1. Background
Thoracic disc hernias, with a prevalence of 1 in 1,000,000 are uncommon diseases in the thoracic spine, with the highest incidence occurring in the lower thoracic discs (T11-T12) (1-3). Most thoracic hernias are asymptomatic. The most common symptoms are radicular pain and myelopathy, seen in up to 30% of patients aged 40 to 60 (4). Surgery is the treatment choice in symptomatic patients unresponsive to supportive therapies or with progressive neurological symptoms or spinal cord compression and myelopathy (2, 5-7).
Surgical treatments mainly differ in their anatomical approaches. These approaches include a posterolateral approach (i.e., modified transfacet and transpedicular), lateral approach (i.e., costotransversectomy), and an anterior approach (i.e., transpleural thoracotomy, thoracoscopy, mini-thoracotomy with retropleural variation) (2). One of the significant challenges in treating patients with thoracic disc herniation is choosing the best surgical approach. There is no consensus on determining the most advantageous surgical method, and therefore choosing the proper surgical approach is coming to a decision by a physician. The physician usually decides based on the hernia’s location and size, the degree of its calcification, comorbidities of the patient, and also their clinical judgment (4, 8-11).
The classic approach in the treatment of thoracic hernias is the anterior transthoracic approach. In this approach, the surgeon accesses the anterior vertebrae and disc by opening the chest wall through the ribs in a lateral position utilizing unilateral pulmonary intubation (12). Generally, in the transthoracic approach to the spine, morbidity and postoperative complications are higher than in other surgical approaches for treating thoracic hernias (4, 13-15).
