1. Background
Non-specific chronic low back pain (NS-CLBP) is a complicated biopsychosocial problem with various manifestations (1). Neuroimaging research had shown that chronic musculoskeletal pain such as NS-CLBP could be the cause of structural and functional cortical reorganization (2). Besides, it was shown that the activity of the lumbopelvic muscles had altered with changes in the motor cortical representation of the muscles in patients with NS-CLBP (3), which, in turn, leads to chronic pain. It thus attracted some researchers to study the potential role of abnormal processes of the cortical central nervous system in patients with NS-CLBP (4, 5). Accordingly, various studies have concluded that altered patterns of muscle activation, such as flexion relaxation phenomena in the trunk forward flexion movement, may be caused by pain and avoidance behaviors (pain-related fear) (6, 7). Trunk forward flexion movement contributes to all physical and functional daily living activities and can be linked to the fear of pain and expected pain as an effective agent to the changes in the representation of the cortex (8, 9). Intermuscular coherence (IMC) is a process in which coherence analysis between surface electromyography signals from the synergistic muscles. IMC was suggested as a useful tool for motor control studies, and it could be have a better perception of the CNS strategies procedure (10), and it is capable of quantifying the pair of muscle common oscillatory drive (11). Besides, it might reveal the presence of neural presynaptic shared inputs from the motor cortex (12), and the contributions of common spinal interneurons (13). By studying the peripheral information only, IMC aims to identify these neural mechanisms. Moreover, it was shown that at specific frequencies, including delta, alpha, beta, and gamma as "0 - 5HZ", "5 - 15 HZ", "15 - 30 HZ", and "30- 60HZ", respectively, the coherence had been mediated via specific pathways. Thus, analysis of coherence detected at different specific frequencies could supply considerable information on the nervous system function for controlling the muscle's activity during different tasks (14). Accordingly, Beta band Intermuscular Coherence (Bb-IMC) was supposed to form hugely from the primary motor cortex and could shape a potential biomarker of the function of the corticospinal tract. It was also supposed to offer the common corticospinal drive to the muscles from the primary motor cortex. Also, the studies suggested that Bb-IMC could be considered an appropriate tool for the assessment of dynamic tasks (14). In other words, the studies suggested that other bands reflect the multiple muscles synchronizations during postural tasks such as slow movements and isometric contraction (15), and are linked to common inputs from the subcortical structures (16). Besides, the studies used the Bb-IMC as a tool to investigate the potential effects on the common neural drive of spinal cord injury to adjust the antagonist and agonist muscle pair's activity (17). Also, another study had investigated the possible mechanisms causing the abnormal motor overflow in spasticity of stroke patients (18). Also, some studies suggested that some new interventions reinforced the control of sensorimotor in elderly subjects by using Bb-IMC (19). Based on our previous studies (in press), a moderate to a high level of reliability and agreement for Bb-IMC in patients with NS-CLBP and healthy subjects were shown during four phases of standing, flexion, relaxation, and extension in flexion-extension task (F-ET). Also, we showed that the Bb-IMC could clinically be used for NS-CLBP assessment in F-ET due to feasibility, easy use, and high safety. Scientific evidence of the last two decades had strongly supported the clinical effectiveness of manual therapy techniques for NS-CLBP (20, 21). To the best of our knowledge, most of the manual therapy studies like spinal manipulation technique (SMT) and muscle energy technique (MET) had focused only on pain assessment and disability and just dealt with the mechanical and physiological effects of SMT. In other words, the probable cortical effects and the effectiveness of these techniques over the primary motor cortex and corticospinal tract function were overlooked.
2. Objectives
The current study aimed to compare two manual therapy technique's effects (SMT and MET) on corticospinal tract function during four phases of standing, flexion, relaxation, and extension in flexion-extension task (F-ET) in the NS-CLBP using pair-wise coherence of Bb-IMC.
