1. Introduction
Hydatid disease is a zoonotic infection caused by larval forms of Echinococcus granulosus. The definite hosts of Echinococcus are various natural domestic carnivores, the common being the dog. All mammals (more often being sheep and cattle) are intermittent hosts. Humans usually get infected by ingestion of the food contaminated by dog feces containing ova of the parasite or by direct contact with dogs (1, 2). The liver involvement is the most frequent manifestations of echinococcosis. However, some larva may occasionally reach the lungs, where it is the second most common echinococcosis manifestations. In rare cases, larva gets entry into the systemic circulation, to the brain, or bone (3). The disease is endemic in many regions of the world, particularly in the Middle East, Mediterranean countries, Australia, New Zealand, South America, and central and South Europe. Iran is among the countries with a high incidence of hydatid disease (4). Hydatid cyst management is surgical excision of the entire cyst without rupture. In some cases where cyst is deep-seated, located in critical areas, or in general, when it is felt that removing the intact cyst is unlikely to succeed, aspiration of the cystic contents through puncturing is an alternative method.
2. Case Presentation
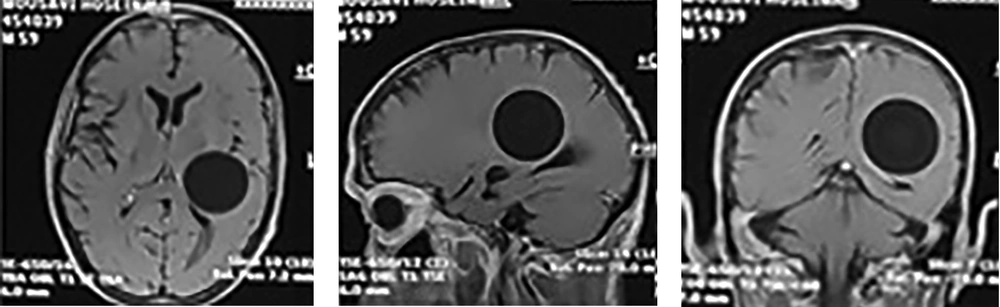
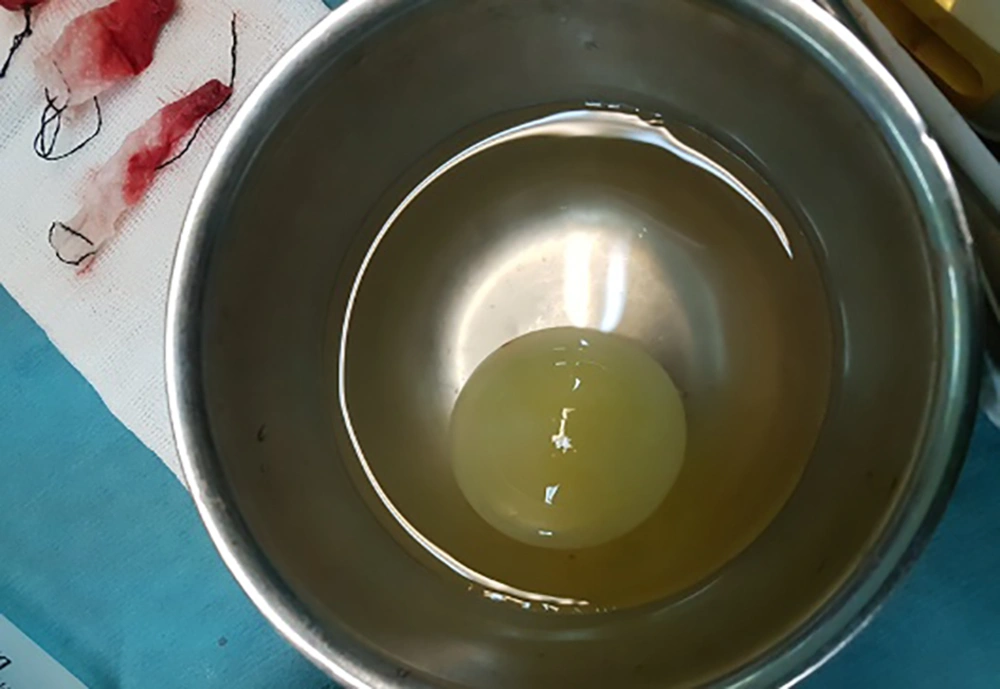
A 59-year-old male was referred to our hospital with complaints of headaches and progressing dysarthria for the last two months, right sided hemiparesis, and altered consciousness at the date of admission. On the physical examination, he was disoriented with right sided hemiparesis and normal vital signs. He was a shepherd from Malayer (located in the central part of Iran) and a 20 pack-year smoker without any significant medical history or opium abuse. The initial CT-scan and MRI revealed a large spherical supratentorial well-defined cystic lesion in the left parietotemporal lobe. This single large cyst had a mass effect on the left ventricle without a midline shift or notable edema (Figure 1). Chest x-ray, and abdominal and pelvic sonography were negative without any notable findings. Liver enzymes level was in the normal range like other laboratory reports. The plan of the neurosurgery teams included surgery and removal of the lesion. In the operating room he had mild disorientation and normal vital signs. Premedication included midazolam 0.03 mg/kg and fentanyl 3 µ/kg, then induction was performed with propofol 2 mg/kg and atracurium 0.5 mg/kg. We used propofol and remifentanil infusion, and atracurium as maintenance. Position was supine and the pin head-holder was used to fix the skull. After surgical exposure, we changed the position of the bed to the trendelenburg position and the bed tilted toward the lesion aiming to push the cyst outward by increasing the intra cranial pressure. In this step we avoided any medication that could possibly decrease the ICP (mannitol, furosemide). Another strategy we followed was the intentional mild hypoventilation to increase Etco2 coupled with applying the valsalva maneuver at the final steps of cyst expulsion. We were also ready and equipped for possible anaphylactic reaction in case of cyst rupture. The entire cyst was delivered successfully without any rupture (Figure 2). The patient was discharged after six days with improved signs and good condition.
