1. Background
The application of opioids is the main method to control the postoperative pain (i.e., oral, intravenous, mucous, and hypodermic). Nowadays, opioids are widely used in the form of patient-controlled analgesia (PCA) pumps (1).
A patient-controlled intravenous pump is an important method to relieve pain, which allows the patient to take the required bolus dose of analgesic based on the severity of the pain using the injection pumps with the scheduled capacity for relieving pain (2, 3). Although this method increases the chance of Hemodynamic changes, but one of its benefits is providing medication whenever needed, which reduces anxiety and stress that are the main factors causing postoperative pain (4).
Due to their high effectiveness in pain management, opioids are the most commonly-prescribed drugs; however, because of their numerous side effects, researchers have always been interested in finding alternative or adjunctive drugs. As a result, several drugs are proposed that can effectively be used to control postoperative pains, including Paracetamol, Ketamine, Dexmedetomidine, Gabapentin, Pregabalin, Lidocaine, Amantadine, Melatonin, and Ketorolac (5).
Nitroglycerin typically uses for angina as a vasodilator. However, in previous studies, it's administered as an analgesic for non-anginal pains (6). Some studies investigated the effectiveness of nitroglycerin in relieving the pain of patients who had arthroscopic knee surgery (6), chronic pain after thoracotomy (7), and diabetic neuropathy (8). Researchers also reported that the systemic use of nitroglycerin was useful in patients who had spinal anesthesia (9).
In another study (10) three groups were investigated, including A (fentanyl 10 µg/kg + 10 mL distilled water), B (fentanyl 10 µg/kg + nitroglycerin 500 µg), and C (fentanyl 10 µg/kg + nitroglycerin 1000 µg), and it was found that the group C had the lowest pain. Although the effect of nitroglycerin on hemodynamic was higher in this situation, but no significant difference was observed between these groups in terms of MAP and HR.
2. Objectives
Above all, to reduce side effects, the best postoperative pain-relieving method should be investigated. Therefore, the current study aimed to investigate the effects of adding nitroglycerin as a nitric oxide imitator to the morphine available in the pain pump to reduce the post-surgery pain.
3. Methods
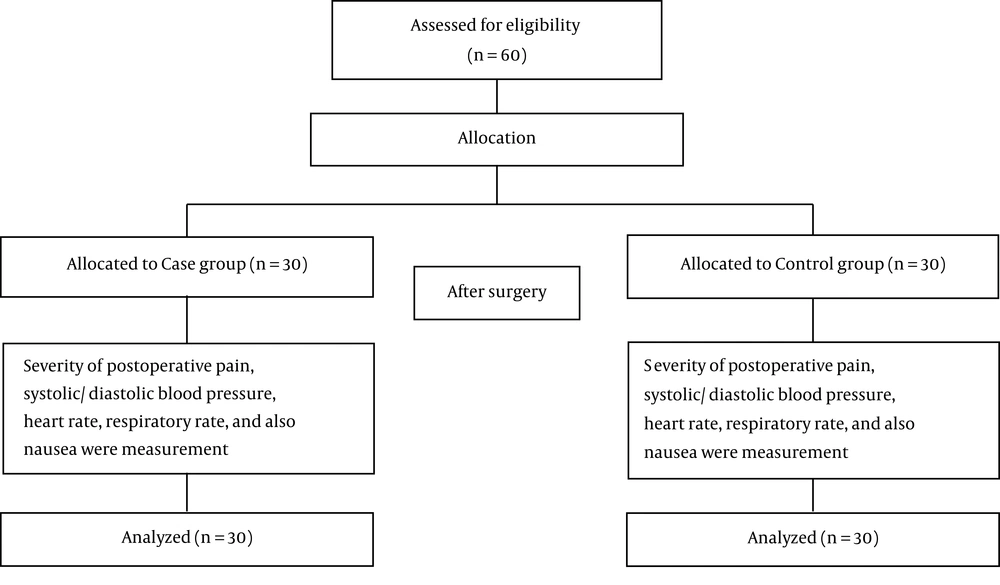
The current study is approved by the Ethical Committee of Birjand University of Medical Sciences (Ir.bums.REC.1395.194). Also, the study is registered in the Iranian Registry of Clinical Trials (IRCT20140519017756N33). A double-blind clinical trial was used to investigate and compare the analgesic and hemodynamic effects of nitroglycerin-morphine sulfate or morphine sulfate alone. The study was conducted on 60 patients (18 - 50 years old) with the American Society of Anesthesiologists (ASA) 1 and 2. The patients were candidates for simple elective surgery (cholecystectomy, jejunoileostomy, etc.). The flow diagram of the current study is presented in Figure 1.