3. Methods
3.1. Participants
Twenty-four men (20 - 40 years) with NS-CLBP and 20 healthy subjects voluntarily participated in this study. They were among the people who were referred to the Physiotherapy clinic and Biomechanics Laboratory, School of Rehabilitation, Tehran University. A patient NS-CLBP was included if he met the following inclusion criteria: patients with continuous or recurrent symptoms for three months or more without referral or radicular pain to the lower extremities, pain according to the Numerical Rating Scale was 30 out of 100 and the disability was eight out of 50 of the questionnaire of Oswestry (22), yellow flags dominant (i.e., emotions and beliefs), red flags absence (such as inflammatory disease or cauda equine syndrome), pain or symptom excitation in loading on the one side and more specific activities and postures such as (desktop-workers, car driver), whereas the functional improvement and pain reduction with dynamic or low load activities, pain/complaints increase(s) during the day, positive prone instability test (23) and specific dysfunction segments (L2-L3-L4 segments), no sign of radicular pain or neurological signs, no sign and symptoms of severe musculoskeletal deformity, no restriction in trunk flexion task in the standing position, no previous treatment or spinal manipulation within the last six months. Patients were excluded if they were not interested to carry on the study or had an increase in the symptoms, which prevented the completion of the study (24). Moreover, healthy subjects were included in this study if they had not received previous exercises of postural training and they had no LBP history (23). Furthermore, an informed consent form was signed by all participants according to the Ethics Committee of Tehran University with the Ethics code IR.TUMS.VCR.REC.1398.675, and this study was approved by Tehran University of Clinical Trials with the number IRCT20090301001722N22.
By the project manager, 24 slips of paper were allocated, half of them were marked for SMT letters and the other half for MET letters. Then they were randomly placed in sealed envelopes so that each slip of paper was in an envelope then each envelope was numbered 1 to 24. Then, they were sent to the clinical who did the testing sessions for the patients. Sealed envelopes were opened by the laboratory director, who was not a member of the study's team, to disclose the group allocation of the subjects.
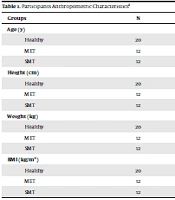
The first group was the spinal manipulation technique (SMT) and the second group was the muscle energy technique (MET). Both patient and healthy groups were matched according to the demographic characteristic (Table 1).
| Groups | N | Mean | Std. Deviation | P-Value |
|---|---|---|---|---|
| Age (y) | 0.564 | |||
| Healthy | 20 | 34.7500 | 10.04136 | |
| MET | 12 | 41.5833 | 9.13991 | |
| SMT | 12 | 37.2500 | 10.01930 | |
| Height (cm) | 0.482 | |||
| Healthy | 20 | 174.8500 | 6.38481 | |
| MET | 12 | 178.4167 | 9.98598 | |
| SMT | 12 | 176.0833 | 5.71216 | |
| Weight (kg) | 0.507 | |||
| Healthy | 20 | 79.6200 | 8.12686 | |
| MET | 12 | 85.6667 | 13.42544 | |
| SMT | 12 | 84.5000 | 9.35900 | |
| BMI (kg/m2) | 0.476 | |||
| Healthy | 20 | 26.0490 | 2.39089 | |
| MET | 12 | 26.8375 | 3.51591 | |
| SMT | 12 | 27.2333 | 2.51864 |
Abbreviation: BMI, body mass index.
3.2. Measures/Instruments
The skin's surface of the muscles was shaved and cleaned with alcohol wipes. All sEMG signal recordings were made using the DataLOG, Biometrics Ltd England. Then, the bipolar active electrodes with a recording diameter of 10 mm and a 20 mm fixed center to center interelectrode distance were mounted on the relevant muscle, built-in differential amplifier, and the ground electrodes were located on the right wrist. The electrode positions and orientations were chosen according to EMG sensor locations defined in SENIAM guidelines The skin's surface of the muscles was shaved. The DataLOG, Biometrics Ltd England was used for sEMG signal recordings. SENIAM guidelines were used to define the electrode positions (24). Then, the bipolar active electrodes with a recording diameter of 10 mm were mounted on the relevant muscle, and the ground electrodes were located on the right wrist. The sEMG signal recordings was recorded from the the following muscles: right lumbar erector spinal "M1", left lumbar erector spinal "M2", right gluteus maximus muscle "M3", left gluteus maximus muscle "M4", right hamstring muscle "M5" and left hamstring muscle "M6". The M1, M4, and M6 muscles were considered A muscle cross. Moreover, M2, M3, and M5 muscles were named as B muscle cross.
