1. Background
The estimated annual global incidence of spinal cord injury (SCI) is about 23 cases per million populations (1), while this is about 72.4 per million in Iran (2). The high prevalence of this devastating injury, in addition to sensory and motor disorders, leads to several complications, including physical, psychological, and social issues. In addition to causing readmission and imposing high costs on the health system and patients, these complications affect patients' quality of life and lead to mortality. The results of many studies have emphasized the need to follow up and implement long-term care after discharge from the hospital and at home to prevent and treat secondary complications (3).
However, according to the evidence, despite the care to prevent and treat these problems, these complications are not well controlled and still have a high prevalence. One of the causes can be providing care without considering the deep knowledge of patients' real needs and concerns (4). A review of the literature in this field shows that limited studies have evaluated the actual perception and experience of SCI patients and their care needs. Madasa et al. reported that the most common physical complications of SCI patients were urinary tract infections, pain, and pressure injury (5). The results of a study in Washington also showed that patients suffered from urinary tract infections (62%), pressure injury (41%), and constipation (33%) (6).
In addition to physical problems, SCI patients are significantly more prone to psychological complications than healthy individuals. Moreno et al. showed that 17% - 25% of SCI patients had psychological disorders, of whom 18% - 37% suffered from depression (7). Other studies have pointed out the importance of paying attention to the care and treatment of psychological disorders in SCI patients (8).
Considering the high prevalence of physical and psychological complications in SCI patients, which has led to increased readmission rates and reduced quality of life, it is necessary that rehabilitation team members provide planned care based on the patient's actual needs (9). However, effective care requires deep awareness and insight into the challenges and needs of these patients and their professional caregivers in real life (10).
2. Objectives
A comprehensive understanding of people's experiences of problems and care needs requires deep and extensive investigation through qualitative research. Thus, this study was conducted to identify and effectively meet SCI patients’ and rehabilitation team members’ physical and psychological care needs.
3. Methods
3.1. Study Design
This study used a qualitative content analysis approach to explain SCI patients’ physical and psychological care needs.
The study population included all SCI patients selected from SCI associations in Tehran and Bam, Iran. Rehabilitation team members included a physiotherapist, a social worker, an occupational therapist, a rehabilitation specialist, a general physician, a nurse, a psychologist, and a sexologist. Purposeful sampling was continued with maximum diversity (age, sex, type of injury, and duration of SCI) until data saturation was reached.
3.2. Inclusion and Exclusion Criteria
3.2.1. Inclusion Criteria
Inclusion criteria were all traffic injured and earthquake victims with SC, paraplegia and tetraplegia SCI diagnosed by a specialist, communicating ability, 18 years of age or older, signed informed consent forms, at least one year of SCI care experience for caregivers.
3.2.2. Exclusion Criteria
The exclusion criteria included unwillingness to participate in the study and traumatic brain injury.
3.3. Data Collection
3.3.1. Demographic Characteristics
After prior telephone coordination, obtaining permission from the participants to interview and participate in the study, and setting an appointment, the researcher visited the mentioned centers at a specified time.
3.4. Method
In this study, semi-structured interviews were used to collect information. Each interview with the patient began with a general question: "Can you tell us about your experiences with this serious injury?" Then, they were asked to "share their experiences of challenges and care needs they had after SCI". The rehabilitation team members were asked to "describe their experience of caring for these patients" or "describe what care patients need at home". Data collection lasted 14 months. The duration of the interviews varied between 30 - 45 minutes. The first researcher performed the interviews and recorded them on a tape recorder. Then, verbatim transcription and continuous comparative analysis were done.
3.5. Data Analysis
The conventional content analysis was used for data analysis. Simultaneously with data collection, the analysis was performed according to the five-step Graneheim and Lundman method (11) as follows: First, the interviews were transcribed immediately after each interview, and then transcripts were read several times. The initial codes were extracted, and then the codes were merged and classified based on their similarities. Finally, the concept and content hidden in the data were extracted.
