1. Background
Approach to lower-thoracic spine for discectomy remains controversial. Traditionally, surgeons prefer to approach lower thoracic discs through anterior or transthoracic (TT) approach, irrespective of the disc location or characteristics (1, 2). This is pertaining to unrestricted access of TT approach to entire disc space. Recently, surgeons have been selective considering herniated disc location and its characteristics as decisive factors for approach to lower thoracic discs. Central disc herniations and calcified discs are anteriorly approached mostly by TT approach. However, lateral disc protrusions are postero-laterally approached using transpedicular (TP) approach (2-4).
This study aimed to compare the primary and secondary outcomes of TT and TP approaches in patients with neurological deficiency, mainly foot drop. We also reviewed the recent trends in approaches to lower-thoracic discs and identifying the optimal approach.
Neurological manifestation of herniated disc is the most common cause for patients seeking surgical intervention (5). Studies have shown that neurological involvement fairly affects the prognosis of surgery. Patients with radiculopathy have better outcome than patients with complete paresis in the lower limb (2, 6). Moreover, duration of palsy, preoperative muscle strength, and age were found to have a significant influence on prognosis (7). Accordingly, in the current study we included patients with neurological manifestation of lower thoracic disc herniation, mainly foot drop, due to weakness in tibialis anterior muscle.
2. Methods
2.1. Patients
In this retrospective study, we collected the data of patients operated between 2005 and 2016 prospectively. All surgeries were performed at a single center by the same surgeon. All patients signed informed surgical consent prior to intervention. Inclusion criteria were patients who underwent one or two levels of lower-thoracic discectomy using either TP or TT approaches. Patients with neurological manifestation, such as unilateral or bilateral foot drop, those with incomplete data entry, accompanying cervical, upper thoracic, or lumbar disc herniation, and patients with no neurological involvement were excluded. The demographic information, preoperative examination notes, surgical data, and postoperative follow-up results were recovered from the hospital archive system (Table 1).
| Approach | P-Value | ||
|---|---|---|---|
| Transpedicular | Transthoracic | ||
| Sex | 0.999 | ||
| F | 2 | 2 | |
| M | 5 | 3 | |
| Level of disc | 0.999 | ||
| T11-T12 | 2 | 2 | |
| T12-L1 | 5 | 3 | |
| Fusion level | 0.003 | ||
| T11-L1 | 2 | 2 | |
| T11-L2 | 0 | 0 | |
| T12-L1 | 0 | 3 | |
| T12-L2 | 5 | 0 | |
| Foot drop | 0.999 | ||
| Bilateral | 3 | 2 | |
| Unilateral | 4 | 3 | |
| Hyper patella reflex | 0.491 | ||
| Bilateral | 5 | 4 | |
| Unilateral | 2 | 0 | |
| Urinary incontinence | 0.999 | ||
| No | 1 | 1 | |
| Partial | 6 | 4 | |
| Erectile dysfunction | 0.999 | ||
| Complete | 3 | 2 | |
| Partial | 4 | 3 | |
| Neurological recovery (weeks) | 0.428 | ||
| Complete | 6 | 4 | |
| Partial | 1 | 1 | |
| CSF leak | 0.364 | ||
| No | 7 | 4 | |
| Yes | 0 | 1 | |
| pulmonary complications | 0.109 | ||
| No | 7 | 3 | |
| Yes | 0 | 2 | |
| Wound complications | 0.999 | ||
| No | 6 | 3 | |
| Yes | 1 | 2 | |
| Infection | - | ||
| No | 7 | 5 | |
| Yes | 0 | 0 | |
| Intercostal neuralgia | 0.109 | ||
| No | 7 | 3 | |
| Yes | 0 | 2 | |
| Readmission within 30 days | 0.364 | ||
| No | 7 | 4 | |
| Yes | 0 | 1 | |
| Mortality within 90 days | - | ||
| No | 7 | 5 | |
| Yes | 0 | 0 | |
2.2. Outcome & Comparison
Primary outcome measures were postoperative neurological recovery at 6, 12, and 24 weeks, operating time, blood loss, time to mobilization, and duration of hospital stay. Secondary outcomes were adverse events related to surgical approach such as pulmonary complications, requisite of postoperative intensive care unit (ICU) monitoring, intercostal neuralgia, wound complications, infection, readmission within 30 days, cerebral spinal fluid (CSF) leak, and 90-day mortality rate. Primary and secondary outcomes of TP and TT approaches were compared for lower thoracic-discectomy in patients with preoperative neurological manifestations.