The modified transfacet approach is one surgical method for treating thoracic hernias, which was introduced by Stillerman et al. in 1995 on cadaver subjects (16). In this method, Stillerman et al. gained full access to the disc with minor tissue damage without removing the pedicle and posterior part of the ribs (16). After that, surgeons performed several studies to evaluate this method. The effectiveness of this method in the surgery of simple and central discs and even oversized and calcified discs were assessed, yielding satisfactory results. The advantages of this method are less tissue and bone incision, shorter operation length, and minor bleeding compared to other conventional surgical methods (1, 3, 8).
This study retrospectively compares the posterior transfacet method and the anterior transthoracic method in a single medical institution to determine if there is a difference between these two methods regarding their outcomes and complications.
2. Methods
2.1. Study Design and Participants
A retrospective case-series study was performed on patients with thoracic disc herniation (TDH) treated surgically in a single tertiary medical center from October 2015 to June 2019. The hospital ethics department approved this study. Patients diagnosed with TDH (based on the clinical and imaging findings) who did not respond to the non-surgical treatment were included in the study. Patients with other types of spinal diseases or a history of previous spinal surgery were excluded. Two surgeons operated on the patients, and each used a different method. One surgeon treated the patients using the transthoracic method, and the other surgeon performed the modified transfacet pedicle-sparing approach.
