1. Background
Cannulation of a central vein is a common procedure in cardiac surgery for monitoring central venous pressure, cardiopulmonary resuscitation, insertion of a transvenous pacemaker, difficult peripheral catheterization, and rapid fluid resuscitation (1, 2). Nowadays, percutaneous infraclavicular subclavian vein (SV) cannulation is a well-known invasive procedure performed by anesthesiologists in cardiac surgery. SV catheterization is associated with a lower risk of infection and more patient comfort than internal jugular vein (IJV) cannulation (3, 4). There are three techniques for infraclavicular SV cannulation based on the needle insertion point (relative to the midpoint of the clavicle). Two of these approaches are generally preferred for catheterization, including midpoint (MP) approach and lateral (LA) approach. The MP approach is the most common approach for infraclavicular SV cannulation while the LA approach is associated with more safety than other techniques (5, 6). The third approach named the media approach is less used because of the difficulty in sustaining the needle in a horizontal situation and the requirement of passage through the costoclavicular ligament. A literature review showed no study of the comparison between the MP and LA approaches.
2. Objectives
This study aimed to investigate the complications and success rate of MP approach versus LA approach for SV catheterization.
3. Methods
This randomized clinical trial was performed between April 2018 and February 2019. The protocol of the study was approved by the Ethics Committee and registered in the Iranian Registry of Clinical Trials numbered IRCT20120721010348N5. Written informed consent was obtained from each patient before study enrolment.
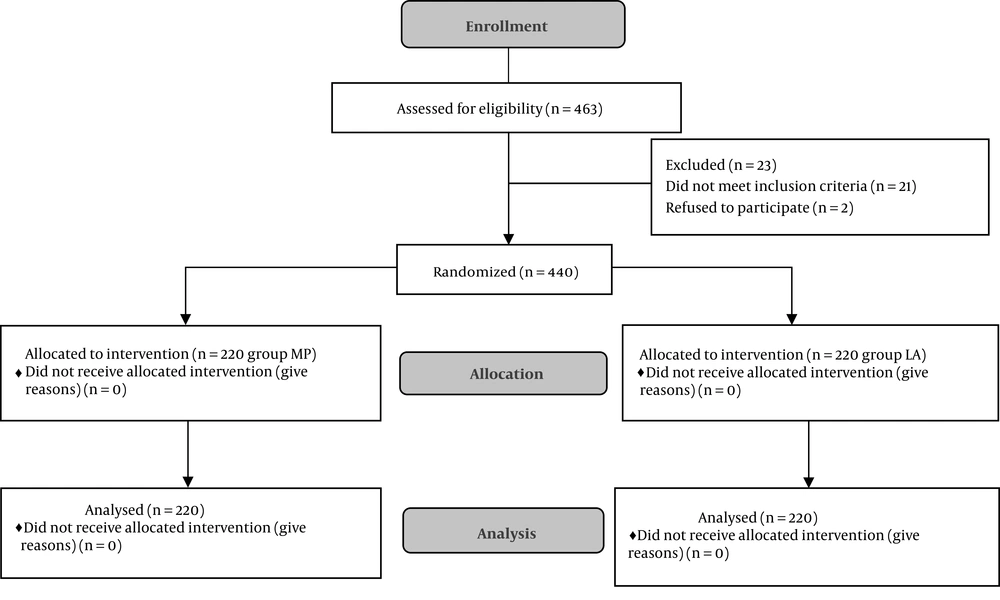
The study recruited 440 patients, aged 25 to 87 years, classified as ASA physical status II or III, undergoing elective CABG surgery. They were randomly assigned to either the MP approach or the LA approach groups for catheterization using block randomization with a block size of 4 (Each block with 110 participants). The flow diagram is shown in Figure 1. The statistical analyst and patients were blinded to the type of techniques; however, the blindness of physician was not possible. The exclusion criteria included emergency surgery, concurrent carotid endarterectomy, blood coagulopathy, history of radiotherapy, skin infection or hematoma in the region of SV cannulation, and history of catheterization or surgery at puncture sites.
