1. Background
Although several preventive strategies are available to prevent infection in patients who use external ventricular drains (EVDs), still 27% of these patients are at increased risk of infection (1-3). These patients are usually hospitalized at the Intensive Care Unit (ICU) in order to manage high intracranial pressure that may occur in several conditions such as intracranial hemorrhage, tumor, and hydrocephalus (4). Many risk factors are associated with EVDs infection, including different diagnosis, co-infection(s), neurosurgical operation, length of tunneling > 5 cm, catheterization for more than 11 days, intracranial pressure monitoring for more than 5 days, catheter type, repeated insertion of the catheter, and multiple catheter replacement (5, 6).
Several studies have investigated EVD-related infections, which reported an incidence rate of nearly 20% and various risk factors. EVD Infections not only increase the length of ICU and/or hospital stay, but also are associated with increased risk of morbidity and mortality of patients. Hence, identifying factors that increase the risk of such infections is necessary.
2. Objectives
This survey aimed to investigate predictive factors for EVDs infection in patients admitted to the neurosurgery ICU of the Loghman Hakim Hospital during 2018 - 2019.
3. Methods
In this longitudinal following-up study, 91 patients admitted to the neurosurgery ICU of Loghman Hakim Hospital in the city of Tehran (Iran) for EVDs replacement are investigated. All patients were followed-up for 30 days for EVDs infection. Ten patients were excluded due to one of the following reasons: presenting with an open skull fracture and cerebrospinal fluid (CSF) leakage, personal hospital discharge, referring to other centers, or death due to other reasons. Also, patients who developed an infection in less than two days after EVDs replacement were excluded. All patients were on intravenous antibiotic prophylaxis before and after neurosurgery. Moreover, none of the catheters were impregnated with antibiotics. All EVDs were placed by a resident of neurosurgery with at least 2 years’ experience. Data on demographic information (i.e., age and sex), underlying disease, diagnosis, number of EVD replacements, length of hospital stay, type of consumed antibiotic before neurosurgery, length of tunneling, type of airway, duration of mechanical ventilation, duration of surgery(hours), surgeon name, APACHE II score, length of ICU and hospital stay, and symptoms of the infection were collected. Laboratory tests (i.e. serum and CSF analysis) were also recorded. According to the Center for Diseases Control and Prevention, the criteria for ventriculitis or meningitis diagnosis are as follow: (1) positive CSF culture results plus clinical symptoms or CNS pleocytosis/cell count increase; or (2) in the case of negative CSF culture, clinical symptoms and increased pleocytosis of the central nervous system (CNS), increased serial measurement/cell