1. Background
Stroke is considered to be one of the leading causes of mortality and disability in elderly patients. Annually, 15 million people around the world have suffered a stroke. Of those, 5 million die and 5 million are left with a disability, putting a burden on family and healthcare systems (1-3).
Numerous rehabilitative approaches aim to enhance patient independence, one such example is the use of mental representation of a motor action (4). Motor imagery (MI) practice is the mental rehearsal of movement without any motor output (5). it is a complex mental process that integrates sensory and perceptual abilities to perform the motor acts at the level of the working memory without performing them physically (6, 7). The main objective of mental practice is to improve motor performance in patients with physical disabilities, such as in stroke patients (8, 9).
Specifically, there are two major forms of motor imagery: visual, in which the individual imagines themselves as an external observer, and kinesthetic, in which the individual tries to experience a sensation of the imagined movement within his body (10, 11). In task-specific training, a type of feedback is received following the practice of context specific motor tasks (12). Examples of motor tasks include holding objects and pouring liquids, with the aim of improving functional motor outcome (13). However, repetition alone without showing the importance of the repeated movement by including it in an important task that matters to the patient, is not enough to increase motor cortical representations, whereas task-specific training of the more affected limb can be associated with significant functional improvements (14).
2. Objectives
An important advantage of MI is that patients can do it independently, without help from others, without the need for special equipment, or having to travel to get the service. This is extremely beneficial during the early stage of stroke, where individuals can rehearse and imagine a task that they cannot physically accomplish due to motor disability.
3. Methods
From May 2018 to June 2019, thirty male patients with ischemic stroke were selected from the outpatient clinic to participate in this study. The median age of the study participants was 54.5 ± 3.51 years. Patients were divided into two equal groups. Group A (study group) received motor imagery training for 15 minutes followed by task specific training for 45 minutes, as well as a selected physical therapy program thrice per week for 6 weeks. Group B (control group) received task specific training for 45 minutes, as well as selected physical therapy program thrice per week for 6 weeks.
3.1. Inclusion Criteria
Patients included in the study were right-handed, ranged from 50 - 60 years old, and all suffered from hemiparesis due to ischemic stroke. Patient’s scores on the National Institute of Health Stroke scale (NIHSS) ranged from 8 - 16. Also, in order to ensure that patients met study requirements, patients were included if: rated 3 on the five-point scale of the kinesthetic and visual imagery questionnaire version-10 (KVIQ-10) (15); had a minimum score of > 10 seconds on the timed up and go test (TUG test) (16), with at least 2 minutes of standing and 2 minutes of upright sitting with no support to the back; scored at least 21 on the Mini Mental State examination (MMSE), to ensure good cognitive functions (17).
3.2. Exclusion Criteria
Patients were excluded from the study if they experienced severe aphasia, hemineglect, cognitive impairments that could interfere with the comprehension of the study or their abilities to respond well to the required tasks. The exclusion criteria also included disabilities caused by diseases other than stroke such as dementia, parkinsonian syndromes, and brain tumors.
The following were utilized for patient assessment: Fugl-Meyer assessment lower extremity (FMA-LE), The Biodex Balance system, TUG test and KVIQ-10. The first three abovementioned tests were performed before and after treatment, while the last questionnaire was completed prior to treatment.
The FMA-LE is used to evaluate motor and sensory impairment of the paretic lower limb after stroke. The assessment took approximately 45 minutes to complete. In this test, the following areas are assessed: In this test 5 domains are assessed; lower extremity, coordination/speed, sensation, passive joint movement and pain. The maximal scores are 28, 6, 12, 20, 20, respectively, the higher the score, the better the patient performance (18).
The Biodex Balance system tests the ability of the individual to maintain their balance while standing on a moveable platform. The SD (L9402), Biomed Service device was used. The Biodex Balance system is an effective method that is used for balance assessment and treatment. It is utilized to address and assess the following: overall stability index (OSI), anterior-posterior stability index (APSI), and medial-lateral stability index (MLSI) (19).
The TUG test is used to assess mobility. A healthy elderly patient is able to complete the test in 10 seconds or less. The patient sits in a chair with arm rests, and a piece of tape is put on the floor 3 meters away from the chair. The patient stands up walks to the tape, returns to the chair and sits back down. The test time is calculated from the patient sitting on the chair, moving up to a standing position, and then returning to sit down on the chair again (20).
In this study, the KVIQ-10 questionnaire was used to assess the motor imagery of stroke patients prior to the start of training. This version of the questionnaire includes 10 items, specifically 5 movements in each of the Visual and Kinesthetic subscales (15).
