1. Background
Carpal tunnel syndrome (CTS) is caused by the compression of the median nerve in the carpal tunnel. The main symptoms of CTS are pain, numbness, and paresthesia in the median nerve innervation regions, including the thumb, the index finger, and the middle and semi-radial sides of the ring finger (1).
The symptoms usually begin gradually and during the night. The pain may spread to the arm. As the disease progresses, there may be muscle weakness in the hand, and the atrophy of the thumb muscles occurs very late in the disease. In more than half of CTS cases, both hands are affected (2).
Diagnosis is made based on specific signs, symptoms, and physical examination and is usually confirmed by electrodiagnostic (EDX) tests. It is assumed that muscle atrophy in the thumb increases the probability of CTS (3).
About 5% of the population in the United States suffer from CTS. Up to 33% of people with CTS may recover within a year without any specific treatment (4). Although CTS is primarily idiopathic, genetic factors are important determinants in developing CTS (1, 2). Also, several studies have demonstrated various predisposing elements, including individual and occupational factors (3-5). Specific occupations and physical exposures, for instance, typists, tailors, butchers, housekeepers, and hairdressers or, in an overall view, manually performed jobs with extensive grip and vibration exposure, are stimulators of CTS (6-10).
Aging and gender are considered two significant risk factors of CTS, as only 10% of CTS reported cases are under 30 years old, and also it affects women three times more than men between 45 and 60 years of age (11). In addition, other studies have shown that individuals with underlying medical conditions, particularly diabetes, arthritis, hypothyroidism, pregnancy, menopause, history of oral contraceptives usage, alcoholism, smoking, BMI above 25 or obesity, and renal and heart failure, are susceptible to developing CTS (12).
2. Objectives
The information on CTS prevalence and risk factors in the Iranian population is limited. This study aimed to provide a comprehensive and detailed overview of CTS prevalence, its personal, psychosocial, and workplace risk factors, and previous medical conditions related to CTS in Iranian patients. To our best knowledge, there is no simultaneous evaluation of CTS incidence and its complex personal, medical, psychosocial, and occupational risk factors.
3. Methods
We extracted data from clinical records of 345 patients who referred to the hand clinic of the Sina Hospital, Tehran, Iran, with complaints of pain and paresthesia in the upper extremities for six months between September 2020 and February 2021. Demographic information, such as sex, age, and underlying disease, including diabetes, hypothyroidism, muscle force examination, deep tendon reflex examination, Tinel’s and Phalen's tests, and electromyography (EMG), and nerve conduction velocity were examined. Finally, the association was evaluated between CTS prevalence and severity with age, sex, clinical examinations, past medical conditions, and occupation in all the cases.
Clinical assessment and EDX examination were performed by different people to follow a blind protocol.
3.1. Clinical Assessment
A fully trained medical doctor performed the clinical evaluation of the patients. The symptoms included pain, numbness, or tingling in the first three digits, palm and wrist, and positive Phalen's test or Tinel's test.
All the patients completed a questionnaire about demographic information, past medical history (including diabetes mellitus and hypothyroidism), past trauma history, and occupational history.
3.2. EDX Assessment
The EDX study was performed with the NeMus device. It was guaranteed to maintain the patients’ hand temperature above 32°C. A median motor nerve conduction study was performed to record initial latency and baseline to peak amplitude from the center of the Abductor pollicis brevis muscle (active site). The stimulation was given orthodromically in the wrist area, 8 cm above the recording site. Also, a median sensory nerve conduction study was performed to record initial latency and baseline to peak amplitude from the third finger (active site) with antidromic stimulation in the wrist area (14 cm above the recorder) and the palm (7 cm above the recorder). The EDX criteria for carpal tunnel syndrome were identified.
The disease severity based on the EMG findings was as follows: (1) mild: sensory distal latency (DL) > 3.6 ms; (2) medium: sensory DL (SDL) > 3.6 ms and motor DL (MDL) > 4.2 ms, motor amplitude > 5 mv; (3) severe: an absence of sensory or motor wave and a decrease in motor wave amplitude and denervation that may be present on EMG: SDL absent, MDL > 6.5 ms, or motor amplitude < 5.
Inclusion criteria: (1) complaints of paresthesia and pain in the upper extremities, (2) age between 15 - 75 years.
Exclusion criteria: (1) lack of patient consent; (2) history of previous surgery of carpal tunnel syndrome; (3) history of hand trauma.
3.3. Statistical Methods
The analysis process was performed using SPSS statistical software version 24.0 (IBM Corp.). Comparisons between the continuous variables were completed using t-test, whereas the categorical variables were compared using the chi square test. We calculated the odds ratio (OR) using univariate analysis with a 95% confidence interval (CI).
P values equal to 0.05 or less were considered statistically significant.