2.2. Surgical Procedure
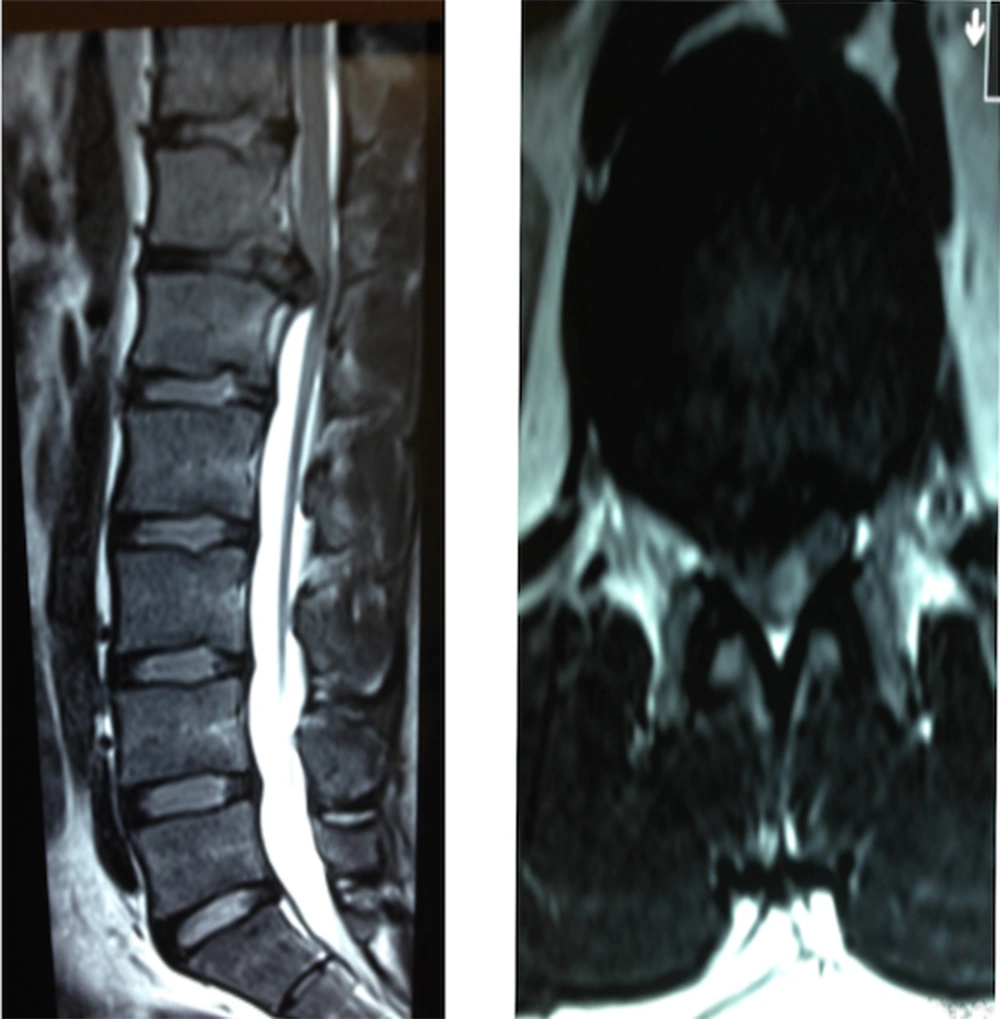
Trans-thoracic or anterior approach for lower thoracic and thoracolumbar region left side approach was chosen. Patient positioned in the lateral recumbent with left side facing upward. In thoracic cases, a surgical incision was placed two ribs above the affected disc. In thoracolumbar cases, a skin incision was placed on the 10th rib. After incising the thoracic skin rib was removed, the vertebra exposed by transpleural approach was removed in the thoracic region, and in the thoracolumbar region, the vertebra was reached retroperitoneally. Then, the disc was incised laterally, and bulged segments of the disc were removed carefully, osteophytes, if present, were removed by small Kerrison Rongeurs, and the spinal cord was decompressed (Figure 1).
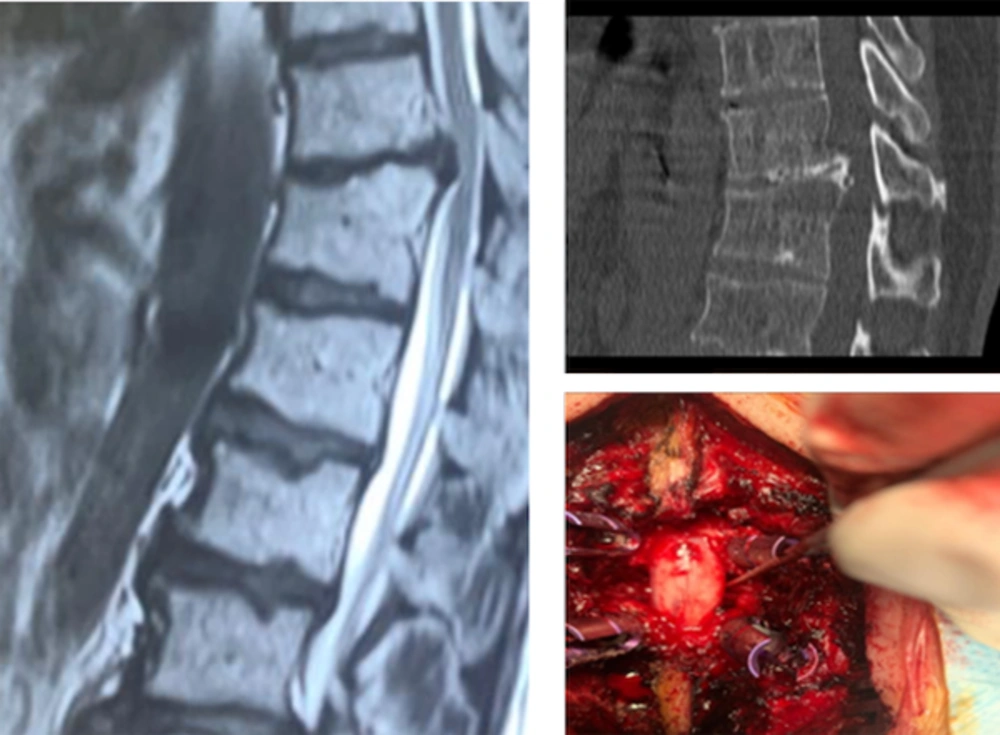
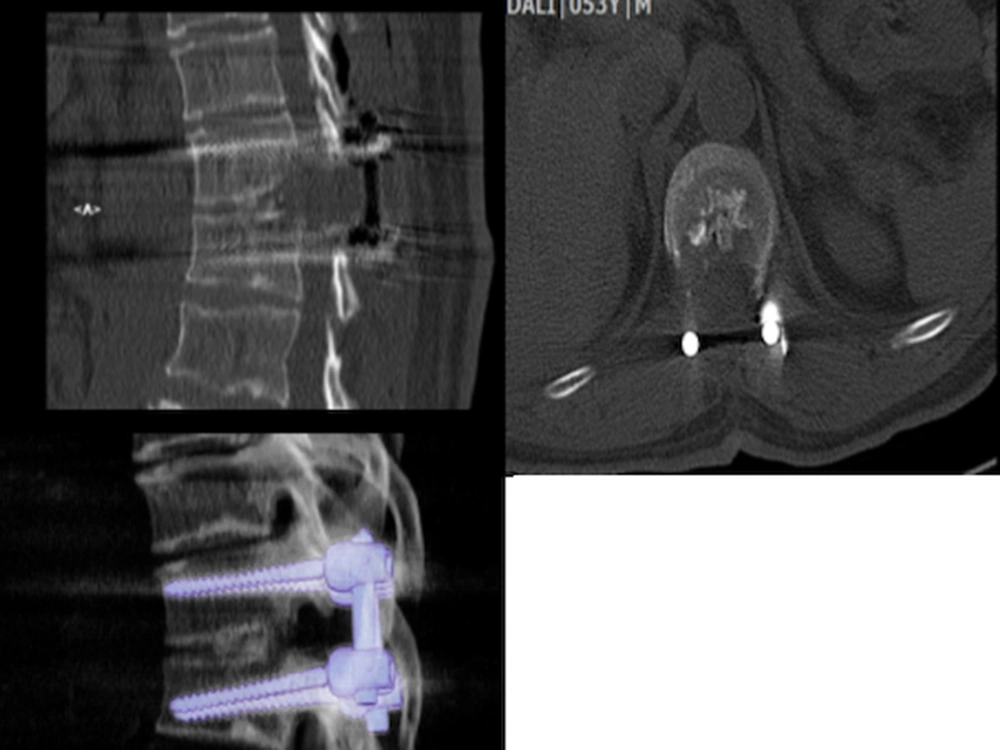
The posterior transfacet approach was made by a posterior midline incision. Muscles were elevated subperiosteally, and the affected disc was confirmed by intra-operative C-arm radiographs. Laminectomy was done, and then the facets were removed bilaterally. The disc was extracted carefully from the posterior. A special curved curette was used to break the central calcified portion into the disc space for removing a calcified disc. After complete discectomy, pedicle screws were inserted in vertebrae above and below, and posterior spinal fusion was achieved with autografts from laminectomy bony particles (Figures 2 and 3).