The designed physical therapy program, which was assigned to both groups included: strengthening exercises for the weak lower limb muscles, core stability exercises, balance training, postural and lower extremity control.
In the first part of this study, motor imagery training was assigned to group A. It was conducted in a quiet room, where each patient was given detailed instructions to perform both visual and kinesthetic practice. For the visual imagery, we asked the patient to imagine doing the requested movement and feeling all the bodily sensations just as if they were viewing all of their movements from the outside. Patients were instructed that while their eyes are closed, they had to see and feel the performance of a particular movement in the most comfortable way for their body without contracting any muscles.
For the kinesthetic motor imagery training, each patient tried to experience the sensations associated with the imagined movement within their body. A quiet environment was maintained and very clear instructions were issued. Prior to the start of the study, patients were trained well in order to achieve the desired response.
Patients were requested to inform us when they completed the imagery task, at which point the time was recorded (21). Practice of the 2 tasks consisted of relaxation and presentation of the imagined environment (2 - 3 minutes), followed by practice of visual imagery (5 - 7 minutes), then practice of kinesthetic imagery (5 - 7 minutes), and lastly a phase of back to the environment (1 - 2 minutes). The content of the imagery practice was changed on a weekly basis by augmenting and altering difficulty levels. The duration of the training period for motor imagery was 15 minutes thrice a week for 4 weeks (22).
The motor imagery for the sit to stand (STS) imagery intervention program, was only assigned to group A. The sit to stand imagery training was for a period of four weeks. Patients were training in both Visual and Kinesthetic motor imagery. Week 1; the sit to stand task was done as one block. Week 2; the phase of transfer from anterior acceleration of the trunk until separation of the buttocks from the chair was trained. Week 3; the stabilization phase was trained at which there is an extension of the hips and the knees associated with straightening of the trunk until complete stance. Week 4; the STS task was practiced again as a whole one block, but with different speeds. The patterns of motor imagery practiced each week for the STS task over the 4-weeks period was escalated gradually, in terms of practice frequency (23).
In the second part of this study, task specific training was assigned to both groups A and B; however, task specific training for group A was assigned following motor imagery. When training for the STS task via task specific training, patients are initially trained using the higher then the lower chair, as with lowering the chair the need for force generation is increased (24). Patients were trained with their feet on two weighing scales in order to provide visual feedback to increase weight-bearing on the affected leg, thus improving muscle strength. Auditory feedback may be used as well to decrease the need for looking downwards at the scales, consequently altering the patient’s body kinematics (25).
Part-practice was applied only for 1st two phases of sit to stand task, which are the most problematic. It was used when the patient was unable to perform a full STS without standby help. The patient sat on the chair, and his vision and attention were directed toward an external focus (green cones) that helped the patient to exert more equal weight on both lower limbs, thus improving motor learning (25). Next, the patient was instructed to lean his whole body forward making his knees touch the green cones and then sit back down.
Twelve patients were lost to follow-up and their data was excluded from the study.
3.3. Data Analysis
The demographic characteristics of the patients were collected and statistically analyzed using descriptive statistics. Paired sample t-tests were utilized to evaluate statistical differences between the study and control groups in all variables (i.e., Biodex indices, TUG and FMA-LE).
4. Results
In this study patients were divided into two equal groups, A and B. In group A patients received motor imagery training for 15 minutes followed by task specific training for 45 minutes, as well as a selected physical therapy program. In group B patients received task specific training for 45 minutes, as well as a selected physical therapy program. Demographic and comparison data are noted in Table 1.
In regards to Biodex indices, both study groups achieved statistically significant improvement after the designed rehabilitative plan; however, in a comparison between groups, the study group that received motor imagery training, showing greater statistically significant improvement than the other group. The P value post-test between group A and group B of MLSI, APSI and overall stability index were significant (P = 0.0141, P = 0.0001, P = 0.0001) as shown in Table 2.
