1. Background
Intensive care unit (ICU) patients are at risk of neurological complications. Changes in patients'
neurological status can predict complications (such as sepsis) and the course of the disease. Mortality and morbidity of patients and staying in the ICU increase as the incidence of neurological complications increases (1). Therefore, scoring systems for the severity of illness are usually applied in the intensive care unit (2). The most common neurological diagnosis among patients admitted to ICUs is delirium. The incidence of delirium in the ICU is reported to be 16 to 89%, which is accompanied by many complications (3, 4). What is most important for neurosurgical patients is measuring their consciousness level (5). Several scales have been designed to determine the patients' level of consciousness; however, the most commonly used scale has been the Glasgow Coma Scale (GCS). This scale is used by physicians and other members of the health team to obtain accurate reports of the patient's state of consciousness (6). The GCS is one of the best-known scales for evaluating and predicting the outcome of these patients (7).
Currently, the GCS, known as the most widely used scale, is used worldwide; however, it has some drawbacks that have been addressed in numerous books and articles (8), including the verbal response that cannot be evaluated in intubated patients and no fair and equal scores given to the three domains of verbal response, eye-opening, and motor response. Also, in high scores, GCS has no sensitivity needed to predict patients' recovery and is also affected by the users' experience, personal taste, agitations, and the inability of some patients to respond to questions. Studies have shown that inexperienced personnel have made serious mistakes in evaluation, and overestimated or underestimated its value on average, even by 4 - 5 degrees (8-11).
A relatively new full outline of unresponsiveness (FOUR) score coma scale has recently been introduced by a neuroscientist named Wijdicks in the U.S. Mayo Clinic, which is growing and spreading to all languages and has been introduced as a good substitute for GCS (12). Unlike the GCS, the FOUR scale cannot evaluate the verbal function and can just examine intubated comatose patients and those having tracheostomy more precisely. The FOUR scale has four components of eye responses, motor responses, brainstem reflexes, and respiration patterns, with a maximum score of 4 and a minimum score of 0 for each component. The evaluation of all the components of this scoring system usually takes a few minutes, and the total score ranges from 0 to 16 (13). The results of a study by Nazari Ostad et al. (14) showed that despite many advantages of the FOUR criterion over the GCS criterion, no score has been considered for patients undergoing oxygen therapy via endotracheal tubes in this criterion.
In addition to the scales mentioned, the Richmond Agitation-Sedation Scale (RASS) is considered the most valid and reliable sedation assessment tool to measure the quality and depth of sedation in ICU patients. The RASS has the highest validation scores and can detect different levels of sedation in different clinical conditions. In addition, the RASS consistently provides a consensus target for goal-directed delivery of sedative agents. However, scales such as RASS require subjective evaluation, which may cause changes in measurement and clinical practices, especially when there are irregular or excessive working hours. Moreover, physicians and nurses occasionally have no sufficient experience, as well (15). In a multicenter prospective clinical validation trial, the Brain Function Index (BFI), as an EEG-only and objective assessment of brain function abnormalities, was shown to scale with the severity of functional impairment (16-18), which indicates advanced signal processing measures reflecting physiological changes reported in cognitive function studies on brain injury (17). Many studies have been conducted, including hypothetical clinical trials and objective studies; however, no study has been performed to compare the correlation and numerical values of BFI with the criteria mentioned earlier.
2. Objectives
Therefore, this study aimed to evaluate the correlation of the brain function index (BFI) with three common sedation scales, namely Glasgow Coma Scale (GCS), Richmond Agitation-Sedation Scale (RASS), and FOUR score at the intensive care unit (ICU) of Imam Reza and Valiasr hospitals in Birjand.
3. Methods
This study was a descriptive-analytical study performed in the autumn and winter of 2018 in two
university hospitals (Imam Reza and Valiasr Hospitals) in Birjand. All patients who met the inclusion criteria were enrolled in the research by the census. After approval of the University Ethics Committee (ir.bums.rec.1397.86), complete explanations were provided to the patients' companions. Also, written informed consent was obtained from the patients' legal guardians.
3.1. Study Population
A total of 85 patients with decreased consciousness were included. Inclusion criteria included patients aged over 15 years who required no muscle relaxants and had no hearing or visual impairment, mental retardation, mental disorder, hemodynamic instability (MAP < 60 mmHg), and hypoxia (SpO2 < 90%), as well as patients with no brain electrical activity disorders such as epilepsy and focal brain disease, and those who had not undergone anesthesia and surgery for the past 24 hours. Patients with suspected brain death (GCS = 3 and no brainstem reflexes) and those who were not able to be examined three times due to death or other factors, as well as patients who had serious complications during the study period, including seizures, oxygen desaturation, hypotension, shock, and hypoglycemia (BS < 70) or hyponatremia (Na < 118) were excluded from the study.
A researcher-made checklist was used to collect the data, which included two sections as follows: (1) demographic information including age, sex, and type of disease; and (2) information related to patients' records, including diagnosis, cause of decreased consciousness, presence or absence of endotracheal intubation and ventilatory support, and sedative prescription, including the type, dose, and time of administration.