Goba and Lincoln's (1994) criteria were used for data trustworthiness, including credibility, dependability, confirmability, and transferability (12). The research team had a long-term relationship that helped gain the participants' trust and understand the study environment. The participants were asked to review and verify the data and codes. After coding, the interview transcripts were returned to the participants to ensure the accuracy of the codes and interpretations, and codes not reflecting the participants' views were corrected. Also, we included diverse participants in terms of age, type of injury, occupation, sex, level of education, and caregivers. Supervisors specialized in qualitative research reviewed the interview transcripts and the extracted codes and classes and reached a high agreement regarding the extracted results.
3.6. Ethical Considerations
The Tehran University of Medical Sciences Ethics Committee approved the study (IR.TUMS.FNM.REC.1398.141). Before the interviews, the participants were informed about the study's objectives and methods.
4. Results
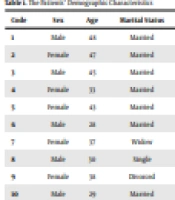
The findings of this study were based on interviews with 24 participants to achieve data saturation. The participants' demographic characteristics are presented in Tables 1 and 2. The results of data analysis led to the identification of two main categories of physical and psychological care needs.
| Code | Sex | Age | Marital Status | Employment | Type of Spinal Cord Injury | Duration of Spinal Cord Injury |
|---|---|---|---|---|---|---|
| 1 | Male | 48 | Married | Teacher | Paraplegia | 18 |
| 2 | Female | 47 | Married | Houseworker | Paraplegia | 18 |
| 3 | Male | 45 | Married | Unemployed | Paraplegia | 18 |
| 4 | Female | 33 | Married | Houseworker | Paraplegia | 18 |
| 5 | Female | 43 | Married | Unemployed | Tetraplegia | 18 |
| 6 | Male | 28 | Married | Unemployed | Paraplegia | 6 |
| 7 | Female | 37 | Widow | Unemployed | Paraplegia | 18 |
| 8 | Male | 30 | Single | Unemployed | Tetraplegia | 8 |
| 9 | Female | 38 | Divorced | Unemployed | Tetraplegia | 5 |
| 10 | Male | 29 | Married | Houseworker | Paraplegia | 3 |
| Code | Sex | Education | Major | Employment Experience |
|---|---|---|---|---|
| 11 | Female | Bachelor | Social worker | 10 |
| 12 | Male | Bachelor | Physiotherapist | 12 |
| 13 | Female | Bachelor | Occupational therapist | 9 |
| 14 | Female | Bachelor | Occupational therapist | 13 |
| 15 | Male | Master of science | Occupational therapist | 8 |
| 16 | Female | Ph. D. | General physician | 6 |
| 17 | Female | Specialist | Rehabilitation specialist | 10 |
| 18 | Female | Ph. D. | Nurse | 10 |
| 19 | Female | Master of science | Nurse | 12 |
| 20 | Male | Master of science | Psychologist | 5 |
| 21 | Female | Master of science | Psychologist | 10 |
| 22 | Female | Ph. D. | Sexologist | 20 |
| 23 | Female | Ph. D. | Sexologist | 7 |
| 24 | Female | Bachelor | Staff of the welfare organization | 10 |
4.1. Physical Care Needs
One of the main aspects of this study was the need for physical care, which has several sub-categories, including care for skin, gastrointestinal, urinary, and musculoskeletal problems.
4.1.1. Skin Problems
The participants suffered from skin problems in the form of pressure injury and burns. Immobility is an influential factor in the incidence of pressure injury, which is a consequence of the caregiver's inability to change the patient's position and lack of patient knowledge. In this regard, a 45-year-old man with paraplegia caused by an earthquake said:
"... After I was discharged from Tehran hospital ... During this time, my wife took care of me. She was also injured in the earthquake, and couldn’t move me, we did not have anyone else, ... " I got a pressure injury." (Code 3)
In the present study, the participants stated that the inability to provide adequate equipment to prevent and treat pressure injury such as alternating pressure mattresses, dressings, standard wheelchairs, and the inability to pay for appropriate treatments, caused them serious problems. In this regard, a caseworker said:
"Because of the rising price of wheelchairs, patients cannot afford to buy high-quality wheelchairs, so they have to buy non-standard and second-hand wheelchairs, which cause pressure injury." (Code 11)
Burns were another skin problem, mostly caused by the patients' lack of knowledge about sensory dysfunction, especially in the early stages of the disease. A married man suffering from a paraplegic lesion for 18 years said:
"For the first time, after SCI, we went on a picnic. My friends had made a fire. We sat around the fire. When I got home, I realized that my legs were burned, but I did not notice.”