| Variable | Pre-Therapy | Post-Therapy | t Value | P Valueb |
|---|---|---|---|---|
| MLSI angle, s | ||||
| Group A | 5.113 ± 0.2825 | 4.5 ± 0.2138 | 6.705 | 0.0001c |
| Group B | 5 ± 0.2535 | 4.707 ± 0.2187 | 3.393 | 0.0021c |
| t value | 1.156 | 2.617 | ||
| P valueb | 0.2573 (NS) | 0.0141c | ||
| APSI angle, s | ||||
| Group A | 6.205 ± 0.1664 | 5.620 ± 0.1373 | 10.507 | 0.0001c |
| Group B | 6.311 ± 0.1791 | 6.053 ± 0.2100 | 3.621 | 0.0012c |
| t value | 1.679 | 6.689 | ||
| P valueb | 0.1042 (NS) | 0.0001c | ||
| Overall SI angle, s | ||||
| Group A | 6.747 ± 0.1246 | 6.173 ± 0.1751 | 10.332 | 0.0001c |
| Group B | 6.820 ± 0.1859 | 6.560 ± 0.1844 | 3.845 | 0.0006c |
| t value | 1.269 | 5.889 | ||
| P valueb | 0.2149 (NS) | 0.0001c |
Abbreviations: APSI, Anteroposterior Stability index; MLSI, Mediolateral Stability index; SD, standard deviation.
aValues are expressed as mean ± SD.
bProbability value.
cSignificant level is set at an alpha level < 0.05.
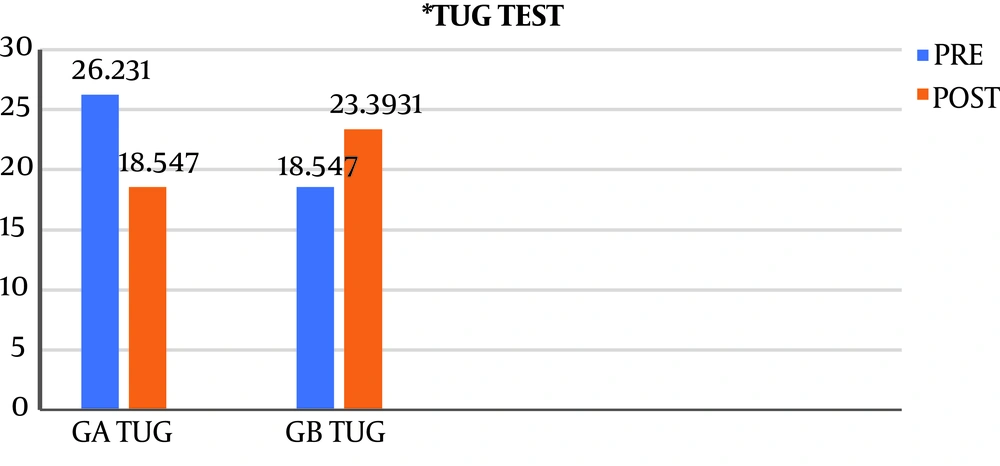
With reference to the TUG test, group A showed a statistically significant reduction in the mean number of seconds needed for the test, denoting an improvement after the implementation of the treatment plan (P value = 0.0001). This improvement did not apply to group B. Interestingly, group B showed a statistically significant worsening in the mean time when comparing before and after treatment plan data. There was a statistically significant difference between group A and group B post-therapy, (P value 0.0001) as shown in Figure 1 and Table 3.
Abbreviations: SD, standard deviation; TUG, timed up and go test.
aValues are expressed as mean ± SD.
bProbability value.
cSignificant < 0.05.
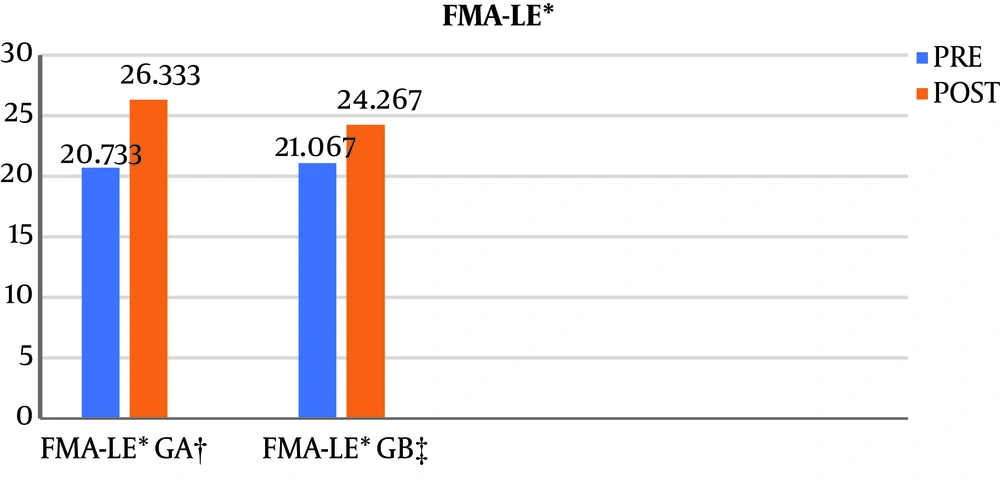
Regarding the FMA-LE test results, both groups showed statistically significant improvement pre- and post-test. The mean scores for the test were in favor of group A, with statistically significant results for the post therapy only (P-value 0.0004), as shown in Table 4 and Figure 2.