3.3. Procedure
Subjects were familiarized with the procedure before the start of the test to reduce stress and fear of testing. Inside a square marked on the floor, all subjects stood while the distance between their feet was equal to their pelvis width, and their hands were aligned with their body and parallel. (25) Also, a paper was on the experiment site to ensure a standardized foot placement for each trial. There was a visual target placed at 3-meter distance, and their eyes were focused on it. After that, subjects were asked by verbal commands to perform three trials of F-ET while the sEMGs were recorded; each trial included recording data for 20 seconds (i.e., 5 seconds at standing phase, 5 seconds during flexion phase, 5 seconds at relaxation phase, 5 seconds during extension phase). A metronome was used to simultaneously monitor the consequences of all the above-mentioned phases with sEMGs recordings as an auditory signal (beep) every second during the whole task. To reduce the probability of discomfort, fatigue, and back injury, they were allowed to rest for two minutes between the trials (26, 27). This procedure was performed pre- and post-intervention for both patient groups (SMT and MET) and once for the healthy group.
3.4. Intervention
Patients of the current study were assigned to the flexed, rotated, and side bent (FRS) and extended, rotated and side bent (ERS) dysfunction groups based on the physical examinations (28). During which, each patient identified the specific dysfunction segment at the request of the physical therapist, which was certain by palpation of bone and muscle tissues such as tissue resistance increase, hypomobility presence, abnormal end-feel. In addition, the Mitchell test was performed to verify vertebral mobility and positioning (28). The manual intervention techniques were applied for patients according to randomly selected groups. An experienced physical therapist that had 10 years of clinical experience in treating patients with LBP and also had received formal training in manual therapies performed the interventions as described by Greenman (29). Some parameters were regarded in terms of the duration of treatment (about 10-15 min of contact time with the clinicians) for all intervention groups.
3.5. Beta-band Intermuscular Pair-Wise Coherence Analysis
The pair-wise coherence (PWC) was measured to highlight the coherence contributions that were common to all synergist muscles or unique to each pair of muscles, (30) across each of two muscle groups i.e., A muscle cross: right lumbar erector spinal " M1", left gluteus maximus muscle " M4", left hamstring muscle " M6" and B muscle cross: left lumbar erector spinal " M2", right gluteus maximus muscle " M3", right hamstring muscle " M5". To discover the coupling of the common neural between each of two muscle groups (i.e., A and B muscle cross). Besides, pairwise coherence analysis was performed to estimate the coherence contribution between two muscles. The following formulation of standard coherence was the basis of this analysis (31):
Where the f was the frequency and Cxy was the coherence between sEMG signals x and y. Pyy and Pxx denoted auto spectra for signals y and x, while Pxy stood for signal x and y cross-spectrum. Following the procedure, xDC (t) time series was used to calculate the coherence of all phases of F-ET. In this case, on 500 ms portions window through Hanning function and with a 50% overlap via Welch's method, the cross-spectral and the auto spectral were calculated. Coherence was defined as the frequency domain of Pearson's correlation coefficient extension and distinct the degree of linear correlation between the signals at each frequency on a scale that ranges from 0 to 1, where 0 represented no correlation and 1 represented ideal correlation and (32). Before the calculation of EMG-EMG coherence, the raw EMG signal was removed, or ejectedto remove the offset. When Intramuscular coherence overrides a confidence limit (CL) with a probability of 95%, it was featured at a specific frequency to be significantly larger than zero.
CL was determined as:
where α equaled the desired level of significance (29).