4.1.2. Gastrointestinal Problems
The patients experienced gastrointestinal problems in the form of fecal incontinence and constipation. According to the data, fecal incontinence caused skin disorders, social isolation, occupational difficulties, and depression in the patients and even affected their patients' sex lives. People with this problem avoided attending meetings and became isolated. In this regard, a 29-year-old married man stated:
"Before this disease, I was a very social person, but this disease has made me stay at home for fear of being disgraced because of my bowel incontinence ..." (Code 10)
According to the present study, non-compliance with a bowel-training program due to impatience and lack of knowledge were mentioned as causes of constipation and fecal incontinence. For example, a nurse with ten years of experience said:
"A bowel training program prevents constipation and accumulation of feces. I had patients who did not suffer from constipation because of following this program regularly and having a proper diet, but some do not compliance. They do not care at all." (Code 18)
4.1.3. Urinary Problems
Urinary problems in patients appeared in the form of urinary tract infection, urinary retention, and urinary incontinence. Urinary tract infection was the most common complaint that the patients attributed to frequent hospitalizations. According to the data, the causes of this complication were lack of caregivers, exhaustion of caregivers, and lack of catheterization knowledge. The results showed that other causes of urinary tract infection were lack of equipment and unsuitable environments for catheterization. According to the patients, unsanitary and small toilets made it impossible for them to follow the hygiene tips during catheterization. Financial problems also forced the patients to use catheters and bladders for extended periods, leading to urinary tract infections.
In this regard, a nurse with 12 years of experience stated:
"Once we visited one of the client's houses in a slum, the patient suffered from urinary tract infection, the house toilet was very small, and the health conditions were poor; Nelaton catheter was also kept in a contaminated environment, which was a factor for infection." (Code 19)
Another problem was urinary incontinence, which had a negative effect on psychological, social, and sexual aspects, leading to a decrease in the patients' quality of life. Some caregivers believed that patients' lack of intermittent catheterization was a cause of incontinence. A caseworker stated:
"Most patients often can adapt with disabilities; however, they cannot adapt with urinary incontinence, and this problem bothers them a lot because it affects many aspects of their lives, sexual, social, and occupational issues." (Code 11)
4.1.4. Musculoskeletal Problems
Shoulder pain and pain caused by muscle spasms were frequently experienced by the patients, affecting their quality of life and making life more difficult for them. These people depend on their shoulders to perform many daily activities, especially pushing a wheelchair. Therefore, pain in this area can significantly impact their ability to perform daily activities. For example, a 47-year-old paraplegic patient with an 18-year history of the disease stated:
"Some nights, I cannot sleep because of pain, it is very annoying, it is worse when I have shoulder pain and I can no longer push my wheelchair and do housework, so I have to be in bed all the time." (Code 2)
4.2. Psychological Care Needs
4.2.1. Isolation
According to the quotes, factors such as lack of proper urban facilities, a shortage of caregivers, pity, and addiction led to the isolation of the patients.
Lack of proper urban facilities was a concern for almost all the participants, making it difficult for them to move independently outside the house. In this regard, a single man with paraplegia stated:
"I cannot go out alone, even to the neighborhood park, there are too many stairs that I cannot go at all, someone must be with me. I only have an old mother and father who cannot come with me, so I do not leave the house anymore. " (Code 8)
Another reason for the isolation of the patients was addiction. After becoming addicted, patients lose their desire for social interactions and become dissociable.