A 53-year-old patient presented with radiculopathy and myelopathy. The left image shows sagittal magnetic resonance imaging of the patient with T11 and T12 thoracic disc herniation. The right upper image shows the sagittal CT scan of the calcified disc. The right lower image shows the surgery site during the posterior transfacet discectomy (both facets are removed, and the curette shows the disc space).
The postoperative images of the same patient in Figure 2. The right upper image shows the sagittal images of CT scan. The left image shows the axial CT scan of the patient and the removed calcified disc. The right lower image shows the pedicle screws and the removed disc.
2.3. Data Gathering and Evaluating Tools
Pre-operative data, including demographic data, clinical symptoms (such as pain, urinary, and bowel symptoms), and Frankel’s score, were recorded for all patients. All patients underwent pre-operative magnetic resonance imaging (MRI) of the thoracic vertebrae (T1-T12); radiologists and surgeons interpreted these results. The operation information (i.e., bleeding, duration of surgery, and complications) was also recorded. Six months after the surgery, all patients were evaluated for their clinical symptoms, Frankel’s Score, and Visual Along Scale (VAS) Score. The patients also filled Short-Form Health Survey (SF-36) Questionnaire and the spine functional index (SFI) in their follow-ups.
In 1969, Frankel et al. cited in Cutler et al. used a grading system to assess spinal cord function in spinal cord injuries (17). Frankel’s criteria are classified into five grades, ranging from A (Complete neurological injury) to E (Normal motor function) (17-19). Moreover, VAS Score is a graphic rating scale for pain assessment with endpoint limits ranging from 0 (no pain) to 10 (the much pain as possible). The SF-36 questionnaire is the most comprehensive tool, in public health assessment of the quality of life, at the international level. It includes 36 questions that measure eight parts: Physical functioning, role physical, pain, general health, vitality, social functioning, emotional role, and mental health. Each section has a score between 0 to 100. A score of zero is the lowest score that indicates the most disability, and as the numbers increase, the amount of disability decreases, so the number 100 indicates no disability (20, 21). Also, SFI is the criterion for whole-spine examination that the patient answers. It is supposed to be an efficient way to examine the outcomes after spine surgery, which also has a lower response error rate (22).
2.4. Outcomes
The improvement in Frankel’s score was considered the primary outcome. Differences between the two groups regarding VAS score, SF-36 questionnaire, and also complications of the surgery were studied as the secondary outcomes.
3. Results
Of a total of 23 patients who underwent surgery, four patients were excluded from the study (one patient did not complete the follow-up sessions, one had a hip fracture after the surgery, one patient had two-level thoracic disc herniation, and one had another disc herniation in the lumbar region). Eleven patients (six males, five females) with a mean age of 46.1 years (SD = 11.64) underwent a transthoracic approach. Eight patients (six males, two females) with a mean age of 47.3 years (SD = 10.58) had a posterior transfacet pedicle sparing approach. In the transthoracic group, one patient had T5-T6 disc herniation, one had T9-T10, three had T10-T11, five had T11-T12, and one had T12-L1 disc herniation. In the transfacet pedicle sparing approach, one had T7-T8, one had T9-T10, one had T10-T11, and five had T11-T12 disc herniation. The urinary and bowel symptoms were present in six patients in the first group and five patients in the second group. The mean VAS score before the surgery was 3.36 (SD = 2.5) and 3 (SD = 2.8), respectively. Mean blood loss was 912 mL (SD = 117) and 387 mL (SD = 134) in the transthoracic and transfacet groups, respectively.
The Frankel’s score improved at least one score in ten patients from the transthoracic group and seven patients from the transfacet pedicle-sparing group. Also, the urinary and bowel symptoms resolved after the surgery in all patients except one patient from the second group. Moreover, we found no significant difference between the two groups concerning SFI (mean = 71 (SD = 28.3), and 61 (SD = 38.0), respectively). As shown in Table 1, there was no significant difference between the two groups regarding the SF-36 questionnaire. There was no infection detected in any group.