3.1. Procedure
After tracheal intubation, the head of the patient was slightly turned to the opposite side and the right arm was kept by the side. During needle insertion, the patient was disconnected from mechanical ventilation. A right-handed physician performed the cannulation of the right subclavian vein in the Trendelenburg position. For the MP approach, the area of the puncture site was 1 to 2 cm beneath the midpoint of the clavicle and we directed the needle toward the suprasternal notch. For the LA technique, the area of the puncture site was 1 to 2 cm lateral to the midclavicular line and directing the needle toward the suprasternal notch (6). The modified Selinger technique was used for both groups after the puncture of the subclavian vein. The depth of the catheter (20 cm, 3 lumens) insertion was 15 cm for both groups. After successful catheterization, all catheter lumens were tested for blood aspiration. If aspiration was not successful, the catheter was withdrawn slowly to the point that blood was aspirated freely and then secured. Each skin puncture was considered as an attempt. If the specified technique of catheterization was not successful after two attempts, the ipsilateral IJV was chosen for cannulation. Immediately after surgery, a chest radiograph was obtained to determine the catheter tip position and the complications of cannulation in the intensive care unit. The arterial puncture and the number of needle passes were recorded during the procedure.
3.2. Data Gathering
The study variables included gender, age, body mass index (BMI), weight, height, the number of cannulation attempts, the success rate of catheterization, and probable complications (catheter tip malposition, hemothorax, pneumothorax, subclavian arterial puncture, thoracic duct damage, and hematoma at the puncture site).
3.3. Statistical Analysis
A total sample size of 440 patients (220 patients in each group) was needed to achieve a power of 95% and detect a significant difference (P < 0.05). The data were analyzed using SPSS software (version 20). The normality of continuous data was checked by the Kolmogorov-Smirnov test. The chi-square test was used to assess the relationship between the success rate and cannulation approach. In addition, a t-test was conducted to evaluate differences in the mean values of continuous variables between the two groups.
4. Results
In total, 440 elective surgeries were conducted in this survey. The demographic characteristics of the participants are described in Table 1. After being selected, the subjects were randomly divided into two equal groups (n = 220 in each group). The right SV catheterization was performed with the MP or LA techniques. The first attempt of SV cannulation was successful in 371 (84.3%) catheterizations, including 192 (87.3%) in the MP group and 179 (81.4%) in the LA group, without a significant difference between the two groups (P = 0.088). The second attempt of SV catheterization was successful in 37 patients, including 21 (75%) patients in the MP technique and 16 (39%) patients in the LA technique, with a significant difference between the techniques (P = 0.003). The overall success rate after two attempts was 96.8% (n = 213) in the MP technique and 88.6% (n = 195) in the LA technique, with a significant difference between the two groups (P = 0.001). The SV catheterization was unsuccessful in 32 (7.3%) patients after two attempts of catheterization in both techniques (Table 2).
| Variable | MP Group (N = 220) | LA Group (N = 220) | Total (N = 440) | P Value |
|---|---|---|---|---|
| Gender ratio (male/female) | 159/61 | 154/66 | 313/127 | 0.599 |
| Age, y | 62.21 ± 10.71 | 61.59 ± 10.49 | 61.90 ± 10.59 | 0.535 |
| Weight, kg | 71.25 ± 12.66 | 71.42 ± 12.60 | 71.33 ± 12.61 | 0.883 |
| Height, cm | 165.12 ± 8.97 | 164.25 ± 8.95 | 164.69 ± 8. 96 | 0.313 |
| BMI, kg/m2 | 26.09 ± 4.06 | 26.47 ± 4.22 | 26.28 ± 4.14 | 0.335 |
Abbreviations: LA, lateral approach; MP, midpoint approach.
aValues are expressed as mean ± SD.