The coherence spectrum inverse Fourier transform was defined as the function of cumulate density. The inverse Fourier transform was calculated, as a time-domain measure of association between signals sEMG, for all muscle groups and every phase of F-ET, the function of cumulate density and coherence spectra were calculated, and the result was a set of 24 coherence spectra per subject. sEMG signals were focused to create a series of longer single times, with the goal of increasing the coherence estimations reliability, for each participant from all three trials. In the following steps, the spectra for a mentioned muscle pair were averaged in all participants within a group to provide a visual representation of the coherence dependence on frequency. According to the results, coherence values were calculated from 0 to 350 Hz. The analysis of frequency spectrum for each phase of F-ET tasks measured using MATLAB software 7.11 and spectrums of 15–30 Hz moved to coherence software too. So, we could assume the mean coherence distribution in a specific frequency band across the participants and provide a group summary.
3.6. Statistical Analysis
The normal distribution was for weight, age, height, and body mass index (BMI) and all outcome measurements (Pair-wise coherence) in three groups (P > 0.05). Considering the alpha level at 0.05 as significant statistically for analyses (P > 0.05). For all analyzes, the SPSS Statistics version 25 was used. Multivariate analysis of variance (MANOVA) test was used to compare the differences between the three groups before interventions in A and B muscle cross and four phases of F-ET. Besides, MANOVA test was also used to compare the SMT and MET before and after interventions in A and B muscle cross and at different phases in F-ET.
4. Results
Regarding basic anthropometric characteristics (i.e., age, height, weight, BMI), there were no significant differences between the groups (P >0.05) (Table 1). In this study, pair-wise coherence (PWC) was calculated, and then we considered the mean pair-wise coherence for the A muscle cross (M1, M4, and M6) and B muscle cross (M2, M3, and M5) for F-ET phases using Bb-IMC in healthy and for intervention groups (SMT and MET) before and after the interventions. The investigation of pair-wise coherence in three groups before interventions in A and B muscle cross in the four phases of F-ET are shown in Tables 2 and 3.
| Phases | 1 - 4 | 1 - 6 | 4 - 6 | F | P-Value | Partial Eta Squared |
|---|---|---|---|---|---|---|
| Standing | 1.17 | 0.31 | 0.527 | |||
| Healthy | 0.906 ± 0.019 | 0.897 ± 0.0244 | 0.900 ± 0.030 | |||
| MET | 0.8970 ± 0.024 | 0.894 ± 0.047 | 0.905 ± 0.025 | |||
| SMT | 0.8918 ± 0.023 | 0.898 ± 0.022 | 0.895 ± 0.026 | |||
| Flexion | ||||||
| Healthy | 0.9144 ± 0.028 | 0.897 ± 0.029 | 0.890 ± 0.030 | |||
| MET | 0.8878 ± 0.021 | 0.887 ± 0.026 | 0.882 ± 0.022 | |||
| SMT | 0.8828 ± 0.021 | 0.891 ± 0.018 | 0.874 ± 0.030 | |||
| Relaxation | ||||||
| Healthy | 0.8996 ± 0.028 | 0.903 ± 0.026 | 0.903 ± 0.029 | |||
| MET | 0.8995 ± 0.029 | 0.901 ± 0.027 | 0.881 ± 0.025 | |||
| SMT | 0.8956 ± 0.017 | 0.901 ± 0.019 | 0.887 ± 0.030 | |||
| Extension | ||||||
| Healthy | 0.9012 ± 0.025 | 0.903 ± 0.024 | 0.915 ± 0.025 | |||
| MET | 0.9146 ± 0.027 | 0.905 ± 0.025 | 0.909 ± 0.022 | |||