Then, the BFI and three clinical criteria of sedation and consciousness reduction, including RASS, GCS, and FOUR score were checked three times with the interval of at least four hours during a 24-h period, and values were recorded. For patients who were intubated, the GCS was assessed based on 10 scores (eye-opening and motor responses), BFI was assessed by a project executer resident using a SAADAT monitoring device, and clinical criteria were assessed by an anesthesiologist and a neurologist using the relevant checklist. The two groups were blinded to the numerical values of the other group. The mean BFI was recorded over three minutes for greater accuracy. Vital signs including mean arterial pressure (MAP), heart rate (HR), and percentage oxygen saturation of hemoglobin (SpO2) were measured and recorded by another nurse using the SAADAT monitoring device. The validity of the researcher-made checklist was confirmed by expert professors, and Cronbach's alpha was used to determine its reliability.
3.2. Statistical Analysis
Data were analyzed using SPSS18. First, descriptive indices including mean, standard deviation, and frequency were reported. To investigate the variables, the assumption of normality was first checked using the Kolmogorov-Smirnov test. The Mann-Whitney test was then used, as the data were non-normal. Besides, the Spearman correlation test was used at a significance level of 0.05 to determine the relationship between variables.
4. Results
In this study, 85 patients including 45 (52.9%) males and 40 (47.1%) females were enrolled.
Considering the age, 24 (28.2%) patients were under 40 years old, 13 (15.3%) patients were between 41 and 60 years old, and 48 (56.5%) patients were over 61 years old. Also, 34 (40%) patients were intubated and 51 (60%) patients were not. The mean BFI score of patients admitted to the ICU was 77.12 ± 24, and the mean level of consciousness of patients admitted to the ICU was 11.63 ± 4.06, -1 ± 2.56, and 12.21 ± 4.39 in terms of GCS, RASS, and FOUR score scales, respectively.
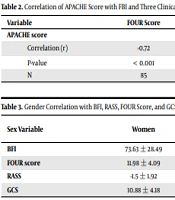
There was a significant positive relationship between the BFI score of patients hospitalized in the ICU and the scores of consciousness based on RASS, FOUR score, and GCS scales (P < 0.05). Accordingly, the correlation of the BFI with the FOUR score was stronger than those with other two criteria (Table 1). Also, there was no significant relationship between the BFI score of patients admitted to the ICU and age (r = -0.08; P = 0.45). A significant negative relationship was observed between the APACHE-II score and the scores of BFI and three clinical criteria in hospitalized patients in the ICU, in which the higher the APACHE-II score, the lower the scores of BFI and the three clinical criteria (P < 0.05) (Table 2).
| Variable | FOUR Score | RASS | GCS |
|---|---|---|---|
| BFI | |||
| Correlation (r) | 0.63 | 0.53 | 0.61 |
| P-value | < 0.001 | < 0.001 | < 0.001 |
| N | 85 | 85 | 85 |
| Variable | FOUR Score | RASS | GCS | BFI |
|---|---|---|---|---|
| APACHE score | ||||
| Correlation (r) | -0.72 | -0.51 | -0.78 | -0.71 |
| P-value | < 0.001 | < 0.001 | < 0.001 | < 0.001 |
| N | 85 | 85 | 85 | 85 |
The mean BFI score was reported to be 78.11 ± 24.18 for men and 73.63 ± 28.49 for women. Also, the mean scores of FOUR score, RASS, and GCS criteria were 12.16 ± 4.80, 0.7 ± 3.18, and 11.93 ± 4.06 in men, and 11.98 ± 4.09, -1.5 ± 1.92, and 10.88 ± 4.18 in women, respectively. Moreover, the Mann-Whitney U test results showed no significant difference in BFI,
FOUR score, RASS, and GCS scores between men and women (P > 0.05) (Table 3).
| Sex Variable | Women | Men | Mann-Whitney | |
|---|---|---|---|---|
| z | P | |||
| BFI | 73.63 ± 28.49 | 78.11 ± 24.18 | -0.03 | 0.97 |
| FOUR score | 11.98 ± 4.09 | 12.16 ± 4.80 | 0.617 | 0.537 |
| RASS | -1.5 ± 1.92 | 0.7 ± 3.18 | -1.25 | 0.21 |
| GCS | 10.88 ± 4.18 | 11.93 ± 4.06 | -1.06 | 0.288 |
a Values are expressed as mean ± SD.
5. Discussion
This study was a prospective descriptive study conducted on 85 patients admitted to the intensive
care unit (ICU) of Imam Reza and Valiasr hospitals in Birjand, during the winter of 2018, aiming at assessing the correlation of the Brain Function Index (BFI) with three common sedation scales, as Glasgow Coma Scale (GCS), Richmond Agitation-Sedation Scale (RASS), and FOUR score. The results of this study showed that there was a significant positive relationship between the BFI score of patients hospitalized in the ICU and the score of patient’s consciousness level based on RASS, FOUR score, and GCS scales (P < 0.05). Also, the correlation of the BFI with the FOUR score was higher than those with the other two scales. In a study by Iyer et al. (19) conducted on 100 ICU patients, it was found that the inter-rater agreement was excellent in each of the four domains of the FOUR score, such as GCS. While the FOUR score was applicable to all patients, including intubated patients, the lowest FOUR score (zero) was better correlated with mortality than the lowest GCS score (three). In addition, researchers in a systematic review in 2018 found that the FOUR score could provide better predictors and more useful and reliable results for physicians and nurses (20).
