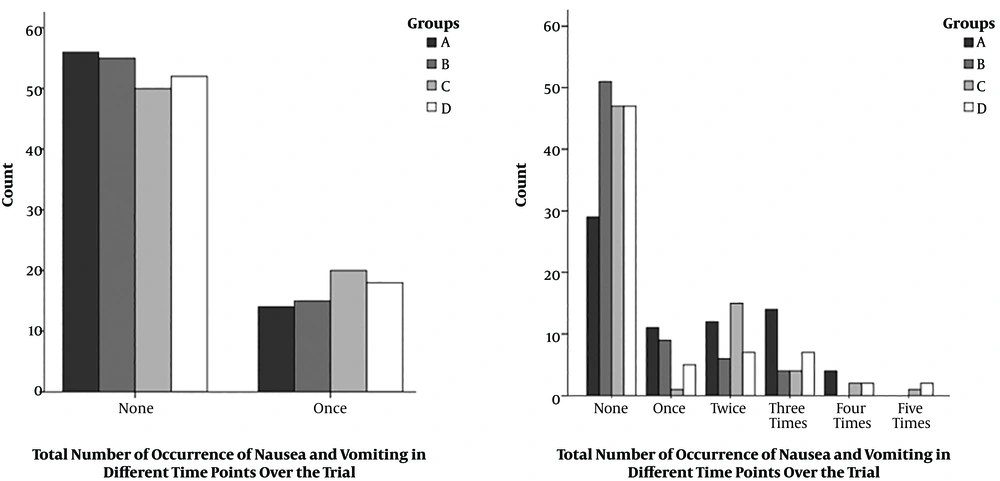
A total of 280 patients with the mean age of 30.5 ± 7.7 years met the inclusion criteria. No statistically significant difference was observed in the mean duration of operation among the intervention groups (P ≤ 0.05) (Table 1). Multivariate repeated measures ANOVA showed unsteady pattern for pain in shoulder, upper abdomen, and incision site at different time points over the trial (Figures 1 - 3). Interaction of time interval and intervention status was statistically significant for shoulder and incision site pain (P ≤ 0.05). The study results showed potential beneficial effect of PRM on the reduction of postoperative shoulder pain; therefore, compared to other groups, patients receiving PRM had the medium level of shoulder pain 24 hours after surgery (mean = 0.4). The patients in the control group had the lowest incision site pain 24 hours after surgery (mean = 0.91) and the group received both interventions had lower incision site pain 24 hours after surgery (mean = 1.10) (Table 2). The occurrence of complications episodes across intervention groups during the first 24 hours after surgery was different; therefore, in the patients that simultaneously received both interventions, the total number of nausea and vomiting episodes was higher than the other groups; while the total number of occurrence of distension episodes in patients receiving intraperitoneal infusion of NS and routine methods were higher than those of the other groups (Figure 4).
| Group | A (N = 70) | B (N = 70) | C (N = 70) | D (N = 70) | P Value |
|---|---|---|---|---|---|
| Duration of operation | 82.1 ± 8.1 | 78.8 ± 7.1 | 82.0 ± 9.7 | 77.7 ± 7.7 | 0.21 |
Abbreviations: A, normal saline intraperitoneal infusion; B, pulmonary recruitment maneuver; C, simultaneously received two interventions; D, control group.
aValues are expressed as mean ± SD.
| Variable | Follow-Up, min | P Valueb | ||||
|---|---|---|---|---|---|---|
| Recovery | 2 | 6 | 12 | 24 | ||
| Shoulder pain | 0.01 | |||||
| A | 0.22 ± 0.78 | 0.48 ± 1.22 | 0.43 ± 1.50 | 1.38 ± 1.49 | 1.05 ± 1.37 | |
| B | 0.14 ± 0.68 | 0.44 ± 1.27 | 0.77 ± 1.51 | 1.90 ± 2.41 | 0.40 ± 0.80 | |
| C | 0.20 ± 0.82 | 0.40 ± 0.92 | 1.04 ± 2.02 | 0.57 ± 1.17 | 0.80 ± 1.07 | |
| D | 0.79 ± 1.91 | 2.26 ± 2.65 | 0.89 ± 1.48 | 1.39 ± 1.49 | 1.24 ± 1.09 | |
| Upper abdominal pain | 0.16 | |||||
| A | 0.11 ± 0.53 | 0.26 ± 0.71 | 0.51 ± 0.92 | 0.28 ± 0.83 | 0.40 ± 0.82 | |
| B | 0.09 ± 0.44 | 0.10 ± 0.54 | 0.60 ± 1.22 | 0.71 ± 1.07 | 0.20 ± 0.73 | |
| C | 0.03 ± 0.23 | 0.16 ± 0.67 | 0.36 ± 0.94 | 0.60 ± 1.01 | 0.36 ± 0.72 | |
| D | 0.34 ± 1.35 | 0.23 ± 0.92 | 0.24 ± 0.69 | 0.51 ± 0.91 | 0.27 ± 0.70 | |
| Incision site pain | < 0.001 | |||||
| A | 0.75 ± 1.57 | 2.80 ± 2.65 | 2.49 ± 2.18 | 2.38 ± 2.00 | 1.34 ± 1.22 | |
| B | 2.44 ± 2.46 | 2.49 ± 2.17 | 2.44 ± 1.97 | 1.84 ± 1.92 | 1.21 ± 1.33 | |
| C | 0.77 ± 1.71 | 2.54 ± 2.63 | 2.71 ± 1.75 | 2.27 ± 1.51 | 1.10 ± 1.09 | |
| D | 2.47 ± 2.85 | 3.14 ± 2.75 | 2.07 ± 1.70 | 1.56 ± 1.46 | 0.91 ± 1.11 | |
Abbreviations: A, normal saline intraperitoneal infusion; B, pulmonary recruitment maneuver; C, simultaneously received two interventions; D, control group.
