1. Background
Spinal cord injury (SCIs) is a chronic condition leading to physical and psychological problems along with numerous economic burdens for patients (1). There are about 1 million patients with SCIs in the United States, and the number is growing by about 12,000 annually (2). The causes of SCI include falls, fights, accidents, and sports injuries, making it a chronic disease (3). Health professionals have been trying to improve the health of these patients, but unfortunately, despite countless efforts in this area, the sensorimotor function of these patients has not been fully improved. In fact, muscle atrophy due to SCIs, as well as nerve damage, affect the performance of these patients (4, 5).
Spinal cord injuries also affect the mental and emotional functioning of patients and their families. In a meta-analysis study of 41 articles, Aaby showed that these patients had a low level of life satisfaction and quality of life and high rates of anxiety, stress, and post-traumatic stress disorder. Other studies have also indicated that this disease can lead to disruptions in employment, friendships, and family relationships that ultimately reduce a person's participation in society (6-8). Also, in a meta-analysis study of 25 articles, Wei et al. exhibited that these patients had venous thromboembolism (9). Moreover, in another meta-analysis study of 37 articles, Hunt et al. showed that the prevalence of post-SCI pain was 68% (10).
In late 2019, an unknown disease called COVID-19 broke out, which quickly spread throughout the world. Its symptoms include cough, fever, nausea, tachypnea, tachycardia, diarrhea, and various types of pain, including headache, myalgia, sore throat, and chest pain (11, 12). Since its onset, COVID-19 has caused important and fundamental challenges for health care systems and has become one of the main health problems worldwide, and patients with SCIs have faced new challenges after the outbreak of COVID-19 (13, 14). Patients with SCIs who develop COVID-19 are at a higher risk for respiratory problems and other complications (15).
COVID-19 pandemic will be eventually eradicated at some point, but the physical and mental disorders created in these patients may be persistent and become chronic. Given that crises such as COVID-19 have a novel and uncertain nature, it is necessary to study the subsequent stresses in all respects (16, 17). In this novel disease, taking timely and prompt measures requires correct knowledge of the epidemic situation in the society and its consequences, so that the necessary interventions for the health of patients can be evaluated (18).
2. Objectives
Considering the prevalence of COVID-19 and the importance of conducting research on this emerging disease, as well as the fact that patients with SCIs, in addition to the problems associated with this chronic disease, have also experienced COVID-19, the aim of the present study was to determine the challenges of SCI patients during the COVID-19 pandemic.
3. Methods
3.1. Study Design
This was a qualitative study performed among SCI patients after obtaining the code of ethics from the Research Ethics Committee of Ilam University of Medical Sciences (IR.MEDILAM.REC.1400.083) in 2021. The purposive sampling method was used, and the sample size was determined based on data saturation.
3.2. Inclusion and Exclusion Criteria
3.2.1. Inclusion Criteria
The inclusion criteria included patients suffering from SCIs for at least one year, the ability to speak and communicate verbally, and informed written consent to participate in the study.
3.2.2. Exclusion Criteria
The exclusion criteria included the presence of active psychotic disorders, drug use, and a tendency to withdraw at any time of the study. The informed consent form was completed taking into account the health protocols. Interviews were also conducted during non-peak hours. Patients expressed their permission to record their voices, and they were assured that all the information would be reported confidentially.
3.3. Data Gathering
3.3.1. Demographic Characteristic
The form of demographic characteristics included items on the history of SCI, age, sex (female, male), education (illiterate, diploma, undergraduate, and university), and marriage (married or unmarried).
3.4. Method of Research
The researchers enrolled patients with SCIs by the available sampling method. Data were collected using semi-structured, face-to-face individual interviews in accordance with the health protocols in a safe environment without stress until reaching data saturation. Data were saturated after interviewing nine patients, and to ensure data saturation, two additional interviews were conducted. In-depth interviews and note-taking were also carried out. After recording the voices and completing the interviews, the researcher transcribed the data on paper, and the concepts and phrases were analyzed. Each interview lasted between 30 and 45 minutes, depending on the condition of each patient.
After the interviewee's basic acquaintance with the objectives of the research and the conditions of the interviews, the researchers started interviews by asking questions such as “What were the limitations you had during the COVID-19?”, “What problems did you have during the COVID-19?”, “What was the difference between the physical care needs you had at the time of COVID-19 pandemic and the pre-pandemic phase?”, ”What was the difference between the psychological needs you had at the time of COVID-19 pandemic and the pre-pandemic phase?”, “What have you been worried about since the COVID-19?”, “How is the amount and type of care provided by your caregivers different from the pre-pandemic period?”, and “How has the spread of COVID-19 affected your health care?”.
