1. Introduction
Ultrasound-guided nerve blocks have enhanced our abilities to selectively and effectively suppress certain nerves to accomplish specific goals beyond the regional anesthesia targets, including diagnostic blocks (1). It may consist of the blockade of a localized seizure muscle movement without affecting the seizure threshold or level of consciousness (2).
We employ the majority of the peripheral nerve blocks (PNB) for acute pain management. Sometimes, we use them for the diagnosis or treatment of chronic pain. There are other indications for PNB like enhancing tissue perfusion (3) and reliving trismus for safer anesthesia induction and intubation (4).
This case report presents a unique application of continuous PNB (CPNB) to control the localized seizure muscular movement, without affecting the seizure threshold or level of the consciousness.
2. Case Presentation
A 27 years old man with high-frequency partial seizures in facial muscles who was a candidate for seizure focus ablation admitted in seizure department for seizure mapping. Seizure mapping was impossible due to forceful facial muscle contractions during convulsions. The patient was referred by his neurologist to suppress chewing muscles at least for 12 - 24 hours, without affecting other cognitive, motor, or protective reflex functions. His body mass index (BMI) was 27.6 kg/m2. He was otherwise healthy, and there was no prominent point to suspect coagulative or infectious problems in the history or physical exams.
Informed consent was obtained from the patient. He was then scheduled for bilateral ultrasound-guided CPNBs of the mandibular nerves.
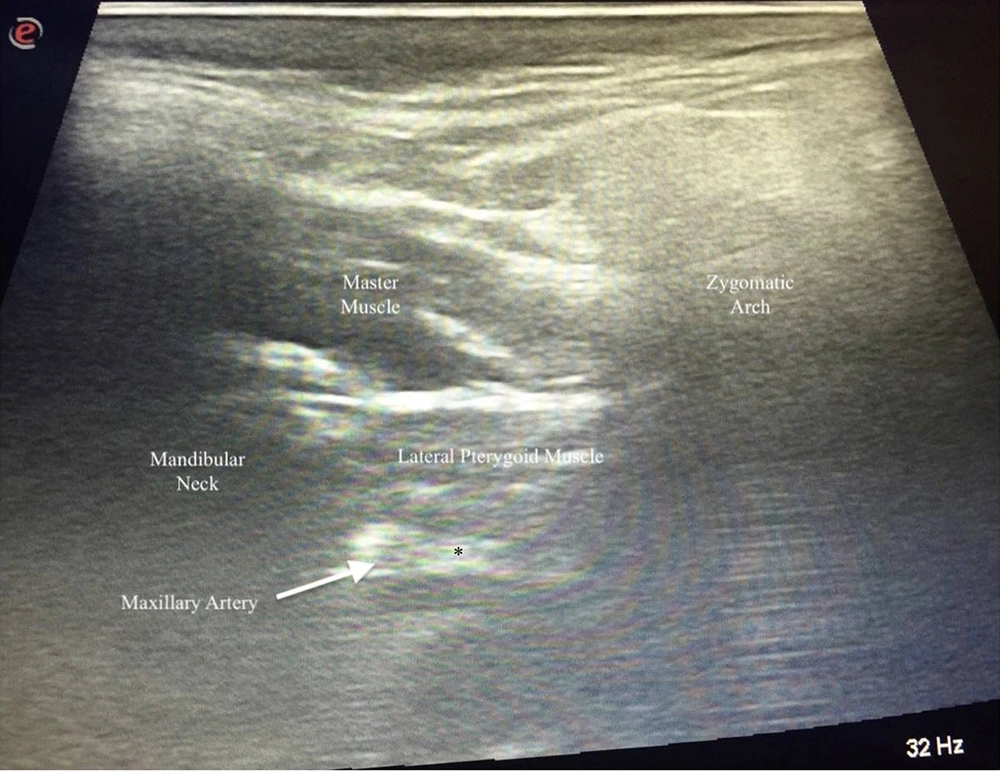
Routine monitoring and secure intravenous line were established. The patient was located in the lateral decubitus position. A linear probe (Medison, linear probe, 5 - 13 MHz) was placed on the infra-zygomatic fossa, just superior to the supra-mandibular notch, and in a transverse plane parallel to the interpupillary line. First, the maxillary artery was detected deep to the masseter muscle and between the lateral and medial pterygoid muscles, in a depth of approximately 3 cm (Figure 1). After prep and drape, the skin and subcutaneous tissue were infiltrated by 1 mL lidocaine 1% plus 1/200,000 epinephrine. We inserted an 18-gauge Tuohy needle in an out-of-plane approach with 5 degrees tilt into the fossa. We advanced the tip of the needle toward the mandibular nerve. Subsequently, we injected 1.5 mL lidocaine 1% plus 1/200,000 epinephrine, and then we inserted a 22-G catheter. We injected 2 mL of normal saline for fluid dissection to ensure the right position of the tip of the catheter. Then, we secured the catheter by fixing it to the skin. The same process was performed on the other side.
The patient was returned to the seizure department with the order of bupivacaine 0.25% 2 mL every 2 hours via each catheter and repeated as needed, to provide optimal facial paresthesia and biting force, based on neurologist decision. Four doses of local anesthetic were enough to provide a complete block of muscular twitch during convulsions for 24 hours. Seizure mapping was successfully performed. The catheter was removed 24 hours later. There was no remained paresthesia, pain, or motor deficit in the following days.
3. Discussion
This case report presented a unique application of CPNB to suppress the localized seizure muscular movement, without affecting the seizure threshold or level of the consciousness. Trigeminal ganglion (TG) has been blocked in different ways. TG has been blindly blocked through foramen ovale and in order to reduce the complications and to increase the accuracy of the block, the fluoroscopy-guided techniques were employed. Mandibular nerve, the third branch of the TG, can be selectively blocked by fluoroscopy or ultrasound guidance as well (5-7). Ultrasound guidance provides excellent visualization of these bony and soft tissue structures. Moreover, the artery and vein, which accompany the nerves, can easily be identified and avoided by the US-guided techniques (5, 8-12). This block was used for reliving spasm during anesthesia and intubation (4), treatment of trigeminal neuralgia (6), and pain management in the intra- or post-operative phases (1, 11).
This is the first report of ultrasound-guided catheter-based mandibular nerve block and also its unique application for control of chewing muscular tone.
Four muscles are mainly implicated in the mastication, including the masseter, temporalis, medial pterygoid, and lateral pterygoid muscles (13). All these muscles are innervated by the third branch of the trigeminal nerve due to their common embryological source, the first pharyngeal arch. This branch of the trigeminal nerve is the only one that has both sensory and motor fibers (13). We could demonstrate that an acceptable block of facial and chewing muscles would be achieved by suppressing the mandibular nerve, which can effectively facilitate the seizure focus mapping and ablation.
3.1. Conclusions
We can selectively suppress the contractures of certain muscles in partial seizures by a continuous block of the responsible nerve. This blockade can facilitate seizure focus mapping and ablation.