Preoperatively, electromagnetic study (EMG-NCV) was performed to verify the source of neurological deficiency. Neurological recovery was measured by comparing preoperative and postoperative muscle grading using medical research council manual muscle testing scale (MMT). Surgical notes were reviewed for operating time and intraoperative blood loss. Postoperative recovery notes were scanned for mobilization time, duration of stay, complications, and mortality. Intraoperative blood loss was calculated by blood in swabs (weight of soaked swabs – weight of dry swabs) + fluid in suction bottle – irrigation fluid. For statistical analysis, using statistical package for the social sciences (SPSS) software version 20 for windows, the primary and secondary outcomes of TT approach were compared with those of TP approach. Symmetrically distributed numerical variables were summarized with means and standard deviations, while other variables were summarized with medians and ranges. Data from both groups were compared using 2-tailed t test, and a P-value less than 0.05 (P < 0.05) was considered significant.
2.3. Surgical Techniques
The choice of approach was based on a general practice trend, not medical comorbidities, location or level of lesion, or degree of cord compression. At the beginning of the study period, we approached all lower thoracic disc using TT technique. However, as the trends shifted towards more selective approach; we preferred TP technique. Thus, the decision to choose one approach over the other was a temporal trend rather than a clinical decision.
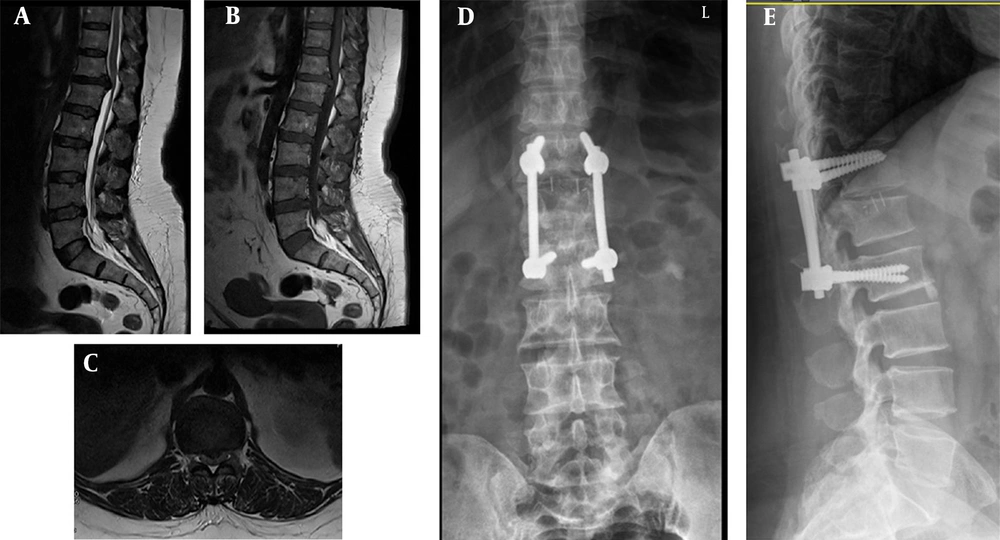
TP approach was carried out through a midline posterior incision after bilateral exposure laminectomy, and pediculectomy of the vertebrae below were performed. The disc was approached with care without stringent manipulation of the cord; herniated disc was debrided, and reverse curette technique was applied to remove the bulk disc between vertebral bodies. Intervertebral cage was inserted to prevent collapse. Posterior fusion was attained using pedicle screw and rod with one level above and below, skipping the pediculectomy vertebrae (Figure 1).
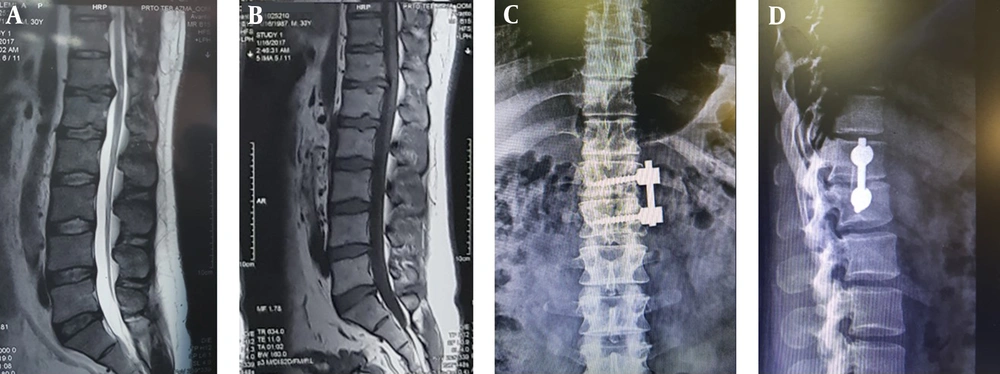
TT approach was performed by thoracotomy at intended level and gaining access to anterio-lateral disc space through pleural cavity. Disc was debrided with care not injuring underlying dura. Excised rib was used as intervertebral autograft for attaining better fusion and preventing collapse. Single-level anterio-lateral fusion was achieved with pedicular screw and rod (Figure 2).