3.5. Data Analysis
Quantitative variables were analyzed using SPSS version 16, and descriptive (mean and standard deviation) and inferential statistics were used to differentiate between the intervention groups. The written file of the interviews was analyzed using MAXQDA software. The researcher started coding after reading the interviews carefully and determining its general meaning and thinking, and pondering on each sentence. Similar codes were then categorized, and themes were formed.
4. Results
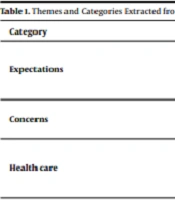
The mean (standard deviation) age and history of SCI of the participants were 54.2 (9.8) and 12.8 (4.9) years, respectively. Thirty-two percent of the participants were female and 68% were male. In terms of education, 57% of the patients were illiterate, 38% had a diploma, and 5% had a university degree. Also, 68% of the patients were married, and 32% were single. According to Table 1, after analyzing the data obtained from the semi-structured and in-depth individual interviews, three main themes, including expectations, concerns, and health needs, were extracted (Table 1).
| Category | Theme |
|---|---|
| Expectations | Need for financial support |
| Need for social support | |
| Need for physical support | |
| Concerns | Fear of death |
| Fear of loneliness | |
| Health care | Health literacy |
| Access to services | |
| How to get informed about the infection |
4.1. Expectations
"Expectations" was one of the main themes extracted from the interviews that examined patients' challenges during the COVID-19 pandemic. The above theme included the three categories of need for financial support, need for physical support, and need for social support.
4.1.1. Need For Financial Support
"Apart from the treatment costs related to my illness, now I have to pay for the purchase of masks, gloves, alcohol, etc. I really do not have money."
"Coronavirus has made my spouse work fewer hours and not be able to afford our living expenses. I also have to be more careful about home expenses. For example, last month, I wanted to buy a wheelchair and I couldn't. Now my own wheelchair is completely broken."
"If I want to go to Tehran to follow up on my treatment, I can no longer travel by plane. I'm afraid of bus due to risk of infection. That's why I delayed my visit to Tehran so that the pandemic may end, and I would go then."
4.1.2. Need For Social Support
"I used to be lonely, and now I'm lonelier. No one has visited us since the onset of the COVID-19 pandemic. No one is asking about us. Everyone is afraid of getting the infection."
"The pre-pandemic phase was good because we could go to the park, have a party, go to a wedding, etc. But since the onset of the disease, we have been very lonely. No one comes to visit us."
"All I do is sit inside the house and look at the furniture in the house. There is no one to talk to. My spouse goes to work and I'm alone at home."
4.1.3. Need for Physical Support
"Before the outbreak, there was someone to help us, and to hold our hand, but now no one is helping. Everyone is running away from each other. They are right, they are afraid to get the infection. But, well, we are alone and have to cope with our disease and do our tasks by ourselves."
"I went with my daughter to visit the doctor the other day. I was very upset. My daughter could not move my wheelchair and it was heavy. Nobody wanted to come to help. People used to help before. I eventually asked someone for help."
"Before the pandemic, my granddaughter was always by my side and helped me, but she has not come since the COVID-19 outbreak..."
"Before the pandemic, I could do a lot of my tasks. For example, I could go to a bakery, a shop, etc. But now I'm afraid to get the infection. I always have to wait for my son to come back from work and do my tasks. My poor son is very upset, but he supports me."
4.2. Concerns
Another theme extracted was patients' concerns about the COVID-19 disease. Concerns included fear of death and fear of loneliness.
4.2.1. Fear of Death
"The first day they informed us about the COVID-19 outbreak, I was very worried. I thought I was going to die."
"I'm always stressed. What if I get the infection and die?! Our bodies are much weaker, and we suffer. I'm very stressed to die."
"I have no fear of dying from my own disease or any other disease. We will all die in the end. But it makes me anxious to get infected with COVID-19 and die."
"I'm afraid I get the infection and the whole family will die, wow, that's really horrible."
"Since the onset of the COVID-19 pandemic, I have not left the house at all because I did not want to get the infection. I am sad when I visit my children by force during the COVID-19 peak times."
"The thought that all of us will die has always made me sad. It’s all silent and in low spirits. I'm much less prone to talk. I'm very bored."
4.2.2. Fear of Loneliness
"I got COVID-19 just upon the onset of the disease. I was hospitalized, too. No one came to visit me. I had a feeling of extreme sadness of being alone. It was horrible. On the one hand, I had physical problems in the hospital, on the other, I was alone and had no one."
"Even if I get the infection, I'm afraid to tell someone I got it because everyone will be afraid and run away from me."