aValues are expressed as mean ± SD.
bP value for interaction of time interval and intervention status.
5. Discussion
The results of the present randomized, controlled triple-blind trial showed that compared to the other interventions, PRM significantly decreased postoperative shoulder pain after 24 hours; while among the patients that received the routine method of gentle abdominal pressure, the incision site pain significantly decreased after 24 hours.
The potential beneficial effect of intraperitoneal infusion of NS is suggested to reduce pain after cholecystectomy (11, 12) and laparoscopic surgery for benign gynecologic lesions (8); but the current study, consistent with other studies (8-10), showed that PRM was superior to intraperitoneal infusion of NS in reducing postoperative pains. There was rare evidence about the effect of intraperitoneal infusion of NS and PRM on pain in incision site, but the current study findings showed that incision site pain was lower in patients receiving routine method of gentle abdominal pressure at 24 hours than the other groups.
The results of a study by Tsai et al., (8) comparing the effect of intraperitoneal infusion of NS with PRM in postoperative pain showed that compared to the control group, postoperative shoulder and upper abdominal pain decreased in patients receiving intraperitoneal infusion of NS or PRM. Although the evidence was consistent with the current study results, unlike the current study, they showed that intraperitoneal infusion of NS was more effective than PRM in reducing shoulder and upper abdominal pain after laparoscopic surgery for benign gynecologic lesions. The disagreement was probably due to difference in time of follow up; in the study by Tsai et al., the effect of intraperitoneal infusion of predominant NS was measured after 48 hours. Although intraperitoneal infusion of NS can be considered as a feasible technique, it is observed that due to abdominal fullness, the patients’ quality of life during the immediate postoperative period is decreased (9).
Treatment effect of applying intraperitoneal infusion of NS and PRM was assessed in a study (13); the study provided the evidence on potential beneficial effect of combined intervention of intraperitoneal infusion of NS and PRM to reduce postlaparoscopic shoulder and upper abdominal pain. In the current study, although employing the two interventions simultaneously could decrease shoulder pain compared to the control group, pain in upper abdomen was lower in the control group. It is argued that privileges of using the two interventions simultaneously are working with different mechanisms at different phases (13). It is documented that the effect of PRM diminished by 48 hours and PRM has short-time effects. On the contrary, intraperitoneal infusion of NS has long-time effects and its effect persists after 48 hours (8).
It is crucial to emphasize that the beneficiary effect of pain reducing techniques in elective laparoscopic gynecologic surgery in patients with ASA class ≥ III is still questionable. Future studies should also be conducted on the effect of these techniques in different patients. Recently, studies evaluating new methods and techniques to reduce postlaparoscopic shoulder pain are increasing; such as the new drug regimens including oral pregabalin (14), oral gabapentin (15), acetazolamide (16), and intraperitoneal sub-diaphragmatic instillation of bupivacaine plus morphine (17).
The current study had some strengths and limitations. The main strength of the present study was its efficient design; on the other hand, the sample size was statistically large enough to detect small differences between the two groups. The main limitation of the current study was short follow-up time; therefore, the effect of intraperitoneal infusion of NS appeared in 48 hours. In conclusion, the current study showed that PRM technique can be considered as a safe and easy technique to reduce pain in shoulder and upper abdomen after 24 hours in patients undergoing elective laparoscopic gynecologic surgery; in addition, patients receiving gentle abdominal pressure had lower incision site pain at 24 hours than other intervention groups.