3. Results
using the international classification of diseases (ICD) codes, searching the database identified 34 lower thoracic discectomies. Preoperative notes revealed 12 patients with at least foot drop. TP approach was used in seven patients and TT in five patients.
3.1. Primary Outcomes
Six patients in TP group and four in TT attained complete neurological recovery after a mean of 10.2 and 7.6 weeks, respectively (MMT 5/5). Partial recovery was observed in one patient from each group by the end of 24th week (MMT 2 - 3/5). The mean operative time of TT and TP approaches was 173.33 and 146.63 minutes, respectively, which was 30% more in TT approach (P-value = 0.02). The mean blood loss in TT and TP approaches was 716.67 and 293.75 mL, respectively, which was 150% more in TT approach (P-value = 0.01). While patients in TP group mobilized after 1 - 2 days, mobilization in TT group was delayed to 3 - 5 days postoperatively. Patients in TP group had less hospital stay (mean: 4 days) compared to patients in TT group (mean: 7 days) (P-value = 0.01) (Table 2).
| Variable | Mean | Std. Deviation | P-Value |
|---|---|---|---|
| Age | 0.55 | ||
| TP | 36.50 | 8.46 | |
| TT | 39.67 | 3.05 | |
| Symptom duration (mo) | 0.90 | ||
| TP | 6.38 | 3.46 | |
| TT | 6.67 | 3.05 | |
| Time to recovery of foot drop (weeks) | 0.50 | ||
| TP | 10.25 | 6.08 | |
| TT | 7.67 | 2.51 | |
| Operative time (min) | 0.02 | ||
| TP | 146.63 | 21.93 | |
| TT | 173.33 | 10.408 | |
| Blood loss (mL) | 0.01 | ||
| TP | 293.75 | 149.08 | |
| TT | 716.67 | 104.08 | |
| Mobilization (days) | 0.01 | ||
| TP | 2.00 | 0.92 | |
| TT | 4.00 | 1.00 | |
| Hospital stay (days) | 0.01 | ||
| TP | 4.13 | 1.64 | |
| TT | 7.33 | 0.57 | |
| ICU stay (days) | 0.01 | ||
| TP | 0 | 0 | |
| TT | 3.33 | 0.57 |
3.2. Secondary Outcomes
All patients in TT group needed postoperative ICU admission (P-value = 0.01), with two of them developing pulmonary complications. Two patients in TT group developed postsurgical intercostal neuralgia for 4 - 5 months. One patient in TP group and two patients in TT group developed superficial wound infections, which was controlled with oral antibiotics. One patient in TT group had CSF leak due to iatrogenic damage to dura, which was repaired primarily. None of the patients had mortality within 90 days; however, one patient in TT group was reported to have readmission due to pneumonia within 30 days of discharge. Further details are shown in Tables 1 and 2.
4. Discussion
Surgical approach should be balanced between morbidity it creates and exposure it offers. In this study, we compared outcomes of two approaches (TT and TP) for lower-thoracic discectomy in patients with neurological manifestation, mainly foot drop. The existing literature favors TT approach over TP in lowering thoracic disc owing to better exposure and safe course for discectomy (2). However, TT approach is associated with higher morbidity rates, with some studies reporting up to 30% postoperative complications (8, 9).
In our study, 83% of patients achieved complete neurological recovery after 24 weeks, and one patient in each group had partial recovery. The mean recovery time in TT group was less than TP group; however, the difference was insignificant (P-value = 0.50). Literature shows that postsurgical neurological recovery is better in patients with lower thoracic compressions than lumbar radiculopathy (5, 10).
Standard laminectomy and posterior discectomy procedure is not performed in thoracic spine owing to myriad complications reported in earlier studies (11). Several authors were concerned about neural canal manipulation leading to postoperative neurological deterioration (12). Several alternative approaches were developed to circumvent such major complications, yet every approach has its own merits and demerits. However, the best surgical approach to thoracic disc, particularly in lower levels (thoraco-lumbar junction), still remains controversial.