"I had not yet received my test result that none of the neighbors came near our house anymore."
4.3. Healthcare
Another extracted theme was related to health care, which included two subcategories: (1) health literacy; and (2) access to services.
4.3.1. Health Literacy
"I do not know anything about this disease. What it is, where did it come from, and what will happen in the end and ..."
"They say that whoever has an underlying disease and gets this disease, (s)he will surely die, I don't know how true this is."
"I always felt it is not true and no one would get the infection until my spouse got infected."
"I have to call my family and friends to give me some information about corona. I do not know what it is. I called so that maybe someone would know and tell me."
4.3.2 Access to Services
"Oh, with all these problems, where can I buy a mask and alcohol, then where can I find it with all these problems?"
"Even though I have diabetes and I always went to the doctor to check my blood sugar, I was scared and I did not go to the doctor at all since the onset of the COVID-19 pandemic."
"I cannot go online to learn about corona because of my physical problems and lack of knowledge about computers. The kids always watch TV, and they do not let me watch anything on TV. I feel uncomfortable because I have no information."
"Some time ago I needed a doctor. I had to stand on a long queue and wait. I waited a long time. Instead of telling them to come at a specific time, I waited a long time."
"I wish they could do a lot of medical work at home. This is very bad that we get the coronavirus just by going to the hospital to receive iv-serums or shots."
"I wish they could do the COVID-19 test at home. It's hard to go out."
"I live in a village. It would be good for me not to take all this long distance to visit the doctor and not to be infected with the coronavirus."
4.3.3. How to Get Informed About the Infection
"A hospital employee told my family that I was infected. My whole family ran away from me. My relatives also ran away. I wish they had not said this to anyone. Maybe we would not like anyone to know about our disease."
"All of a sudden, they told me that I got the coronavirus and I was shocked. I was about to die. I wish they hadn’t told us we were infected and just said it was a simple cold."
5. Discussion
The aim of the present study was to determine the challenges of patients with SCIs during the COVID-19 pandemic. Patients with SCIs suffer from various problems, including pain (10), anxiety, depression (19), venous thromboembolism (20), pressure ulcers (21), and autonomic dysreflexia. This is the first qualitative study on the challenges of patients with SCIs during the COVID-19 pandemic in Iran. Since there has been no similar article, the results of the present study will be compared with other similar studies. The results of this study showed that these patients faced challenges in the three areas of expectations, concerns, and health care during the outbreak of COVID-19, which will be discussed.
These patients faced challenges in the three areas of need for financial support, need for social support, and need for physical support during the of COVID-19 outbreak, which will be compared with the results of other studies. In a qualitative study, Fatehi And Kamali showed that family support plays a very important role in returning patients with SCI to employment status. Moreover, one of the main themes extracted was "the role of the family" as working people referred to the significance of psychological support of the family members for their employment (22). Consistent with the present study, Ghaderi et al. referred to social factors, such as participation in social groups supporting SCIs, job creation, financial, emotional support, and family empathy, as effective factors in post-traumatic growth in patients with SCIs (23).
Among the ''concerns'' theme, patients with SCIs referred to the two concerns of fear of loneliness and fear of death as their challenges. In a study of the elderly's experiences during quarantine, Gholamzad et al. found that one of the main extracted themes was negative outcomes, including illness anxiety disorder, social isolation, mood problems, interpersonal conflicts, and death anxiety (24). In a study, García-Rudolph et al. showed a high rate of anxiety and depression among SCI patients (25), which is consistent with the results of the present study suggesting the fear of death and fear of loneliness among the patients.
With regard to the “health care’’ theme, the challenges facing SCI patients since the onset of the COVID-19 outbreak included health literacy, access to services, and how to get informed about the infection. In a study of factors influencing the acceptance and adaptation to SCIs, Khanjani et al. showed that structural and contextual barriers in SCI patients included health-related problems and ignoring the disabled (26), which is consistent with the results of the present study. On the other hand, Gholamzad et al. (24) showed in their qualitative study that one of the positive outcomes of quarantine during the COVID-19 period was the improvement of lifestyle, and the extracted meaning included increasing self-care, increasing media literacy, and developing healthy habits, which is not consistent with the results of this study suggesting the existence of health challenges among SCI patients at the time of the COVID-19 pandemic. One of the reasons for this discrepancy is the difference in study populations. In the present study, SCI patients were investigated, while in the study by Gholamzad et al. (24), the elderly were investigated.
5.1. Conclusion
Considering the challenges in the three areas of expectations, concerns, health care, it is necessary to take appropriate measures to eliminate these challenges.
.png)