| SMT | 0.8955 ± 0.022 | 0.895 ± 0.030 | 0.900 ± 0.027 |
| Phases | 2 - 3 | 2 - 5 | 3 - 5 | F | P-Value | Partial Eta Squared |
|---|---|---|---|---|---|---|
| Standing | 1.287 | 0.186 | 0.452 | |||
| Healthy | 0.896 ± 0.030 | 0.891 ± 0.031 | 0.885 ± 0.030 | |||
| MET | 0.897 ± 0.030 | 0.897 ± 0.024 | 0.892 ± 0.022 | |||
| SMT | 0.901 ± 0.020 | 0.895 ± 0.033 | 0.899 ± 0.021 | |||
| Flexion | ||||||
| Healthy | 0.895 ± 0.025 | 0.902 ± 0.024 | 0.890 ± 0.026 | |||
| MET | 0.887 ± 0.029 | 0.891 ± 0.027 | 0.898 ± 0.025 | |||
| SMT | 0.897 ± 0.027 | 0.892 ± 0.013 | 0.882 ± 0.021 | |||
| Relaxation | ||||||
| Healthy | 0.892 ± 0.025 | 0.890 ± 0.025 | 0.886 ± 0.019 | |||
| MET | 0.897 ± 0.028 | 0.909 ± 0.019 | 0.899 ± 0.025 | |||
| SMT | 0.898 ± 0.021 | 0.891 ± 0.017 | 0.896 ± 0.035 | |||
| Extension | ||||||
| Healthy | 0.896 ± 0.023 | 0.883 ± 0.027 | 0.893 ± 0.026 | |||
| MET | 0.888 ± 0.028 | 0.888 ± 0.035 | 0.894 ± 0.027 | |||
| SMT | 0.911 ± 0.022 | 0.907 ± 0.022 | 0.895 ± 0.016 |
Multivariate tests before interventions indicated there are no significant differences between the three groups and F-ET phases in pair-wise coherence of A muscle cross (M1, M4, and M6) and pair-wise coherence of B muscle cross (M2, M3, and M5). The investigation of pair-wise coherence between SMT and MET intervention groups before and after the interventions in A and B muscle cross in each phase of F-ET phases are shown in Tables 4 - 7. In standing phase of F-ET, there were no significant differences in the SMT and MET groups before and after the intervention in PWC of A muscle cross and B muscle cross (P < 0.05). We noticed that, in this phase, the SMT increased PWC in all pair muscle, whereas it increased in A muscle cross and decreased in B muscle cross in the MET group, and there were no significant differences in the MET group before and after the intervention in four phases of F-ET (Table 4).
| Standing Phase | SMT | MET | ||||
|---|---|---|---|---|---|---|
| Before | After | P-Value | Before | After | P-Value | |
| A muscles cross | ||||||
| PWC (M1-M4) | 0.89 ± 0.02 | 0.90 ± 0.01 | 0.12 | 0.897 ± 0.025 | 0.899 ± 0.031 | 0.374 |
| PWC (M1-M6) | 0.89 ± 0.02 | 0.90 ± 0.02 | 0.24 | 0.894 ± 0.047 | 0.898 ± 0.029 | 0.392 |
| PWC (M4-M6) | 0.895 ± 0.02 | 0.899 ± 0.01 | 0.30 | 0.906 ± 0.026 | 0.908 ± 0.028 | 0.374 |
| B muscles cross | ||||||
| PWC (M2-M3) | 0.89 ± 0.02 | 0.90 ± 0.03 | 0.22 | 0.897 ± 0.025 | 0.894 ± 0.033 | 0.401 |
| PWC (M2-M5) | 0.896 ± 0.03 | 0.898 ± 0.02 | 0.43 | 0.894 ± 0.047 | 0.892 ± 0.033 | 0.423 |
| PWC (M3-M5) | 0.894 ± 0.02 | 0.899 ± 0.01 | 0.22 | 0.906 ± 0.026 | 0.894 ± 0.024 | 0.113 |
With regard to the flexion phase, there were significant differences in the SMT group in all pair muscles as PWC (M1-M4), PWE (M1-M6), PWC (M4-M6) (P < 0.05), and PWC increased in A and B muscle cross in all muscle pairs. In the MET group, PWC increased in all muscle pairs, and there was a significant difference in the PWC (M4-M6) (P < 0.05, Table 5). Considering the relaxation phase, the SMT increased PWC in all muscle pairs, and it was significant in PWC (M2-M5). In the MET, it increased PWC in PWC (M1-M6) PWC (M4-M6), and PWC (M3-M5), and whereas had decreased in PWC (M1-M4), PWC (M2-M3), and PWC (M2-M5), and it was significantly different in PWC (M4-M6) (Table 6).