3.4. Ethics
Due to the confidentiality principle, the patients remained anonymous. No written evidence was removed from the patients' clinical records, and no intervention was performed on them. Written informed consent was obtained from all participants.
4. Results
The study sample comprised 345 participants. Table 1 summarizes the demographic characteristics of the cases. Of 345 subjects, 213 (67.1%) met the criteria for CTS. More precisely, 53 out of 100 males and 160 out of 245 females had CTS. We found that CTS was significantly related to gender and that being a female was a risk factor for CTS (P = 0.38). The mean age of the participants was 49.43 ± 13.08, and the study included predominantly female subjects (N = 245, 71%). The mean age of the 213 CTS patients was 53.80 ± 11.57 years, whereas asymptomatic participants were significantly younger (42.39 ± 12.31 years, P < 0.001).
| Respondents Characteristics | Total (N = 345) | Asymptomatic (N = 132) | With Clinically Assessed CTS (N = 213) | P | OR | CI |
|---|---|---|---|---|---|---|
| Sex | 0.038 | 0.599 | 0.373 - 0.961 | |||
| Male | 100 | 47 | 53 | |||
| Female | 245 | 85 | 160 | |||
| Age; mean ± SD | 49.43 ± 13.08 | 42.39 ± 12.31 | 53.80 ± 11.57 | < 0.001 | ||
| PMH | 29 | 6 | 23 | 0.08 | ||
| DM | 9 | 1 | 8 | 0.089 | 0.196 | 0.024 - 1.582 |
Abbreviations: OR, odds ratio; CI, confidence interval; PMH, past medical history; DM, diabetes mellitus.
Of the 213 CTS cases, 190 (89.2%) had bilateral involvement, 17 (7.9%) had right hand involvement, and six (2.8%) had left hand involvement.
Of the 345 patients, only four with CTS had positive Phalen's test based on physical examination. However, the Phalen's test results were not statistically associated with the CTS status (P = 0.302). Five patients with CTS had positive Tinel’s test. However, the Tinel’s test results were not significantly related to the CTS status (P = 0.161). Three patients had a reduced force in the hand region (4/5), of whom only one had CTS. In total, muscle force was not related to CTS (P = 0.561). Six patients had bilateral hand muscle atrophy, five had right hand muscle atrophy, and one had left hand muscle atrophy, who were all CTS positive cases. Atrophy and CTS did not retain statistical significance (P = 0.53).
Twenty-nine participants had a history of a previous medical condition including diabetes mellitus (N = 9, 2.6%), trigger finger (N = 9, 2.6%), hypertension (N = 2, 0.6%), rotator cuff tendonitis (N = 2, 0.6%), breast cancer (N = 2, 0.6%), rheumatoid arthritis (N = 1, 0.3%), multiple myeloma (N = 1, 0.3%), hypothyroidism (N = 1, 0.3%), hemangioma (N = 1, 0.3%), and Chiari malformation (N = 1, 0.3%). There was no significant correlation between comorbid conditions and CTS incidence.
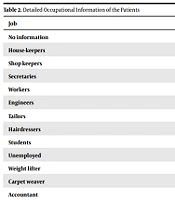
Regarding occupational history (Table 2), only 117 patients had consent to share their information. Among these 117 cases, there were 70 housekeepers, 16 shopkeepers, ten secretaries, seven workers, three tailors, two engineers, two hairdressers, two students, two unemployed, one weight lifter, one carpet weaver, and one accountant. We did not find any association between occupational categories and CTS prevalence (P = 0.091).
| Job | CTS Positive | CTS Negative | Total |
|---|---|---|---|
| No information | 141 | 87 | 228 |
| House-keepers | 51 | 19 | 70 |
| Shop keepers | 8 | 8 | 16 |
| Secretaries | 6 | 4 | 10 |
| Workers | 5 | 2 | 7 |
| Engineers | 0 | 2 | 2 |
| Tailors | 1 | 2 | 3 |
| Hairdressers | 0 | 2 | 2 |
| Students | 0 | 2 | 2 |
| Unemployed | 0 | 2 | 2 |
| Weight lifter | 1 | 0 | 1 |
| Carpet weaver | 1 | 0 | 1 |
| Accountant | 1 | 0 | 1 |
Moreover, the jobs were categorized into hard, medium, and easy based on the use of hands and fingers. There was no difference in CTS prevalence between the job categories (P = 0.252).
For a more detailed analysis, we divided CTS into three groups by intensity; 64 (30%) patients had severe CTS while 105 (49.3%) and 44 (20.7%) patients had moderate and mild CTS, respectively. CTS intensities appeared to be significantly related with age (0.024), and patients with higher CTS intensity had older ages. There was no statistically significant difference between the CTS intensity subgroups with gender (P = 0.922), Tinel’s test (P = 0.065), Phalen's test (P = 0.232), force (P = 0.145), comorbid conditions (P = 0.543), DM (P = 0.369), occupational history (P = 0.272), and occupational hardship (P = 0.739).