Abbreviations: FMA-LE, Fugl-Meyer assessment lower extremity; SD, standard deviation.
aValues are expressed as mean ± SD.
bSignificant < 0.05.
Concerning the speed of STS movement, the speed of movement showed better increase and improvement in group A when compared to group B post therapy, (P value 0.0001). The results are noted in Table 5.
aValues are expressed as mean ± SD.
bProbability value.
cSignificant < 0.05.
5. Discussion
This study aimed to investigate whether task specific training preceded by motor imagery or task specific training alone was more effective for facilitating sit to stand in patients with stroke. Both visual and kinesthetic imagery practice were utilized to account for individual differences in compliance and tolerance. Another reason for combining both types of imagery practice is the privilege you get when processing 2 integral sensations. In addition, previous research studies have included training with both visual and kinesthetic types of motor imagery as it has been demonstrated to be better than training with only one of them in stroke neurorehabilitation (22, 26).
The statistical analysis revealed that there were statistically significant differences in all variable scores before and after treatment within both groups. Moreover, there were highly statistically significant differences after treatment in favor of the study group. The improvement in the Biodex indices observed in the study group was consistent with the systematic review conducted by Zimmermann-Schlatter et al. (8) on the efficacy of motor imagery in post-stroke rehabilitation. In their study, they concluded that compared to conventional physiotherapy, motor imagery provided additional benefits in stroke patients (8).
In another systematic review the connection between motor imagery and mental practice on post-stroke functional recovery was investigated; and it was reported that mental practice improved spatial and temporal parameters of gait, as it decreased the apprehension of falling and reinforced earlier gait retraining (4).
These results correlate with a study conducted by Verma et al. (27) who assessed the effectiveness of a task-oriented gait rehabilitation training program when added to mental imagery, and found statistically significant improvements were achieved in regards to independent functional gait. A case report written by Jackson et al. (28) reported that after combined motor imagery practice and physical therapy, sequential foot movements showed significant improvement in patients with hemiparesis.
Ehrsson et al. (29) found that brain regions that are responsible for motor function are activated during motor imagery. In addition, focal enhancement of motor cortex excitability occurs and enhances relearning and generalization of daily tasks after stroke (30). These findings can explain the effect of motor imagery techniques on the brain and on the effectiveness of the rehabilitation process. In a controlled clinical trial, Hwang et al. (31) found statistically significant improvements in clinical gait assessments in the study population receiving motor imagery techniques in the physiotherapy program. The clinical gait assessment parameters included gait speed, length of stride, and dynamic balance. These improvements can be explained by the transfer of skills and the psychological aspects of mental imagery, such as a decrease in the fear of falling (31).
In the current study, the progress achieved by the study group in the Fugl-Meyer score (FMA-LE) can be clarified by a study conducted by Porro et al. (32). By utilizing functional magnetic resonance imaging (fMRI), they found that during the actual execution of motor function there was increased neural activity in brain regions, which overlapped with brain regions activated during motor imagery practice. The activation of neuronal networks included those in the areas of movement preparation (32).
In the current study, the improvement in the TUG test noted in the study group was consistent with the findings of Dunsky et al. (33) who assessed the outcome of home-based gait training by motor imagery. Significant improvement was noticed in patient walking speed, and such improvement was detected for up to 3 weeks during patient follow-up. Improvement was most evident in cadence, time of single support for the weak leg and stride length (33).
Malouin et al. (34) found that after only one training session of motor imagery, stroke patients showed an improvement in the weight bearing abilities of the paretic limb while standing, such improvement continued for 1 day. Mental practice, through involvement of a learning effect, plays a significant role in the memorization of newly acquired motor abilities (34, 35). Motor imagery preceding task specific training has proven to improve functional outcomes, such as the sit to stand function, in hemiparetic stroke patients when compared to task specific training alone.
5.1. Conclusions
Motor imagery is a safe, accessible, inexpensive and effective therapeutic technique for motor rehabilitation in conjunction with task specific training for functional rehabilitation in stroke patients.