The inclusion criteria were being aged 18 to 50 and anesthetic classes 1 and 2 (i.e., the patient did not take any sedative and antiemetic medications and had no history of drug abuse. All abdominal surgeries took less than two hours, bleeding volume was less than 200 mL, and surgical incision length was less than 10 cm. Exclusion criteria were as follows contraindications, nitroglycerin, and morphine drug allergy, severe nausea and side effects (such as hypotension, headache, vomiting, and arrhythmias). Besides, the side effects occurred during the pump usage should be treated, which complicates surgical operations.
In a study performed by Gabriela R and colleagues, initially, the sample size for each group was estimated at 22. However, they increased the sample size to 30 to minimize the impacts of attrition bias and to increase the inaccuracy of results.
Patients were divided into two groups (i.e., case and control groups). For both groups, the following procedures were performed in the operating room: systolic and diastolic blood pressure monitoring, automatic and non-invasive mean arterial blood pressure monitoring, constant measurement of arterial blood oxygen by an oximeter pulse, constant electrocardiogram recording by a 5-lead method, and fluid prescription after the reception.
Surgery was performed using general anesthesia. The anesthesia in both groups was induced equally using propofol, fentanyl, and muscle relaxant with dosages of 2 mg/kg, 3 µg/kg, and 0.5 mg/kg, respectively. All patients were intubated with an endotracheal tube by an anesthesiologist. Bleeding and other outflow parameters were monitored both during and after the surgery. After transferring patients to the recovery room, the Iv PCA with a capacity of 100 ml (adjustable in 2, 4, 6 & 8 mL/h) was filled by an anesthesiologist, and it was kept at the dose of 4 mL per hour. For the control and case groups, morphine sulfate 10 mg/ml (Morphine, Darupakhsh Co., Iran) (0.75 mg/mL) and nitroglycerin-morphine (morphine 0.5 mg/mL + nitroglycerin 10 mg/2mL (Nitral, Caspian Tamin Pharmaceutical Co., Rasht, Iran) 15 μg/mL) infusions were administered. In each group, the remaining part of the pump volume was filled up to 100 ccs with normal saline. A demographic information form (including information on age, sex, anesthesia classification, and vital signs) was completed for all patients. Then, hemodynamic and breathing parameters, nausea and vomiting, and pain were measured based on a VAS Score immediately, 2, 6, 12, and 24 hours after the surgery.
The visual pain scale is a unidimensional measure that contains two ends ranging from 0 to 10. “no pain” on the left (i.e., 0) and “hurt worst” on the right (i.e., 10). Generally, scores in the ranges of 1 - 3, 4 - 7, and 8 - 10 indicate mild, moderate, and severe pain, respectively. Data were analyzed by SPSS version 20 using the t-test (age, pain, hemodynamic parameters of systolic and diastolic blood pressure, heart rate, and breathing rate of the patient) and Mann-Whitney U-test (surgery period and nausea) and the homogeneity was checked by the Kolmogorov-Smirnov test.
4. Results
The data were collected to analyze the effect of adding nitroglycerin to morphine in PCA on the pain relief after surgery in two groups, each with 30 patients. In the case group, 16 patients (53.3%) were male and 14 (46.7%) were female. However, in the control group, 18 patients (60%) were male and 12 (40%) were female. The mean age of the case and control groups was 36.93 and 33.30, respectively. As mentioned before, there was no significant difference in terms of age and sex between the two groups.
Mean pain scores, according to the VAS Score of the surgery, for both groups are provided in Table 1. Based on the results, the scores were only negligibly different.