3. Discussion
Surgical excision of cyst in total is the method of choice in the treatment of cystic echinococcosis. Various atraumatic techniques of cyst removal have been designed to avoid rupture (1). The most popular surgical procedure for intact removal of the cyst is Dowling-Orlando technique, in which cysts are removed all together by mean of hydrodissection. In this technique, head of the operating table is lowered and irrigation with hypertonic saline is used with mild force between the cyst wall and the surrounding brain parenchyma to deliver the cyst intact.
It is recommended to clean the area with sodium chloride, which decreases the chance of recurrence (5-8). Few reports are available mentioning the efficacy of treatment with anti-helminthic drugs, albendazole, and mebendazole, especially for patients suffering from multiorgan and multicystic disease, having inoperable or deep-seated cysts, and those who are at risk for surgery. These drugs act through impairing uptake of glucose by the larval and adult stages of the susceptible parasites, leading to depletion of glycogen storage and thereby, decreasing the ATP formation and death of the parasite. Albendazole can also be administrated as a preventive treatment to sterilize the cyst and reduce the tension in the cysts wall, which decrease the rate of recurrence in case of cyst rupture (9).
However, as surgical excision of intact cyst is the treatment of choice, certain intra-operative challenges, depending on the location, the size, the number of cysts, and the applied technique, should be considered. Bacterial infection, cyst rupture, and anaphylactic reactions to antigenic contents of cyst are the possible complications of hydatid disease (10).
As mentioned, total surgical excision of the cyst is critical, because even minimal spillage can have life threatening consequences. Some major problems encountered during the surgical procedure include, periventricular location of cyst, its thin wall, and micro-adhesions to the brain parenchyma. If hydatid cyst is ruptured, its highly antigenic contents are released into the circulation, leading to IgE mediated anaphylactic reactions. The severe anaphylaxis is followed by immediate hypersensitivity reaction and increased airway pressure due to bronchospasm. The immunologic symptoms can range from mild urticaria to severe anaphylactic shock (6, 11-13). In this case, high index of suspicion and early aggressive operative treatment with intravenous epinephrine infusion along with administration of 100% oxygen and massive fluid resuscitation are necessary to minimize the life threatening risk of anaphylaxis. Prophylactic hydrocortisone supplementation for the prevention and treatment of refractory hypotension is recommended as well.
Cardiovascular signs including hypotension, tachycardia and arrhythmias are frequent under anesthesia. Despite that, the incidence of severe bronchospasm during general anesthesia is rare. Anesthesia is also potentially associated with cutaneous symptoms such as rash, flushing and urticaria, however, they are often difficult to detect due to being masked with surgical draping. As cutaneous manifestations are the most common symptoms of anaphylaxis and in most cases, cyst rupture, anaphylaxis is reported to occur within minutes of spillage of the contents, its diagnosis should be established with considerable caution, using precise immunologic evaluation.
In addition to mentioned complications, the surgical excision of the cyst is associated with risk of increased bleeding during dissection. Usually swollen cyst may compress the vessels; however, after opening the dura and cyst excision, such pressure is relieved, resulting in increased blood flow to surrounding fragile tissues, and thus, raising the risk of excessive bleeding. Hence, preparation for possible massive blood loss (e.g. ensuring sufficient blood products) and its management prior to operation of infected cystic lesion is crucial.
Moreover, removal of large cysts leaves a cavity, which can lead to disruption of the cerebral structures and post-operative neurological complication (11). Epidural hematoma, development of subdural effusion, and pneumocephalus are among other reported complications of hydatid cyst surgery (14).
On that account, all mentioned challenges should be well thought out and, more importantly, planned by the anesthesiologist, preoperatively. The exact surgical procedure, depending on size and location of cyst as well as general condition of patient should be defined. Besides, close cooperation between surgery and anesthesiology personnel is essential for proper performance of this technique.
In detail, the anesthesiology team needs to control surgical field bleeding and prepare a stable condition for the surgeon to excise the cyst smoothly. It is also noteworthy to mention that, although lowering the intracranial pressure (ICP) is a critical component of anesthesia in neurosurgical procedures to provide a better surgical access to the cyst, in some cases increasing ICP at some stage of surgery can serve to push the cyst outward. Thus, increasing Paco2 level by hypoventilation and even valsalva maneuver may be used along with trendelenburg position.
In general, as operation of cerebral hydatid cyst is associated with the risk of massive bleeding and anaphylactic shock, the anesthesiologist should be well prepared and equipped for management of these challenging conditions.
Here, we reported a successfully managed case of giant cerebral hydatid cyst in a 59-year-old male with headache, dysarthria, and hemiparesis. Conclusively, several precautions should be applied intraoperatively by the operating team as ruptured cyst may cause life threatening consequences