4.2.2. Lack of Adaptation in Patients with Spinal Injuries
Most of the participants acknowledged their inadequate knowledge about SCI, coping strategies, and how to live after the injury. They considered this lack of knowledge an effective barrier to their adaptation. Another obstacle to achieving adjustment was giving the patient false hope about recovery. Caregivers noted that giving false hope by the rehabilitation team made the accepting process more difficult for the patients and emphasized that the rehabilitation team should consider this more seriously. Lack of adaptation to the living environment was another problem for the patients to adapt and return to daily activities. Data showed that the patients wanted to return to society after adjusting to their illness; although, the conditions and infrastructure in their living environment were an obstacle.
For example, a 48-year-old man suffering from paraplegia for 18 years said:
"At first I did not understand what had happened to me. Like a small child for whom something has happened, but the child does not understand, I did not know my illness. On the first days, something like this happened to me. I did not understand what I should do, how I should cope with this disability and live with it." (Code 1)
Another participant, a 33-year-old female patient suffering from paraplegia for 18 years, said:
"After a long time, when my mental health improved, I decided to go shopping like before my illness, but there was no suitable space for wheelchairs in the city and shops. I used to go shopping on foot. Now I accept this with a wheelchair, but when it is not possible to go with a wheelchair, many places are not suitable; what should we do?" (Code 4)
4.2.3. Addiction
Lack of counseling and insufficient knowledge about strategies to deal with mental (low self-esteem), physical (chronic pain), sexual (premature ejaculation), social (lack of jobs), and financial issues can be risk factors for addiction.
A 29-year-old man suffering from paraplegia for three years stated:
"I could not cope with my disability; I could not believe that I could not walk anymore, I was under a lot of pressure, so I became addicted to calm myself down." (Code 10)
Another cause of the patients' tendency to drug abuse was lack of proper employment, leading to financial problems. This prevented one from appearing as a successful and authoritative person in the family and society, causing them to face severe psychological issues. Consequently, they chose drug abuse as a relief.
For example, one of the patients, a 28-year-old man suffering from paraplegia for six years, said:
"Before I was disabled, I was a masonry, I could afford my living expenses, but after that I am always in the house. It is very difficult to be a man at home and cannot make money for his wife and children, I feel bad when my wife has to be the breadwinner. How can I work when I am paralyzed?"
Another factor mentioned by the participants was the use of opium to delay ejaculation. Premature ejaculation is a sexual disorder experienced by some of the patients. The patients were looking for a way to deal with this complication. However, due to lack of sexual counseling and training, they used wrong methods such as opium use to solve this problem and eventually become addicted.
5. Discussion
The patients' immobility due to lack of proper caregiving and inadequate knowledge led to a high prevalence of pressure injury in them. This problem may be due to the patients' limited access to home health care services to provide education and care after discharge from the hospital. As in Eslami et al.'s study, one of the important reasons for the high prevalence of pressure injury in these patients was lack of home health care services after hospital discharge (13). According to some studies, home health care services in Iran face challenges, one of the most important of which is lack of insurance coverage, limiting access to such services. Other problems in providing home health care services include flawed policy and lack of guidelines (14, 15). However, measures have already been taken, including defining such services and implementing them as pilot projects in several cities. However, there are still significant differences in home health care standards between Iran and other countries (16).
Other factors included limiting patients' access to protective equipment, as found by Sleight et al. (17). They reported that lack of institutional support and patients' financial inability were the causes of limited access to equipment. Although the Welfare Organization in Iran has taken steps to provide necessary equipment, an inadequate budget and high costs of standard equipment have remained among its main concerns. This is in line with the results of a 2012 study by Burns and O’Connell (18).
Another finding was the refusal of the patients to follow the healing process of pressure injury due to the high cost of treatment. According to the participants, they had to follow their treatment at private clinics since public hospitals provided limited services due to the long-term treatment of pressure injury and yet they could not afford private treatment. In this regard, Stroupe et al. reported that pressure injury was one of the costliest complications of the disease (19). Home health care services can prevent this costly complication, which is one of the main causes of patient mortality, and shorten the length of hospital stay, resulting in reduced costs for the health system and the patient (20).