| Flexion Phase | SMT | MET | ||||
|---|---|---|---|---|---|---|
| Before | After | P-Value | Before | After | P-Value | |
| A muscles cross | ||||||
| PWC (M1-M4) | 0.883 ± 0.021 | 0.899 ± 0.014 | 0.041 | 0.888 ± 0.022 | 0.894 ± 0.033 | 0.281 |
| PWC (M1-M6) | 0.892 ± 0.018 | 0.905 ± 0.018 | 0.049 | 0.887 ± 0.027 | 0.901 ± 0.029 | 0.119 |
| PWC (M4-M6) | 0.875 ± 0.031 | 0.899 ± 0.020 | 0.011 | 0.882 ± 0.023 | 0.904 ± 0.029 | 0.028 |
| B muscles cross | ||||||
| PWC (M2-M3) | 0.897 ± 0.027 | 0.908 ± 0.030 | 0.205 | 0.888 ± 0.022 | 0.904 ± 0.022 | 0.051 |
| PWC (M2-M5) | 0.893 ± 0.014 | 0.894 ± 0.020 | 0.471 | 0.887 ± 0.027 | 0.897 ± 0.034 | 0.490 |
| PWC (M3-M5) | 0.882 ± 0.022 | 0.896 ± 0.028 | 0.087 | 0.882 ± 0.023 | 0.886 ± 0.027 | 0.220 |
| Relaxation Phase | SMT | MET | ||||
|---|---|---|---|---|---|---|
| Before | After | P-Value | Before | After | P-Value | |
| A muscles cross | ||||||
| PWC (M1-M4) | 0.896 ± 0.017 | 0.899 ± 0.023 | 0.333 | 0.900 ± 0.030 | 0.895 ± 0.040 | 0.369 |
| PWC (M1-M6) | 0.901 ± 0.020 | 0.905 ± 0.019 | 0.263 | 0.902 ± 0.027 | 0.903 ± 0.026 | 0.442 |
| PWC (M4-M6) | 0.887 ± 0.030 | 0.900 ± 0.019 | 0.089 | 0.882 ± 0.026 | 0.898 ± 0.022 | 0.017 |
| B muscles cross | ||||||
| PWC (M2-M3) | 0.898 ± 0.022 | 0.906 ± 0.021 | 0.191 | 0.900 ± 0.030 | 0.897 ± 0.033 | 0.427 |
| PWC (M2-M5) | 0.892 ± 0.018 | 0.904 ± 0.013 | 0.029 | 0.902 ± 0.027 | 0.888 ± 0.032 | 0.153 |
| PWC (M3-M5) | 0.896 ± 0.035 | 0.898 ± 0.029 | 0.411 | 0.882 ± 0.026 | 0.889 ± 0.024 | 0.236 |
In the extension phase, the SMT was increased among A muscle cross i.e., PWC (M1-M4), PWC (M1-M6), and PWC (M4-M6); however, it was decreased among B muscles i.e., PWC (M2-M3), PWC (M2-M5), and PWC (M3-M5) without significance (P < 0.05) (Table 7). In MET intervention group, it increased in A and B muscle cross, and there was a significant difference in PWC (M2-M3) and PWC (M2-M5). The results showed that, by increasing the pair-wise coherence in all of the FE-T phases (i.e., standing, flexion, relaxation, and extension phases), the SMT intervention was more effective than MET intervention.
