1. Background
Deformity in spine is defined as malalignment in curvature caused by failure of formation and/or separation in one or more segments of spine, more often, it can be idiopathic in nature. Based on patient age and underlying cause, its clinical presentation and radiographic appearance may differ (1). Major causes of deformity include congenital, skeletal-muscular, idiopathic, degenerative, and other causes such as trauma, skeletal dysplasia, and syndromic diseases (2).
The most common spinal deformity is reported to be adolescent idiopathic scoliosis (AIS), seen in young population. Secondary to degenerative disease, adult patients, mostly, present with adult spinal deformity (ASD), with exception to missed AIS during early adulthood (3). The pivotal aim in these patients is restoration of regional and global alignment, although specific goals may differ based on individual patients, such as the need for neurological decompression. One of the most important objective in spinal deformity correction surgery, to improve patient outcome and reduce the risk of junctional failure is to achieve appropriate sagittal alignment (2). Studies have reported that restoration of spino-pelvic parameters such as sagittal vertical axis (SVA), pelvic incidence - lumbar lordosis (PI-LL) mismatch, T1-pelvic angle (TPA), pelvic tilt (PT) and sacral slope (SS) is associated with improved post-operative function and reduce the risk of revision surgery (4).
Development of advanced planning tools have helped in pre-operative planning of spine surgery to achieve desired alignment (5). However, intra-operatively spine surgeons cannot ensure that their plan is accurately executed, despite the available alignment goals. In the operating room, rods are bend manually using French benders, which may cause over or under bending of the rods and lead to malalignment. Biomechanical properties of posterior instrumentation and rod contouring are important factors effecting the patient outcomes (6, 7). Adequate rod contouring is vital for achieving both global and regional target re-alignments, thus, reinforcing the importance of intra-operative rod bending.
Recent studies have reported that inappropriate (over or under) bending of spinal rods can affect the post-operative spino-pelvic alignment, leading to inferior patient outcomes (6).
Identifying the difference between desired bend to achieve proper alignment and the actual bend performed intra-operatively, can provide significant information, impacting the outcomes of the deformity correction surgeries of the spine (8). The purpose of this study was to assess how accurately spine surgeons can bend rods; on two different occasions; first, in-situ on the three-dimensional (3D) printed moulage without knowing the angles and secondly, with desired correction angles.
In recent studies, attention is paid to restoring sagittal balance, especially in 3D deformities, which has many reasons, including improving biomechanics, reducing energy consumption in all situations (standing, walking, and sitting) as well as reducing the risk of segmental degeneration. Furthermore, sagittal imbalance, increases the amount of energy consumed, especially during walking (9). Restoration of proper sagittal balance in spinal deformities require accurate recognition of the extent and location of deformities, and the most important measure to achieve this goal is preoperative planning and executing this plan intra-operatively.
The alignment correction is accomplished using soft tissue refinement along with various bone osteotomies and ultimately the instrumentation (10). Creating an appropriate force to correct and eventually maintain alignment requires a proper device; one of the most widely used are longitudinal rod spindles (7). Rods are bend and applied based on Pre-OP planning, considering the soft tissue condition and curve rigidity. Intra-operativley, the rods are bend manually by-hand using French benders, the actual bend performed by surgeon may differ from what was considered in Pre-OP planning.
2. Objectives
Therefore, the current study aimed at investigating the accuracy and difference of rod bending by surgeons when provided with or without template (3D moulage).