5. Discussion
With 345 participants and 213 confirmed CTS cases, this study identified age and gender as prominent elements of inducing CTS. All patients with CTS in our study were between 40 and 60 years, and around 75% of the subjects suffering from this condition were female.
These results are consistent with previous literature, showing that the highest prevalence of CTS is in the fifth to sixth decades of life (13, 14). It has been reported that age-related physiological changes and exposure to long-term work may cause an increase in CTS prevalence (3). Studies have shown that CTS severity is also associated with aging, and more extreme pathophysiological processes were detected by EDX analysis in the elderly (15); however, a recent study noted that symptoms were more severe and recurrent in younger individuals (16). Although the correlation between CTS prevalence and age is proven, the association between CTS intensity and age is inconsistent. We found that older age was significantly associated with higher CTS intensity. This issue needs to be addressed in future studies to determine if younger CTS patients suffer from greater symptoms and its pathophysiology.
Our results regarding female domination in CTS are compatible with several previous studies. Statistics show that women suffer from this problem almost three to four times more than men (17, 18). This discrepancy was previously explained by females' genetics and their hand and wrist anthropometric features (19).
Despite the lack of statistical relevance between CTS prevalence with intensity and occupational history in our study, the role of manual activities cannot be underestimated in CTS occurrence. Repetitive wrist movement is a known risk factor for CTS. We had limited information about the patients’ occupations, and only 117 individuals shared their occupational status, of whom 70 were housekeepers. A previous study in Iran showed that houseworkers had the highest frequency of CTS among people with different occupations (20). It seems like, with the advancement of technology, housekeeping requires less manual work, and it is no longer a risk for developing CTS. It is an important finding that highlights the role of technology in improving the quality of our lives. As for the rest of the jobs, we had few patients. However, we cannot state that jobs reviewed in this study are not related to CTS despite our insignificant results in this regard. For elucidating this association, each job should be surveyed exclusively with a group of controls to provide a sufficient population.
We noticed that 89% of our cases had bilateral hand involvement. This is concordant with previous literature showing that most reported cases had bilateral CTS manifestations (21). However, CTS occurs more intensely in the dominant hand. According to a recent review, this is due to central nervous system sensitization (22). We did not address the question of whether the dominant hand preceded the other hand regarding CTS symptoms.
According to our physical examination, CTS prevalence and severity were not correlated with Tinel’s and Phalen's tests. In line with our results, another study expressed no significant relationship between clinical findings and electrophysiological CTS severity (21). Some other studies have presented contradictory results and a significant correlation between positive Tinel’s and Phalen's tests with CTS prevalence (18, 23). Future studies are needed to examine this issue with more sensitive tests and a larger population to resolve these controversies.
Total muscle force and hand muscle atrophy did not appear related to CTS in our assessment. Previous findings revealed that thenar atrophy could reflect the severity of CTS (15). However, another study reported thumb abduction strength was not effective enough to measure CTS severity, and their patients did not have detectable muscular atrophy (24). It sounds like with increased public awareness, individuals suffering from paresthesia and numbness seek treatment before serious functional problems and muscle atrophy occur, and early CTS diagnosis and follow-up medical interventions can prevent hand atrophy.
We did not observe any association between underlying diseases and CTS incidence. Since only 13% (29 individuals) of our subjects had PMH, our results do not necessarily rule out the link between PMH and CTS. A limited number of participants with an underlying disease is probably why our results are inconsistent with other articles. A study on the Iranian population mentioned that BMI was 30 to 40 in 52% of patients. Some studies have considered BMI > 29, diabetes, thyroid dysfunction, and rheumatoid arthritis major risks of CTS (20, 25-28). Another study did not find any significant difference between underlying conditions, except for diabetics and obesity, and CTS. Therefore, a large population comparative investigation designed to precisely assess each disease may help find the exact association of the disease with CTS. A future prospective study is needed to examine CTS incidence in subjects with obesity, diabetes, thyroid dysfunction, and rheumatoid arthritis. In case of a significant correlation between CTS incidence and diseases mentioned above, a screening about underlying diseases is needed at the beginning of CTS diagnosis.
As a final point, based on our results, age and gender were two crucial factors in CTS, and underlying occupational risk factors, underlying diseases, positive Tinel’s and Phalen's tests, and muscle atrophy were not correlated with CTS prevalence and intensity. This is an important finding, meaning that most CTS cases were idiopathic. Although this might mean that CTS prevention is still somehow futile, CTS diagnosis can prevent functional problems and lower the cost of surgeries. This highlights the role of CTS screening in all populations. At last, it is better to repeat this research in a larger group of people and investigate the effect of each risk factor more precisely to obtain more accurate results.