count, hypoglycemia (less than 50% of simultaneous blood sugar), and increased lactate (more than 2 mmol/dL or 36 mg/lit) or gram-positive smear. In cases of suspected colonization, the simultaneous lumbar puncture was used. If there was intraventricular hemorrhage (IVH) or subarachnoid hemorrhage (SAH), correction of pleocytosis, based on concurrent blood counts, was administered (7-9). All diagnoses were confirmed by several infectious specialists. This study was approved by the ethical committee of Shahid Beheshti University of Medical Sciences, Tehran (ethic code: R.SBMU.RETECH.REC.1397.343).
3.1. Statistical Analysis
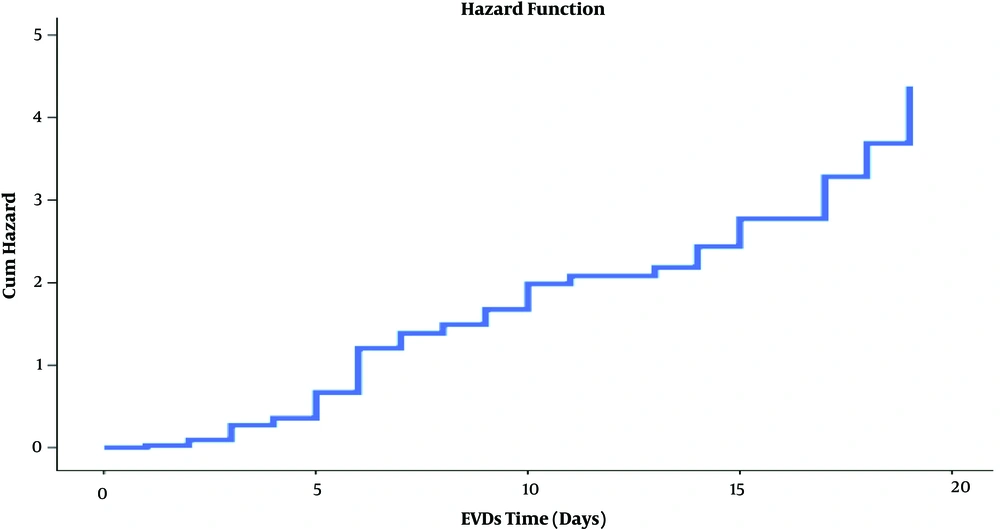
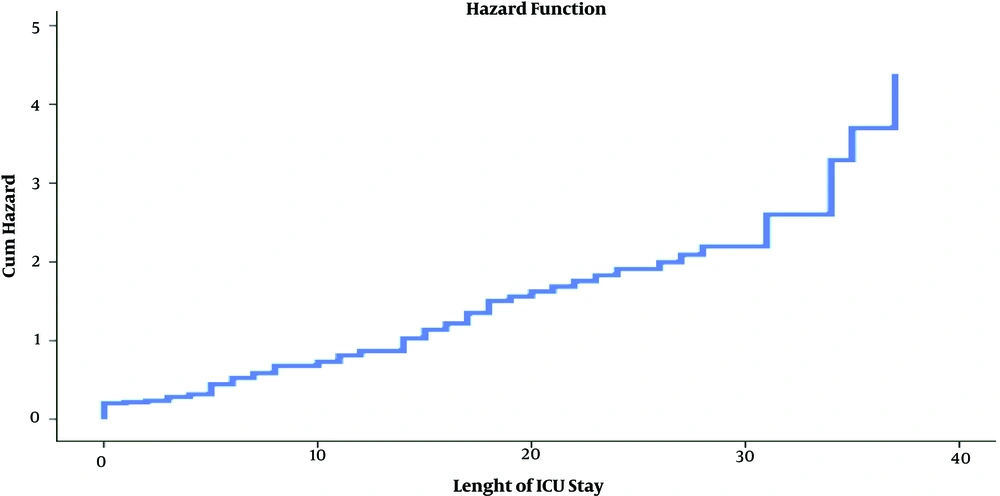
Descriptive results are reported using the mean, standard deviation (SD), and number and percentage. Bivariate analysis was performed to define the risk factors associated with infection, represented by relative risks and 95% confidence intervals. The chi-square and two-tailed Fisher’s exact tests were used for categorical variables. The independent t-test was used for continuous variables. A logistic regression model was developed to identify suspected risk factors of EVD infection. The model included variables that were significant at P < 0.1 in the bivariate analysis. Finally, the hazard function curve was plotted. Data were analyzed using SPSS version 19. Statistical significance was considered when P-value < 0.05.
4. Results
Of 81 eligible patients with EVDs, 39(48.1%) were infected (25 (55.6%) for males and 14 (38.9%) for female). According to the results of the bivariate chi-square analysis, there was no significant difference between participants concerning EVD infection rate, sex, age, diagnosis, medical history, APACHE II score, number of EVDs, time of EVDs, duration of surgery, type of airway, mechanical ventilation, time of antibiotic prophylaxis, CSF and serum factors analysis, and duration of ICU and hospital stay (P > 0.05) (Table 1). For those affected by EVDs and for others, the mean ± SD of the CSF lactate was 57.92 ± 28.49 and 55.81 ± 23.83 mg/lit, respectively. Mechanical ventilation for more than 6 days (OR: 2.3, 95% CI: 1.4 - 3.56, P = 0.04) and length of tunneling > 5 cm (OR: 2.5, 95% CI: 1.87 - 4.76, P = 0.01) could predict EVDs infection. In addition, those consuming ceftazidime + vancomycin were 70% less likely to develop EVD infection (OR: 0.3, 95% CI: 0.08 - 3.78, P = 0.04). The comparison between the two groups concerning the aforementioned factors is provided in Table 1. Besides, the final model of multiple logistic regression could predict the EVDs infection in patients admitted to the ICU (Table 2). There was no difference concerning the time since EVDs, so the length of ICU stay and EVDs infection but hazard function plot showed with increasing days of having external ventricular drain as well as with increasing the length of ICU stays, the incidence rate of EVDs infection increased. (Figures 1 and 2).