3. Methods
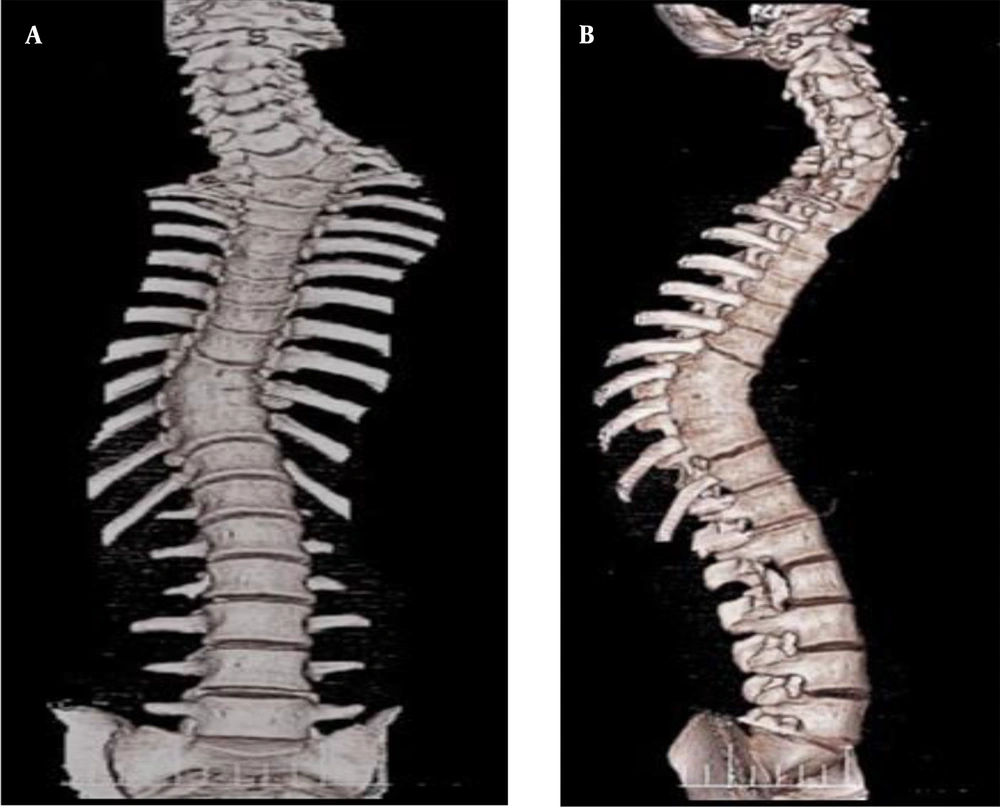
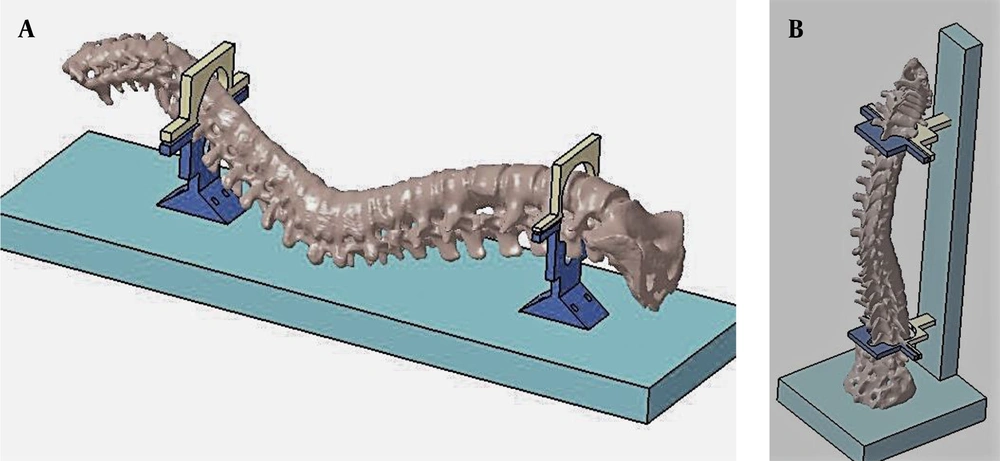
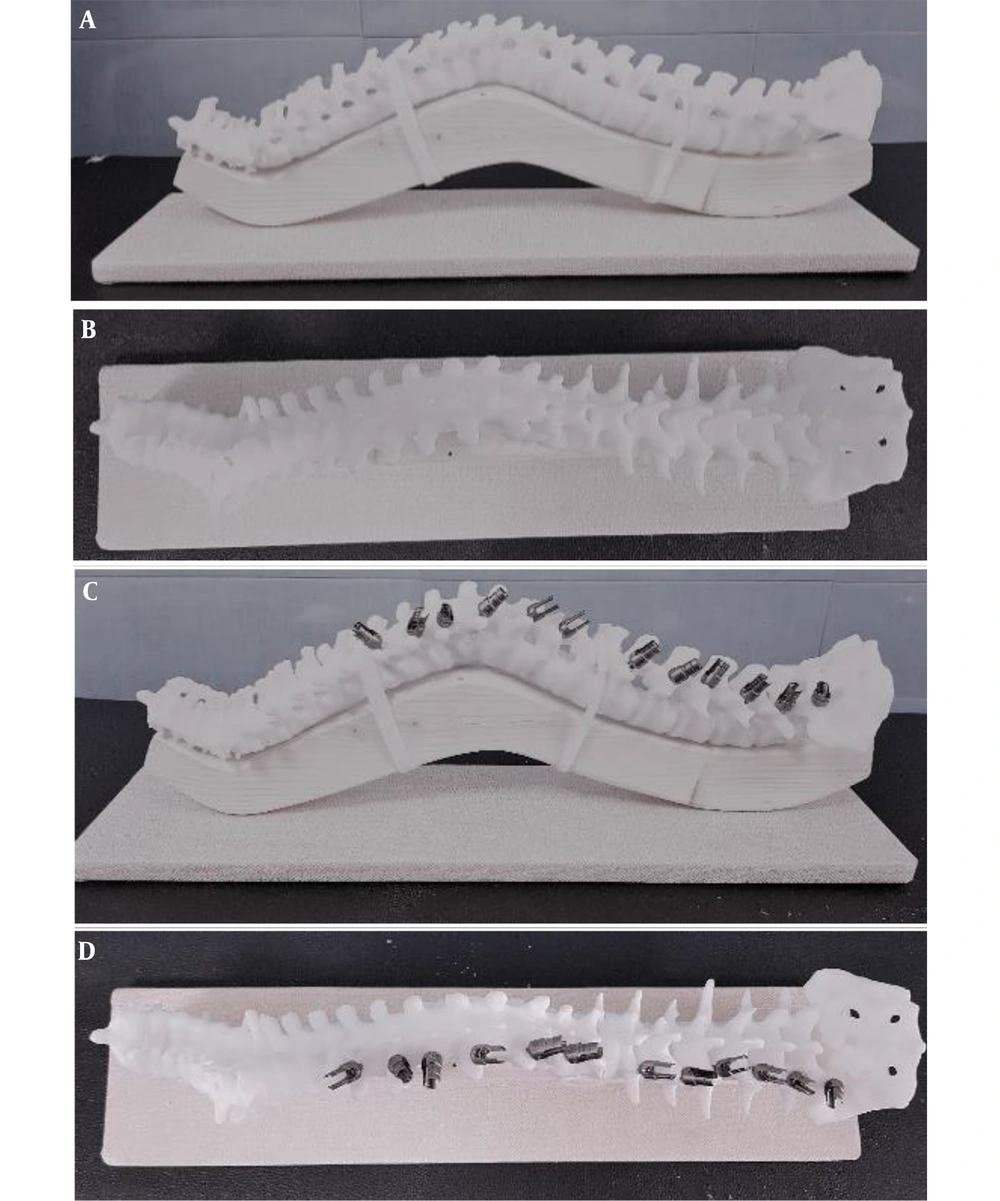
Spine surgeons with minimum 2 years of experience in the field of deformity correction were requested to participate in the study. First, a patient with spinal deformity was selected. Patient was 16 years old male with congenital kyphoscoliosis deformity. The patient was a candidate for correction surgery and routine preoperative examinations were performed. CT scan is routinely obtained for patients undergoing deformity correction surgeries, we had 3D reconstruction of CT scan of this patient on macropacs software (Figure 1). Using 3D-CT scan a schematic moulage was designed on octoprint for windows (Figure 2). 3D printing of moulage was carried out using PLA (polylactic acid) material. Pedicle screws (Zimmer Biomet) were mounted on one side of moulage to stimulae the thoracic and lumbar fixation using Roy-Camille pedicle insertion technique (11). Thus, the moulage was ready as spine representation for rod bending (Figure 3).