| Extension Phase | SMT | MET | ||||
|---|---|---|---|---|---|---|
| Before | After | P-Value | Before | After | P-Value | |
| A muscles cross | ||||||
| PWC (M1-M4) | 0.896 ± 0.023 | 0.900 ± 0.008 | 0.299 | 0.915 ± 0.028 | 0.908 ± 0.029 | 0.273 |
| PWC (M1-M6) | 0.896 ± 0.031 | 0.902 ± 0.016 | 0.274 | 0.905 ± 0.025 | 0.900 ± 0.032 | 0.334 |
| PWC (M4-M6) | 0.901 ± 0.027 | 0.905 ± 0.014 | 0.349 | 0.909 ± 0.023 | 0.906 ± 0.035 | 0.401 |
| B muscles cross | ||||||
| PWC (M2-M3) | 0.912 ± 0.023 | 0.903 ± 0.016 | 0.077 | 0.915 ± 0.028 | 0.887 ± 0.025 | 0.013 |
| PWC (M2-M5) | 0.907 ± 0.023 | 0.894 ± 0.017 | 0.116 | 0.905 ± 0.025 | 0.888 ± 0.029 | 0.018 |
| PWC (M3-M5) | 0.895 ± 0.017 | 0.894 ± 0.017 | 0.348 | 0.909 ± 0.023 | 0.892 ± 0.033 | 0.089 |
5. Discussion
This study aimed to compare the effects of two manual therapy techniques (SMT and MET) on corticospinal tract function in NS-CLBP by using pair-wise coherence of Bb-IMC during standing, flexion, relaxation, and extension phases that called flexion-extension task (F-ET) phases. The results showed that, by increasing the pair-wise coherence in all of the FE-T phases (i.e., standing, flexion, relaxation, and extension phases), SMT intervention was more effective than MET intervention on supraspinal structures, including the corticospinal tract. Previous studies had mentioned that, as an index of corticospinal activity, Bb-IMC (15 - 35 Hz) was analyzed, and further clinical studies showed that Bb-IMC was decreased or disappeared in spinal cord injury and stroke patients as motor deficits resulting (33, 34). Generally, as a result of a gait rehabilitation intervention, quantification of Bb-IMC was adopted for corticospinal drive monitoring (33, 34). Also, the studies showed that intramuscular coherence could be used to study the effects of interventions quantifying aimed to improve the ability to walk, such as non-invasive brain stimulation or intensive gait training (robot-aided) that may increase the neuroplasticity promote (34). Spedden et al. reported that during a simple task, an age-related oscillatory corticospinal activity reduction in the beta band (35) indicated the corticospinal system efficiency decreased, which led to compensatory strategies to perform a specific task. Whereas, pair-wise coherence among each pair of muscles measurement is useful to highlight the coherence contributions from all synergist muscles or each muscle pair (32). The studies propose that the degree of correlation that is recorded between the different muscle activities can advertise the co-activation of functional, and it may be extended to functionally similar and anatomically close muscles (13, 36) or functionally different and anatomically distant (37). The pair-wise coherence can also be modeled as two terms summation: The one just related to the muscles pair considered (residual) with excluding the third one effects and the one relative to the whole synergy (pair-wise) but with elements synchronized to the third muscle involved activity (31). According to this claim, the pair-wise coherence decline could be explained either by the contribution of coherence decreasing relative to the drive of synergistic (all three muscles common command) or by volley desynchronization that is solely common to the two muscles (31).
In this study, during observing pair-wise coherence of A and B muscle cross in the NS-CLBP intervention groups, before intervention, we noticed that both of pair-wise coherence of A and B muscle cross between each pair of muscle in all phases of FE-T decreased in comparison to healthy subjects that indicated in two NS-CLBP intervention groups patients had a decreased activity of corticospinal tract from of impairments. In line with our findings, AM Castronovo et al. showed the overall cross-muscle coherence decreased at task failure (31). Furthermore, based on previous studies, that showed a reduction in beta-band coherence with movement (38), A-PWC and B-PWC were decreased in the flexion and extension phase compared to their values in the standing and relaxation phase (Tables 2 and 3).