Recent review on complication rates associated with approach is illustrated in Table 3. Among thoraco-lumbar approaches, posterior approach has been linked to fewer complication rates, explicitly postero-lateral TP approach being the lowest one. In the last decade, we observed an urge in spine surgeons to move towards minimal invasive techniques, including video assistance in wake of avoiding unnecessary soft tissue mutilation. However, reports on long-term outcome are scarce, and steep learning curve is being interpreted. One such approach is minimal invasive video-assisted thoracoscopic spinal surgery (VATS) pioneered by Mack et al. (13).
| Approach | Study | Complication Rate (%) |
|---|---|---|
| Laminectomy | Ridenour et al., 1993 (14) | 35 - 48 |
| Transpedicular | Arts and Bartels, 2014 (4) | 5 - 7 |
| Transthoracic | Lubelski et al., 2013 (8) | 30 - 39 |
| Costotransversectomy | McCormick et al., 2000 (12) | 10 - 15 |
| Lateral extracavitary | Lubelski et al., 2013 (8) | 15 - 17 |
| Transfacet | Stillerman et al., 1995 (15) | 9 - 11 |
| Mini-Transthoracic | Arts and Bartels, 2014 (4) | 22 - 28 |
| Mini-Lateral | Uribe et al., 2012 (16) | 11 - 18 |
There are several comparative studies on surgical approach to lower-thoracic discs (2, 4, 8). However, reports focused on an approach with neurological outcome are scarce. Therefore, we compared the outcomes of two approached to lower-thoracic discs in patients with neurological symptoms. We primarily focused on patients with foot drop caused by lower-thoracic disc herniations; all patients in our study had either unilateral or bilateral foot drop.
Exposure is the main defining factor for any given approach; technically, there is no exposure assessment tool that can measure or compare surgical exposures. TT approach has been reported to provide excellent exposure without stark manipulation of the spinal cord. Nonetheless, attaining extensive exposure at the expense of accompanying morbidity has to be justified. TT approach has been associated with higher rates of complications and morbidity (8).
The surgical treatment of patients in lower-thoracic disc herniations with neurological manifestation can be challenging and may be associated with varying risks. Therefore, these complex spinal procedures should be conducted in the presence of multi-disciplinary team with experienced spine surgeons. The treatment algorithm for the optimal surgical approach should include magnetic resonance imaging (MRI), computed tomography (CT) scan, and conventional radiography of the whole spine. Proper documentation is mandatory to avoid the pitfalls of wrong level surgery. Arts et al. recommended that in approaching lower-thoracic spine, central disc herniations and large calcified paracentral herniated discs should be treated with TT approach (4). They also preferred performing discectomy without any additional instrumentation and fusion. However, we performed instrumentation and fusion in all our patients with placement of bi-cortical screws and rod fixation (Figures 1 and 2); thereby, iatrogenic scoliosis can be prevented.
As the results of our study and some previous reports indicated, pulmonary complications such as pneumonia are common in TT approach. All patients in TT group required postsurgical ICU monitoring and had longer hospital stay, endangering patients to nosocomial infections and substantially increasing the cost of surgery. We did not undertake cost or expense analysis in this study, as acquiring exact cost related to approach might be challenging, specially in state-owned hospitals. However, cost analysis comparing approaches in thoracic spine would be a possible study for further research.
Our results indicated that TP approach is more cost-effective than TT approach given the operative time, requirement for blood, ICU, and hospital stay. Patients in TP group had a decreased operative time and blood loss, mobilized earlier, did not require ICU admission, and had a decreased hospital stay. To attain better exposure in TP approach, a slight manipulation of cord might be required; however, if minimal manipulation is kept, neurological consequences can be avoided. This is consistent with the studies indicating that postsurgical neurological deterioration is a rare complication in this technique (1%) (12, 17).
4.1. Limitations
This is a prospective study. Any errors on recording database would reflect on outcomes. We tried to minimize this error by reviewing patient data with the surgeon who operated and residents who examined the patients. Another major limitation of our study is its small sample size, which could not represent a randomized control trial. Therefore, we included a literature review comparing our results with previously published reports to achieve a cohort prospective. Moreover, since thoracic discectomy cases with neurological manifestation (foot drop) are rare, we encountered 12 patients in last 10 years.
4.2. Conclusions
Significant neurological recovery can be expected in patients with foot drop due lower-thoracic disc herniation, irrespective of approach and symptom duration. No outcome study can substitute surgeons's experience while deciding on approach to surgery. However, the operating surgeon has to consider various other factors such as patient comorbidities, cost analysis, risk factors, level, and characteristics of the disc. TT approach offers an excellent exposure for discs in lower-thoracic levels; nevertheless, it is associated with increased morbidity and higher complication rates. On the other hand, TP approach offers ample exposure with reduced operative time and blood loss, as well as early mobilization and discharge.