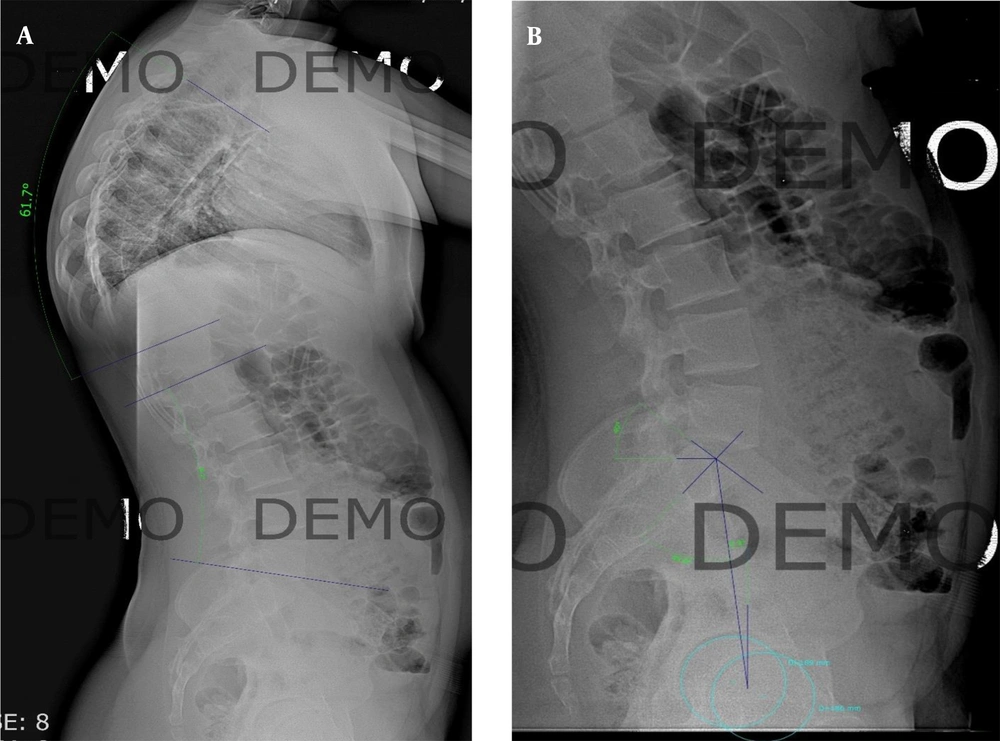
Pre-operative planning and measurements of spinopelvic parameters were performed on digital radiographs (Medicad classic 3.5 demo version). The values obtained were as follows: Lumbar lordosis: 46, thoracic kyphosis: 61, pelvic incidence: 56, sacral slope: 45, and pelvic tilt: 9 (Figure 4). Based on the spinopelvic parameters and Pre-OP planning, the rod should be bent to obtain the necessary correction. For this purpose, surgeons were asked to consider 20 degrees of correction for thoracic kyphosis. Each surgeon was given two rods of same length and thickness (5.5 mm), and they were asked to bend them first regardless of any correction in situ on the moulage and the second rod was asked to be bend with correction of 20 degrees of thoracic kyphosis.