In the study by Turkmen et al. (21), the RASS was significantly correlated with bispectral index values during dexmedetomidine infusion among critically ill patients requiring mechanical ventilation in the ICU. Also, in another study (22), the routine RASS assessment of arousal during clinical care was considered necessary because it was related to prognosis.
The findings of our research showed that gender was not significantly correlated with BFI and the three clinical criteria used for assessing the level of consciousness. In this study, it was also found that there was no significant relationship between the BFI score of patients admitted to the ICU and patients' age. Although no study was found in this regard to compare, this result was different from those obtained among traumatic brain injury patients, and it can be said that it is in some way inconsistent with the study by Lueckel et al. (20). The study also pointed to the increased hospitalization of elder adults in the hospital and deaths resulting from traumatic brain injury; they also found that in 2018, among 134 children who suffered from moderate to severe traumatic brain injury, six children died. At Rhode Island Hospital, more than 800 adult patients with traumatic brain injury were reported to be annually hospitalized; more than 500 adult patients with traumatic brain injury required long-term care, and more than 100 patients died in acute conditions (20), which indicates the effect of age. Also, the injury mentioned in this study was falling, which may be due to the loneliness of the elderly in foreign countries and their late arrival at the hospital. However, in Iran, the elderly are usually not alone, and patients' quick delivery to medical centers and providing a rapid response to patients could reduce this mortality rate.
Other results of this study showed that there was a significant negative relationship between the APACHE-II score and the BFI and three clinical criteria scores in patients admitted to the ICU, in which the higher the APACHE-II score, the lower the scores of BFI and three clinical criteria. Investigating the literature, few studies were found to be similar to the present study. Based on the results of this study, a significant inverse relationship was found between the APACHE-II score and the four criteria of RASS, GCS, BFI, and FOUR score. Guler et al. (23) showed a negative correlation between GCS and APACHE-II in patients with acute renal failure. Temiz (24) reported a correlation of 0.85 between these two variables in patients undergoing neurosurgery. The two systems are currently used jointly to measure the ICU patients’ status. However, APACHE-II also includes the patient's major physiological parameters. Since the GCS index is one of the components of the APACHE-II score, the correlation between these two indices is expectable. Temiz (24), in his study of neurosurgical intensive care unit (NICU) patients showed that the correlation between APACHE-II and FOUR score was 0.85, and the evaluation results showed that compatibility between the FOUR score, GCS, and APACHE-II was high. The FOUR score uses minimum items to evaluate a patient with altered consciousness. This criterion includes important information, which cannot be evaluated by the GCS scale, including the brainstem reflexes, e.g., by determining eye-opening, blinking, and tracking, a broad spectrum of motor responses, and the presence of abnormal breath rhythms.
Unlike the study by Yaman et al. in 2010, which only examined the APACHE-II score in patients (1), in the present study, not only the correlation of the APACHE-II score (significant negative relationship) with BFI and the three criteria scores was proven but also the effect of APACHE-II score on the correlation of BFI with the three clinical criteria was investigated, which showed this correlation increased with increasing APACHE-II score (patient’s condition deteriorating). Three other variables for ICU patients, including arterial blood oxygen saturation (SpO2), mean arterial pressure (MAP), and sedative drug use, were also considered in our study; however, none of them was shown to affect the correlation between the BFI criterion and the three clinical criteria.
Although our study is consistent with the studies by Guler et al. (23), Lueskel et al. (20), Temiz et al. (24), and other studies, the unique aspects of this study that distinguish it from other research are as follows: (1) the statistical population was high, with three records from each of the 85 hospitalized patients in the ICU with all variables (255 records in total); (2) three common and important clinical criteria were considered simultaneously; (3) not only the correlation between BFI and clinical criteria was demonstrated but also the influence of various components such as age, sex, mechanical ventilation, sedative drugs, MAP, SpO2, and APACHE-II score was investigated on this correlation; and (4) a wide range of patients were studied because the ICU of Valiasr hospital is a medical ICU, where most elderly patients with multiple comorbidities are hospitalized, and a wide range of medications are prescribed for them, while the ICU of Imam Reza hospital is a surgical ICU, where younger patients and trauma patients are mostly admitted.
Generally, objective criteria for assessing the level of consciousness such as BFI are sufficiently accurate. Thus, BFI can be used instead of using less objective clinical criteria that may not be properly evaluated and may be overestimated or underestimated due to differences in the examiners’ judgments.
5.1. Conclusions
In future studies, it is suggested to examine the underlying disease type and its effect on the correlation between BFI and the three clinical criteria more closely. It is also recommended to conduct similar research on other clinical criteria for assessing the level of consciousness, such as
Ramsy Sedation Scale and confusion assessment method for the intensive care unit (CAM-ICU).