| Time (h) | Groups | P Value | |
|---|---|---|---|
| Case | Control | ||
| Pain | |||
| Immediately after surgery | 6.2 ± 2.35 | 6.14 ± 2.65 | 0.71 |
| 2 | 5.03 ± 2.35 | 4.36 ± 2.32 | 0.19 |
| 6 | 3.3 ± 2.18 | 3.06 ± 1.98 | 0.47 |
| 12 | 2.3 ± 1.5 | 2.24 ± 1.57 | 0.71 |
| 24 | 1.26 ± 1.7 | 1.1 ± 1.39 | 0.91 |
| Systolic blood pressure | |||
| Immediately after surgery | 130.93 ± 18.16 | 123.5 ± 14.16 | 0.092 |
| 2 | 125.5 ± 18.16 | 116.48 ± 14.21 | 0.031 |
| 6 | 121.66 ± 15.88 | 116.2 ± 12.65 | 0.167 |
| 12 | 119.93 ± 16.38 | 115.17 ± 13.85 | 0.234 |
| 24 | 118.86 ± 20.19 | 108.4 ± 17.1 | 0.037 |
| Diastolic blood pressure | |||
| Immediately after surgery | 80.1 ± 12.45 | 77.79 ± 11.63 | 0.472 |
| 2 | 79.3 ± 10.96 | 70.2 ± 15.46 | 0.010 |
| 6 | 78.83 ± 9.97 | 72.68 ± 10.07 | 0.021 |
| 12 | 76.5 ± 8.82 | 72.06 ± 8.18 | 0.050 |
| 24 | 75 ± 10.66 | 69.31 ± 3.37 | 0.016 |
| Heart rate | |||
| Immediately after surgery | 82.15 ± 15.02 | 73.82 ± 10.9 | 0.011 |
| 2 | 83.42 ± 13.92 | 80.41 ± 10.64 | 0.324 |
| 6 | 79.9 ± 13.64 | 80.51 ± 8.48 | 0.769 |
| 12 | 78.93 ± 11.43 | 79.93 ± 9.2 | 0.714 |
| 24 | 76.06 ± 9.91 | 69.51 ± 23.37 | 0.164 |
aValues are expressed as mean ± SD.
Furthermore, the systolic blood pressure 2 and 24 hours after the surgery (case group) was significantly higher than that of the control group (P = 0.031 and 0.037, respectively). Also, aside from 2 hours after the surgery, the diastolic blood pressure was substantially higher in the case group.
According to the results, the heart rate was significantly lower in the control group only immediately after the surgery.
The mean breathing rate of patients, except for immediately after the surgery, was highly lower in the control group.
Finally, the results revealed that the mean score of nausea was consistent in both groups at any time after the surgery.
5. Discussion
The current study evaluated the effects of nitroglycerin on abdominal surgery using general anesthesia and the PCA method. Based on the results, administration of the nitroglycerin resulted in a significant decrease in the mean score of postoperative pain; thus, morphine-alone or morphine-nitroglycerin had significant pain relief effects at least 24 hours after surgery. However, there was no large discrepancy in the mean pain score between the two groups. A study has reported that prescribing Dexmedetomidine in lower than normal doses of non-opioid analgesics, such as ketorolac, is effective in controlling postoperative C-section pain while it helps to achieve optimal analgesia without causing any major complication (11). Some reported contradicted findings. According to some studies adding nitroglycerin to drugs (such as neostigmine and nalbuphine) resulted in further reduction of pain and increased duration of analgesia (12, 13). The current study also investigated the hemodynamic variables, including systolic and diastolic blood pressure. The mean systolic blood pressure was considerably small in both groups after the surgery; however, it was higher in the case group.
On the other hand, mean diastolic blood pressure was dramatically reduced only in the control group. By contrast, Jeon (14) demonstrated that adding nitroglycerin to lidocaine did not alter hemodynamic variables such as blood pressure. However, another study suggested that nitroglycerin infusion had partially successful hemodynamic effects during laparoscopic low anterior resections (15)
Derakhshan et al. (16) investigated the effects of nitroglycerin on pain control and reported that it decreased both systolic and diastolic blood pressure. This decrease might be due to nitroglycerin vasodilatation and lower vascular resistance by hypotension. Although in the present study adding nitroglycerin decreased the systolic and diastolic blood pressure, the systolic and diastolic blood pressure indices were stable in the case group.
Moreover, although there was a significant increase in the mean heart rate during the early hours after the surgery, but it was observed in both groups. It worth noting that in the case group no heart rate fluctuation was observed.
Consistent with the findings of the current study. The results of the study conducted by Derakhshan et al. (16) also showed a decrease in heart rate after receiving nitroglycerin. However, the mean heart rate negligibly changed after taking the drug. These results confirm the higher stability of the hemodynamic index in the case group.
Further, the mean respiratory rate was hugely higher in the control group, apart from early hours after the surgery, which was close to its standard level, due to the presence of nitroglycerin.
5.1. Conclusions
Based on the findings of the present study, combined administration of nitroglycerin and morphine had no synergistic effects on reducing postoperative pain. However, the addition of nitroglycerin to morphine can further stabilize hemodynamic parameters. Also, it can improve patient breathing without any side effects.
5.2. Limitations
In the current study, only the effect of adding nitroglycerine to morphine on the control of pain was investigated. However, the effect of this drug on the reduction of morphine dose was not addressed. We recommend investigating the effect of nitroglycerin alone (in comparison to opioids) on surgical procedures in future studies.