| Attempts | MP Group | LA Group | Total | P Value |
|---|---|---|---|---|
| First attempt | 0.088 | |||
| Success | 192 ( 87.3) | 179 (81.4) | 371 (84.3) | |
| Failure | 28 (12.7) | 41 (18.6) | 69 (15.7) | |
| Second Attempt (n = 74) | 0.003 | |||
| Success | 21 ( 75.0) | 16 (39.0 ) | 37 (53.6) | |
| Failure | 7 (25.0) | 25 (61.0 ) | 32 (46.4) | |
| Total | 0.001 | |||
| Success | 213 ( 96.8) | 195 (88.6 ) | 408 (92.7) | |
| Failure | 7 (3.2) | 25 (11.4) | 32 (7.3) |
aValues are expressed as No. (%).
The catheter tips placed through the right SV were misplaced in 19 of 440 patients (14 in the MP technique and 5 in the LA technique). In the MP technique, 11 catheter tips were located in the ipsilateral IJV, one catheter tip was placed in the contralateral SV, and two catheters formed a loop around itself over the SV. In the LA technique, one catheter tip was placed in the right IJV and four catheter tips were placed in the contralateral SV. There was a significant difference between the two techniques (P = 0.035). The overall rate of catheter tip malposition was 4.3% in both techniques.
Inadvertent subclavian arterial puncture occurred in 26 (5.9%) patients, including 3 (1.4%) in the MP group and 23 (10.5%) in the LA group, with a significant difference between the groups (P = 0.0001). In 15 (3.4%) patients, pneumothorax was confirmed by chest X-ray, including seven in the MP technique and eight in the LA technique, without a significant difference between the two groups. Although hematoma at the puncture site (0.9%) and hemothorax (0.5%) occurred only in the LA technique, there was no significant difference between the two techniques (Table 3). There was no injury of the thoracic duct in SV catheterization.
| Complications | MP Group | LA Group | Total | P Value |
|---|---|---|---|---|
| Malposition | 14 (6.40) | 5 (2.30) | 19 (4.30) | 0.035 |
| Subclavian artery puncture | 3 (1.40) | 23 (10.50 ) | 26 (5.90) | 0.0001 |
| Pneomotorax | 7 (3.20) | 8 (3.60 ) | 15 (3.40) | 0.739 |
| Hematoma at puncture site | 0 (0.00) | 2 (0. 90 ) | 2 (0.50) | 0.499 |
| Hemothorax | 0 (0.00) | 1 (0. 50 ) | 1 (0.20) | 0.317 |
aValues are expressed as No. (%).
5. Discussion
The results of the present randomized clinical trial showed that the overall success rate and incidence of catheter tip malposition were higher in the MP technique than in the LA technique, whereas the incidence of inadvertent subclavian arterial puncture was lower in the MP technique than in the LA technique for infraclavicular SV catheterization in cardiac surgery.
The subclavian vein offers many potential advantages for central venous catheterization including patient comfort, easy insertion, ease of nursing care, greater diameter, less collapsibility with hypovolemia or shock, low complication rates, the higher level of patient acceptance, and easiness in securing catheters (4, 7). In landmark-based techniques, the clavicle is an important bony surface landmark for SV catheterization. The clavicle is an elongated S-shaped bone that has anterior convexity in its medial two-thirds and anterior concavity in the lateral third portion. The anterior convexity of the clavicle at the junction of the medial and middle thirds (clavicle bend or break) is an important palpable surface landmark.
There are three techniques of infraclavicular approach that vary based on the needle insertion point relative to the midpoint of the clavicle. In the midpoint approach as described by Aubaniac, the needle insertion point is approximately in the midclavicular line (1 cm lateral to the bend of the clavicle). It is generally used by most physicians. In the lateral approach, the point of needle insertion is lateral to the midclavicular line, as first described by Tofield in 1969. Some physicians believe that it improves the safety of the procedure by considering the contour of the clavicle (the lateral third is concave anteriorly). The anterior convexity of the medial two-thirds of the clavicle also facilitates needle insertion in this approach (5, 6). Some studies declare that the lateral approach may reduce the incidence of phrenic nerve injury and pinch-off syndrome (crimping of the catheter between two bones i.e., the first rib and the clavicle) (8).