| Variables | EVDs Infection | P-Value | OR (95% CI) | |
|---|---|---|---|---|
| Yes | No | |||
| Sex | 39 (48.1) | 42 (51.9) | 0.1 | 2 (0.76 - 5.76) |
| Male | 25 (55.6) | 20 (44.4) | ||
| Female (reference) | 14 (38.9) | 22 (61.1) | ||
| Age | 44.33 ± 19.5 | 44.88 ± 20.57 | 0.9 | 1.7 (0.9 - 4.2) |
| Diagnosis | 0.3 | 0.7 (0.3 - 1.85) | ||
| Vascular | 23 (46.9) | 26 (53.1) | 0.4 (0.2 - 3.23) | |
| Brain tumor | 11 (47.8) | 12 (52.2) | 0.5 (0.4 - 1.45) | |
| Shunt and malformation (reference) | 5 (55.6) | 4 (44.4) | ||
| Past medical history | 0.8 | |||
| Diabetes (DM) | 2.9 (0.7 - 7.37) | |||
| Yes | 6 (50) | 6 (50) | ||
| No (reference) | 33 (47.8) | 36 (52.2) | ||
| Hypertension (HTN) | 0.3 | 0.6 (0.1 - 2.4) | ||
| Yes | 7 (389) | 11 (61.1) | ||
| No (reference) | 32 (50.8) | 31 (49.2) | ||
| Hyperlipidemia (HLP) | 0.1 | 0.7 (0.1 - 3.4) | ||
| Yes | 0 (0) | 2 (100) | ||
| No (reference) | 39 (49.4) | 40 (50.6) | ||
| Ischemic heart disease (IHD) | 0.1 | 0.3 (0.02 - 3.08) | ||
| Yes | 1 (20) | 4 (80) | ||
| No (reference) | 38 (50) | 38 (50) | ||
| Cerebrovascular attack (CVA) | 0.4 | 0.5 (0.07 - 3.71) | ||
| Yes | 2 (28.6) | 5 (71.4) | ||
| No (reference) | 37 (50) | 37 (50) | ||
| APACHE II score | 0.4 | 0.9 (0.1 - 1.5) | ||
| 0 - 15 | 13 (40.6) | 19 (59.4) | 0.8 (0.41 - 1.73) | |
| 16 - 19 | 12 (57.1) | 9 (42.9) | ||
| 20 - 30 (reference) | 14 (50) | 14 (50) | 0.6 (0.3 - 2.43) | |
| Number of EVD | 0.3 | |||
| One time | 35 (89.7) | 38 (90.5) | 0.8 (0.3 - 4.2) | |
| More than one time (reference) | 4 (10.3) | 4 (9.5) | ||
| Time of EVDs, d | 7.34 ± 4.68 | 4.95 ± 3.86 | 0.09 | 1.2 (0.4 - 3.6) |
| > 6 | 15 (62.5) | 9 (37.5) | ||
| ≤ 6 (reference) | 23 (41.1) | 33 (58.9) | ||
| Type of airway | 0.4 | |||
| Intubation | 34 (50) | 34 (50) | 1.3 (0.6 - 2.5) | |
| Awaked and spontaneous (reference) | 5 (138.5) | 8 (61.5) | ||
| Duration of surgery, h | 4.22 ± 1.20 | 4.12 ± 2.1 | 0.2 | 1.3 (0.7 - 1.86) |
| CSF lactate ≥ 36 | 0.9 | 1.5 (0.9 - 3.2) | ||
| Yes | 21 (48.8) | 22 (51.2) | ||
| No | 18 (47.4) | 20 (52.6) | ||
| Mechanical ventilation (MV) | 0.3 | 1.6 (0.9 - 2.5) | ||
| Yes | 34 (50.7) | 33 (49.3) | ||
| No (reference) | 5 (35.7) | 9 (64.3) | ||
| Length of time MV, d | 12.87 ± 12.18 | 8.57 ± 10.40 | 0.04b | 2.3 (1.4 - 3.56) |
| > 6 | 23 (60.5) | 15 (39.5) | ||
| ≤ 6 (reference) | 16 (37.2) | 27 (62.8) | ||
| Use of antibiotic prophylaxis | 0.04b | |||
| Ceftazidim + vancomycin | 17 (39.5) | 26 (60.5) | 0.3 (0.08 - 0.78) | |
| Vancomycin + meropenem ( ± other antibiotics) (reference) | 22 (57.9) | 16 (42.1) | ||
| Length of tunneling, cm | 0.01b | 2.5 (1.87 - 4.76) | ||
| > 5 | 9 (69.2) | 4 (30.8) | ||
| ≤ 5 (reference) | 36 (44.1) | 38 (55.9) | ||
| Length of time antibiotic prophylaxis, d | 15.69 ± 3.71 | 13.68 ± 8.37 | 0.5 | 1.2 (0.76 - 8.23) |
| > 9 | 21 (55.3) | 17 (44.7) | ||
| ≤ 9 (reference) | 18 (41.9) | 25 (58.1) | ||
| Length of time ICU stay, d | 13.87 ± 3.67 | 10.55 ± 2.27 | 0.1 | 1.04 (0.6 - 1.98) |
| > 10 | 22 (56.4) | 17 (43.6) | ||
| ≤ 10 (reference) | 17 (40.5) | 25 (59.5) | ||
| Length of time hospital stay, d | 22.33 ± 9.61 | 21.1 ± 12.22 | 0.1 | 1.8 (0.8 - 3.21) |
| > 14 | 23 (57.5) | 17 (42.5) | ||
| ≤ 14 | 16 (39) | 25 (61) | ||
Abbreviations: CI, confidence interval; OR, odds ratio.