To the best of our knowledge, this is the first study that intended to make a comparison between the two manual therapy techniques' effects on patients with NS-CLBP by using pool coherence of Bb-IMC before and after the interventions. Therefore, we could not compare our results with other studies, but most of the studies that studied the immediate effects of an SMT on patients with NS-CLBP reported that these techniques reduced muscle activity while increased muscle coordination. Ellingsen et al. reported that trunk muscle activation was reduced as established by surface electromyography or functional magnetic resonance imaging after one session of spinal manual therapy technique that involved SMT and mobilization interventions (39). In another study, it was reported that they temporarily reduced EMG activity during an F-ET and, consequently, changed flexion relaxation phenomena parameters (40). Where the results of a recent study supported the idea that the effects of treatment could be mediated by the CNS as neurophysiologic effects rather than just being biomechanically orientated such as releasing adhesions or reducing distortions of the annulus fibrosus, vertebral segments moving to allow in a larger range of motion and the mechanical stress reduce on lumbar erector spine muscles (20), where this model suggests that a cascade of neurophysiological responses (i.e., pain adaptation and pain-spasm-pain models) from both the central and peripheral nervous systems were produced from a spinal manipulation mechanical force that might give explain the improvements in SMT clinical outcomes (41). Interestingly, one SMT proposed effect, which involves salient proprioceptive and sensory feedback by SMT, is that it may help disrupt the relationship among pain anticipation, fear, and movement (39). This study suggests that SMT may reduce affective-motivational and cognitive aspects of fear of movement and anticipated pain, along with corresponding brain processes (39). As far as we know, no study has been interested in studying the effects of MET on the central nervous system. Possibly, it is the first study in this field, and we conclude that MET has no large effect on the central nervous system such as SMT.
The previous studies concluded that the region of SMT was considered to be unimportant, and non–region-specific SMT was just as effective as region-specific SMT in terms of pain intensity (20, 41). Most of the studies have applied the SMT without specifying the segment, where it only identified the painful side and then applied the technique. But because we want to study the central effects of the SMT rather than the biomechanical effects, it is not important for us to identify the segment that has dysfunction. However, we identified patients with dysfunction in one of the segments (L2-L3-L4 segments) to make our study more accurate (20). The effects of the study were strong and statistically significant, although the numbers of samples for the study were relatively small, providing confidence that our findings could reflect the effect of other treatments on NS-CLBP, and we can use Bb-IMC in practical settings to studying the effects of a particular intervention on the corticospinal tract in patients with NS-CLBP patients.
The present study was limited to males and did not include females. This is not considered one of the determinants of the study because the Bb-IMC does not differ according to gender (42). One of the most important determinants of this study was to study the immediate effects of intervention techniques. So, future studies should include long treatment and follow-up assessments. In addition, since Bb-IMC was task-dependent (35), each task requires different coordination patterns among muscles to produce the needed forces and motions. The previous studies demonstrate that analysis of coherence can detect the nervous origin of various coordination patterns of muscle required by different tasks, and the coherence changes across muscles to the "type of task" (32, 38). So the study’s results suggest that the specific type of muscle coordination should be included in this listing to meet the constraints of a given task (32). This necessitates studying other circumstances and functional tasks such as lifting weight.
5.1. Conclusions
It had been stated that manual therapy techniques exert their beneficial effects by affecting the nervous system. But few studies had examined these claims in patients with NS-CLBP. This study provided crucial information about the two common effects of manual therapy techniques for NS-CLBP on the primary motor cortex and corticospinal drive. The results showed that, by increasing the pair-wise coherence of Bb-IMC in all phases of FE-T, SMT intervention was more effective than MET intervention on neurophysiologist consequences, and therefore, it could be useful to secure the optimal treatment when designing the rehabilitation protocol. Another reason that makes our study innovative is that, to date, no studies used pair-wise coherence of beta-band intramuscular coherence to study NS-CLBP and the effects of the various interventions on this population of patients.