Dear Editor,
The novel coronavirus disease 2019 (COVID-19) is in the pandemic stage, and there are concerns about patients with autoimmune diseases (1, 2). Neuromyelitis optica spectrum disorder (NMOSD) is an autoimmune disease of the central nervous system (CNS), which predisposes cases to increased risk of infection based on immunosuppressive treatments (3). Up to now, NMOSD cases have been evaluated regarding COVID-19 infection, and different infection rates have been reported.
Thus, the aim of this systematic review and meta-analysis was to estimate the pooled prevalence of COVID-19 infection in patients with NMOSD.
Two independent researchers searched PubMed, Scopus, EMBASE, Web of Science, and google scholar and also gray literature up to October 20, 2020.
The search syntax for searching in PubMed was (coronavirus OR Wuhan coronavirus OR novel coronavirus OR coronavirus disease OR COVID-19 OR 2019 novel coronavirus infection OR 2019-nCOV OR severe acute respiratory syndrome coronavirus 2 OR SARS-CoV-2) AND Neuromyelitis optica spectrum disorder OR NMOSD OR Devic syndrome OR Neuromyelitis optica spectrum disorders.
STATA (Version 13.0; Stata Corp LP, College Station, TX, USA) was used for data analysis. Inconsistency (I2) was calculated for heterogeneity evaluation.
We found 54 articles; however, after careful evaluation, five manuscripts were included for meta-analysis. Totally, 3458 patients with NMOSD had been evaluated (Table 1).
| Study | No. of Patients | Mean Age | F/M | Mean Disease Duration | The Most Common Symptoms | No. of Patients With COVID-19 | No. of Hospitalized Patients | ICU Admission | Death |
|---|---|---|---|---|---|---|---|---|---|
| 1. Zeidan et al. (4) | 75 | 43.9 | 3.68 | 6 | Fever, cough, asthenia, headache, diarrhea, ageusia/anosmia, asthenia, and headache | 5 | 1 | 0 | 0 |
| 2. Mirmosayyeb et al. (3) | 157 | 38 ± 10.8 | 0.256 | 6 ± 4 | myalgia, and headache/vertigo | 8 | 3 | 1 | 0 |
| 3. Tomczak et al. (5) | 17 | - | 4.6 | - | Respiratory Symptoms, including fever, chills, and shortness of breath | 2 | 0 | 0 | 0 |
| 4. Fan et al. (6) | 3060 | - | - | 4/94 | - | 2 | 0 | 0 | 0 |
| 5. Sahraian et al. (7) | 149 | 37.55 ± 11.57 | 6.22 | 7.95 ± 4.71 | Fever, Dyspnea, myalgia, Gastrointestinal complications, fatigue, and vertigo | 5 | 3 | 0 | 0 |
Findings of the Included Studies
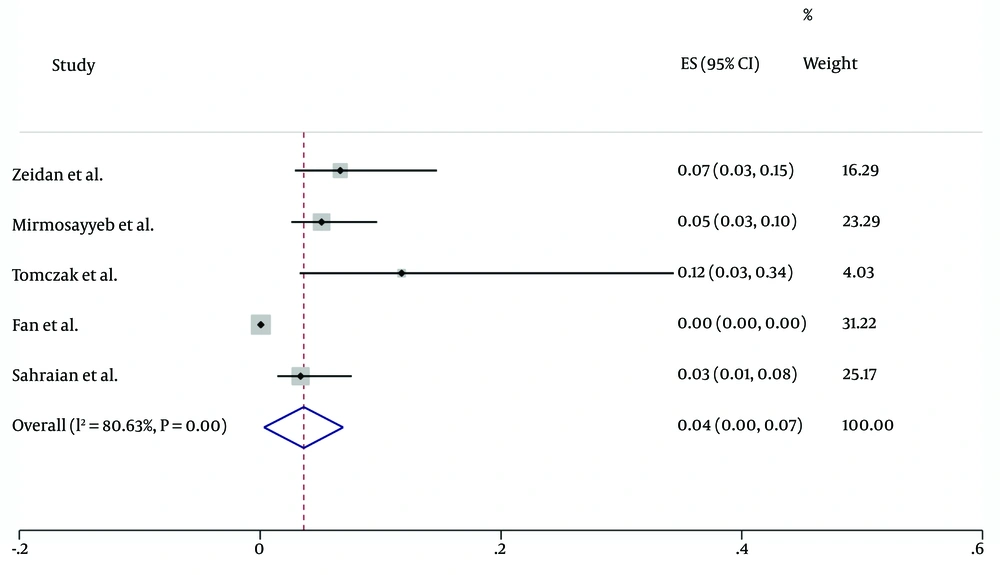
The pooled estimate of COVID-19 infection in NMOSD patients was 2% (95% CI: 0 - 7%) (I2 = 80.6%, P < 0.001) (Figure 1).
Patients with NMOSD are prone to a wide range of infections based on immunosuppressive treatments and concerns raised during the COVID-19 pandemic. The incidence of COVID-19 in the general population ranges from 0.35 to 13.3% (8), while in NMOSD patients, the prevalence ranges from 0 - 12%, and most cases had mild infection without the need for hospitalization (only seven out of 3458 hospitalized cases) or ICU admission (only one) as it is shown in Table 1. The results also showed that no death was reported among NMOSD patients. This could be based on great care of these patients and also following preventive strategies and strict quarantine rules (3). Previous findings have shown that B cell depleting agents do not increase the risk of infection in NMOSD patients (3, 7).
A limited number of the included studies is the limitation of this study. The prevalence of COVID-19 infection is rare in NMOSD patients.