aValues are expressed as No. (%) or mean ± SD.
bIndicates statistical significance.
| Variables | OR (95% CI) | P-Value |
|---|---|---|
| Time of EVDs, d | 0.08 | |
| > 6 | 1.1 (0.4 - 3.6) | |
| ≤ 6 (reference) | ||
| Length of time MV, d | 0.04* | |
| > 6 | 2.5 (1.6 - 3.56) | |
| ≤ 6 (reference) | ||
| Use of antibiotic prophylaxis | 0.04* | |
| Ceftazidim + vancomycin | 0.4 (0.08 - 0.84) | |
| Vancomycin + meropenem (± other antibiotics) (reference) | ||
| Length of tunneling | 0.02* | |
| > 5 | 1.98 (1.87 - 4.76) | |
| ≤ 5 (reference) |
aThe adjusted odds ratio in multiple logistic regression analysis to predict EVDs infection. Statistical significance is indicated with a star (*).
5. Discussion
Although in the present study only two (5.1%) of cultures were positive with gram-positive or gram-negative micro-organisms, the prevalence of EVDs infections was 48.1%, which is more than the rate reported by several studies that used criteria similar to the present study (7-9). There was no difference between the patients concerning the variable of gender. Although There was no difference between infection rate and the number of catheter placement in neurosurgery patients …, but having a catheter was associated with an increased risk of EVDs infection (Figure 1). A study performed by Camacho EF mentioned the length of catheterization as an important risk factor for EVDs infection (OR: 10.3, 95% CI: 4 - 26, P = 0.04) (10). The aforementioned study also reported that the median length of hospitalization was higher in the EVDs infection group (OR: 42, 95% CI: 10 - 111, P = 0.007) (8). In the present study, there was no difference between the duration of surgery and catheter infection; however, Lu et al. (11) reported that the operation time in the infected group was longer than the non-infection group (4.66 ± 2.00 vs. 3.57 ± 1.33; t = 6.159, P = 0.014). In the same study, the logistic regression analysis confirmed that a preoperative ventricular-peritonea shunt, operative duration, blood transfusion during surgery, multiple CSF sampling, and EVDs duration were correlated with postoperative EVD-related infection (P < 0.05) (11). According to the findings, the length of mechanical ventilation was significantly higher in the EVDs infection group. However, there are studies that reported other results. It can be argued that patients who received mechanical ventilation for a long time often do not have a good physical condition, so they are at increased risk of catheter infection. In the current survey, the length of tunneling (> 5 cm) was associated with a higher incidence of EVDs infection. A study performed at the University of Florida on 100 patients with catheter < 5 cm reported an infection rate of zero (12, 13). Kim et al. (14) found an association between ventriculostomy-related catheter tract hemorrhage (VCTH) and Ventriculostomy-related infection (VRI). Although we did not use antibiotic-coated EVDs in the ICU of Loghman Hakim Hospital, but the efficacy of antibiotic-coated EVD (AC-EVD) in reducing the occurrence of EVDs was evaluated and confirmed (15, 16). Lang et al. (17) demonstrated a significant decline in ventriculostomy-associated CSF infection rate following the implementation of antibiotic-impregnated EVD catheters (0.9% vs 6%, P = 0.00128). Verberk et al. (18) reported that antibiotic-impregnated EVDs were not associated with a significant decline in the risk of VRIs in routine care. Also, it did not affect bacterial etiology. In this study, ceftazidim + vancomycin prophylaxis was associated with a lower risk of infection than vanco + meropenem (± other antibiotics) (39.5% vs. 57.9%). In another survey performed by Camacho et al. (10), no generation of cephalosporins was superior to other generations. Tsioutis et al. (19) reported that Gram-negative bacteria (GNB) predominated (57.9%) in the EVDs infection, followed by Gram-positive (36.8%) and fungi (5.3%). The current study had limitations, including not considering culture results when diagnosing the infection, because of the high prevalence of false-negative reports. Hence, the authors recommend further studies with higher accurate laboratory facilities and selecting participants from various healthcare facilities. We hope this study, despite its limitation, can provide useful information for considering risk factors for EVD infection.