| Short-Form Health Survey Questionnaire Score | Trans-thoracic Approach | Trans-facet Pedicle Sparing Approach | P-Value |
|---|---|---|---|
| Physical functioning | 61.8 ± 38.35 | 51.2 ± 42 | 0.492 |
| Role limitation due to physical health | 63.63 ± 46.58 | 75.00 ± 46.29 | 0.600 |
| Role limitation due to emotional health | 81.81 ± 40.45 | 81.62 ± 37.83 | 0.904 |
| Energy/fatigue | 65.68 ± 17.6 | 59.37 ± 14.5 | 0.395 |
| Emotional well-being | 69.81 ± 17.28 | 66.00 ± 16.00 | 0.657 |
| Social functioning | 80.68 ± 23.95 | 75.00 ± 24.09 | 0.657 |
| Pain | 71.59 ± 29.33 | 81.25 ± 18.02 | 0.657 |
| General health | 74.50 ± 19.77 | 64.50 ± 21.56 | 0.238 |
a Values are expressed as mean ± SD.
4. Discussion
Thoracic disc herniation (TDH) is a rare condition that could present with radicular pain and myelopathy. Several surgical approaches are trying to relieve these symptoms and improve these patients’ quality of life; however, there is no consensus on this subject. One of these methods is the transthoracic approach, which is supposed to provide an enhanced view and better access to the spinal canal’s ventral part. This method, however, has its own potential complications, mainly due to the manipulation of thorax components during the surgery. On the other hand, posterior approaches usually do not influence the chest components and are more familiar with spine surgeons. They have less but adequate access to the ventral part of the spinal canal, which is the main area compressed by a herniated disc. The lateral components (part of rib, pedicle, and facet) should be resected to access the disc without retracting the spine and causing spinal cord injury. In the transfacet posterior approach, only the facet adjacent to the disc is resected. This method could make the spine unstable and make instrumental fixation required.
In this case series study, we compared the possible differences between the two surgical methods in patients with TDH. As mentioned before, the results showed that the transfacet pedicle-sparing approach and transthoracic approach have similar outcomes. The latter statement was compatible with our hypothesis. It also suggests that the transfacet pedicle-sparing method can be used to treat herniated thoracic discs with improved safety and decreased number of complications.
In a study performed by Black, seven patients underwent a similar method of surgery (11). This study showed that the posterolateral transfacet pedicle-sparing approach could be an effective and safe technique for treating TDH (11). Bransford et al. studied eighteen consecutive patients with TDH (7). All of these patients were operated on using the modified transfacet pedicle-sparing technique in addition to short segmental fusion. They suggested this method as a safe way to improve patients’ symptoms (7). In another study, sixteen patients with symptomatic TDH were operated on with a combination of posterior transfacet pedicle-sparing approach and real-time intraoperative ultrasound. All patients had improvements after the surgery and during the follow-ups. The authors also suggested this combination to reach a higher safety level during the surgery (23). Carr et al. reported fifty-one consecutive patients with TDH who underwent surgery with a modified transfacet pedicle-sparing approach (1). The patients’ symptoms improved after the surgery and during the follow-ups regarding VAS score, American spinal injury association impairment scale, as well as Nurick grade (1).
Our study was in accordance with these previous studies, demonstrating the satisfying efficacy and safety of the modified transfacet pedicle-sparing method compared to the transthoracic approach. Both of these methods increased SFI and Frankel’s scores and improved patients’ quality of life. This study suggests that these surgical methods can be chosen considering the following items; patient’s comorbidities, especially low cardiopulmonary reserve, location of the herniated disc and its calcification, and maybe most importantly, experience and skill of the surgeon.
The main limitations of this study are that surgeries were performed by two different surgeons and a relatively small sample size, which negatively affected the reliability of the results. However, they revealed that the two methods were comparable but increasing the power of the study was not possible due to the rarity of patients undergoing surgery due to TDH. Further investigations with a higher number of subjects can examine the correctness of these results. Also, systematic reviews that add up all similar articles can reach a comprehensive recommendation for treating TDH. Other limitations were the lack of access to patients for follow-up and the retrospective design of the study, which was also because of the small number of patients.
4.1. Conclusions
However, the posterior transfacet approach and transthoracic method yielded similar results in our study, but it is challenging to extract definite conclusions due to the small sample size.