Kim et al. reported a success rate of 95.6% (1 to 6 attempts) for the LA approach of SV catheterization with a landmark-based technique (9). In another study, Oh et al. documented a success rate of 87% (with LA approach) versus 53% (with MP approach) for SV catheterization with an ultrasound-guided technique and a landmark-based technique, respectively (10). Kang et al. also observed a success rate of 97.2% for the LA approach in the neutral shoulder position with a landmark-based technique (11).
In previous studies, the success rates of the MP approach ranged from 53 to 98% in adults and 87 to 98% in infants and children with landmark-based techniques (3, 10, 12, 13). In our study, the overall success rate was significantly higher in the MP approach (96.8%) than in the LA approach (88.6%) after two attempts with a landmark-based technique. This wide difference in the results of both approaches in different studies may be due to the different sample size of the study, the number of attempts for defining the success rate, catheterization techniques (ultrasound-guided technique or landmark-based technique), age of participants, catheter insertion site, and physician skill. However, as mentioned before, there was no comparative study of MP and LA approaches in terms of success rate in the literature.
Catheter tip malposition is the most common mechanical complication during infraclavicular SV catheterization. It was defined as a catheter tip located in the IJV or contralateral SV (9). Since a sharp angulation exists between the right-sided SV and the right IJV, most catheter tips are positioned in the right IJV (2, 14). Catheter tip malposition may cause local venous thrombosis, elevated intracranial pressure, infection, retrograde perfusion of the intracranial vein, and inaccurate central venous pressure reading. Some authors opine that catheter length of < 20 cm and the passage of the guidewire with the J-tip directed caudally may decrease this complication (10, 15).
Previous publications have reported a malposition rate of less than 3% in the LA technique and more than 3% in the MP technique (9, 11, 14-17). In this study, the malposition rate was significantly higher in the MP technique (6.4%) than in the LA technique (2.3%) after two attempts. The rates of malposition in both approaches in our study are in line with the results of the mentioned studies.
Another serious complication of SV cannulation is accidental subclavian artery puncture that is difficult to compress the puncture site for hemostasis. Since the subclavian artery is anatomically parallel to the subclavian vein, it increases the risk of arterial puncture. Moreover, the right subclavian-jugular venous junction overlies the right subclavian artery, causing this vessel to be more susceptible to injury than the left subclavian artery (12, 17). In some studies, the use of real-time ultrasound guidance could reduce the incidence of arterial puncture (7-9). If an arterial puncture is suspected, the needle is immediately withdrawn and a direct pressure is continuously applied to the puncture site for 5 minutes to prevent hematoma formation (5, 17). The incidence of an arterial puncture during infraclavicular SV catheterization has been reported to range from 3% to 5.7% with the MP approach in cardiac surgery (2-4). In our study, the incidence of accidental arterial puncture was significantly higher in the LA technique (10.5%) than in the MP technique (1.4%) using a landmark-based technique.
Finally, in the present study, there were no significant differences in complications such as hemothorax, hematoma at the puncture site, and pneumothorax between the techniques. It must be noticed that although point-of-care ultrasound (POCUS) and real-time ultrasound-guided techniques possess advantages such as higher success rate and efficiency, they have some limitations such as the need for skilled labor, time-intensiveness, no availability at all medical facilities (such as our hospital), and inability to prevent the malposition of the catheter tip (1, 18).
5.1. Limitations
The blindness of the physician was not possible in the present study.
5.2. Conclusions
The results of the present study indicate that although the incidence of malposition of catheter tips is significantly lower in the LA approach than in the MP approach, the LA approach seems not to be an appropriate alternative to the MP approach for SV catheterization with a landmark-based technique.