Urinary and fecal incontinence were other physical challenges that led to social, sexual, and psychological disorders. Other studies have also indicated adverse effects of these complications on patients' quality of life (21-23). The participants mentioned a bowel and bladder training program as a way to prevent these problems. A review of studies examining bladder and bowel management methods showed the effect of this program on reducing these problems (24, 25). However, some of the participants pointed out that they could not comply with the bowel and bladder exercise program due to lack of knowledge and impatience. Thus, the rehabilitation team members needed to plan an exercise to manage this issue.
Another common physical problem was urinary tract infections due to poor hygiene during catheter insertion, non-standard toilets, and long-term use of catheters and urine bags, as mentioned in some other studies (26, 27). Inadequate bathroom surroundings were additionally stated by Burns and O’Connell (18). However, urinary catheters were used for more extended periods, which can be attributed to the limited access to catheters due to the patients’ poor economic status.
Research results described the experience of pain as a distressing problem that negatively affected daily functioning. In this regard, several studies have pointed out the negative relationship between pain intensity and patients' daily activity (28-30).
Isolation was one of the psychological challenges, and poor welfare facilities were identified as one of its contributing factors. Cimino et al. showed that urban structural barriers restricted patients' access to recreational facilities and services and forced them to be isolated at home (31). Therefore, city authorities should adapt urban space to prioritize people with disabilities so they can use urban facilities and enjoy their citizenship rights (32).
The present study's findings introduced the compassionate look at the patient as another factor of isolation. The unpleasant opinions of people and their unnecessary help, due to their bad attitude toward people with disabilities, were so annoying from the patients' point of view that caused their reluctance to participate in social life. This was in line with Hammel et al.'s findings (33). Increasing people's awareness of the abilities of people with disabilities can change society's attitude toward them so that they can take their rightful place in society without being stigmatized (34).
The analysis of the interviews revealed barriers to adaptation to the disease. Lack of knowledge about the disease and how to deal with it, expressed by almost the majority of the participants, was one of the most critical barriers. According to the findings, it was due to lack of appropriate counseling and training. Another obstacle was lack of structural adaptation to the living environment. This is because, without adapted environmental conditions, patients cannot lead a normal life.
Similar to our results, Babamohamadi et al. identified that lack of necessary information about the disease and adaptation methods and patients' lack of access to urban facilities and spaces were the factors of incompatibility (34). Inappropriate urban elements were considered a factor for not participating in social activities (35). Additionally, giving false hope by the rehabilitation team was another issue that led to patients' failure to achieve adaptation, according to Dorsett et al. (36).
Another important finding of this study was to explain the factors of the patients' tendency to addiction. Based on the participants' experiences, lack of knowledge about adaptation strategies and lack of counseling sessions led to drug addiction instead of using practical and scientific strategies. Our findings indicated the importance of counseling and education in the adaptation process. The results of previous studies also showed that patients tended to use drugs as an ineffective coping strategy to accept their disease (37, 38). Similarly, we observed that the patients considered drug abuse as a solution to relieve chronic pain, as confirmed by Smedema and Ebener (39).
The patients also considered drug abuse a defensive method to relieve psychological stress, which is in line with Tetrualt and Courtois findings (40). The present study showed that people used drugs to increase the time of sexual intercourse, as also mentioned by Khammarnia and Peyvand (41). Other factors included economic problems, especially unemployment, causing the patients to use drugs as a means of entertainment and a solution to forget their problems. These results are in line with those of Karimyar Jahromi and Eftekharzadeh (42). Therefore, we suggest psychological counseling and training to deal with these challenges.
5.1. Conclusions
This study identified patients' home health care needs, based on their actual experiences and caregivers, according to the community's economic, social, and cultural conditions. We also emphasize the need for home health care services and the financial support of caregiving organizations. Implementation of such services in the country requires health insurance coverage, guideline preparation, and care standardization. Therefore, it is suggested that health policymakers design effective home health care rehabilitation programs based on the real needs of patients and the conditions of society and eliminate obstacles to implementing such services in the country's health system. The consequence can be improving patients' quality of life and reducing the costs of the health system.
5.2. Limitations
The study's limitation was our inability to interview a sufficient number of family caregivers to achieve data saturation in this group. This limitation means the perspectives of families providing informal care to SCI patients after hospital discharge and at home may be underrepresented in the study findings.