Descriptive statistics were performed using statistical package for the social sciences (SPSS) version 20, rod angles were compared for average and significant differences as well as for error percentage, P-values were calculated using a 2-sample t-tests and P < 0.005 was considered to be statistically significant. Data was presented as mean value + standard deviation. Internal review board approval was not required and patient consent was not indicated, as this study was confined to biomechanical analyses on instruments without involvement of patients, patient material/treatment or animals.
4. Results
Participants of this study were; 21 fellowship trained spine surgeons; including 11 from orthopedics and 10 from neurosurgery specialty. Surgeons were classified according to the experience in spine surgery into two groups of less than five years (42.9%) and over five years (57.1%). The degree of rod bending by surgeons was evaluated on two rods and four curves:
(1) In-situ rod: A, degree of rod bending for thoracic curve (cut-off 61°); B, degree of rod bending for lumbar curve (cut-off 46°).
(2) Correction rod: A, degree of rod bending for thoracic curve (cut-off 40°); B, degree of rod bending for lumbar curve (cut-off 46°).
The analysis was carried out based on the differences in the degree of bending of the rod from the cut-off point. For in-situ rod, mean thoracic and lumbar bend were 65.2 (P = 0.033) and 49.3 (P = 0.077) degrees, respectively and difference from cut-off point were not significant. However, for the correction rod, mean bend in thoracic and lumbar were 53.8 (P = 0.001) and 51.8 (P = 0.004) degrees, respectively, with significant difference from cut-off point (Table 1).
Rod Bending Differences in Lumbar and Thoracic Curves
Each curve was over-bend and it was more pronounce in thoracic, both on in-situ and correction rods, 61.9 and 71.1 %, respectively (Table 2). Relationship between the rod bending and the field specialty and the experience level were analyzed (Table 3). Level of experience showed positive correlation with degree of rod bending more than five years in thoracic in-situ bend (P = 0.003) and thoracic bend with correction (P = 0.004). Degree of rod bending showed correlation with field of specialty as well; with orthopedic in-situ bend (P = 0.002) and with correction (P = 0.003).
| Level | Frequency (%) |
|---|---|
| Thoracic in-situ bend | |
| Over | 13 (61.9) |
| Under | 7 (33.3) |
| No change | 1 (4.8) |
| Thoracic bend with correction | |
| Over | 15 (71.4) |
| Under | 6 (28.6) |
| No change | 0 (0) |
| Field | |
| Orthopedic | 11 (52.4) |
| Neurosurgery | 10 (47.6) |
| Experience | |
| > 5 years | 12 (57.1) |
| < 5 years | 9 (42.9) |
Frequency and Basic Characteristics
Rod Bending Correlation in Thoracic Curve Based on Surgeon Experience and Field
5. Discussion
In recent decade significant research has been performed on the importance of sagittal alignment. There is now substantial evidence that patient outcomes measures and quality of life index correlate with sagittal alignment (12, 13). The progression of malalignment in sagittal plane can compromise the spino-pelvic parameters and propel the body out-of-balance, losing its ability to maintain an upright posture within the cone of economy with minimum energy expenditure (14).
In the present study, most of the surgeons tend to over-bend the rod, irrespective of moulage or angles provided. When spine surgeons were asked to bend the rods without a reference template (3D printed moulage), there was considerable variation in the angles, especially as the target angles decreased for correction. When aiming for 40 and 46 without moulage there were mean differences from the target angles of 13.8 and 5.8, respectively. However, when the surgeons performed in-situ bending on the moulage without knowing the angles, the difference in the angles were less significant and the rod was bend close to the target angles; for 61 and 46 the mean difference was 4.2 and 3.3 degrees respectively. This observation implies that surgeons can perform rod bending close to target, in-situ, without knowing the angles and when no correction is required. The accuracy drops when angles are provided and correction is needed.
Similarly, in their study on accuracy of rod bending, Sardi et al, proved that surgeons have tendency to over-bend the rods when provided with angles (6). However, the accuracy was improved when a spine template was given. Similarly, our study re-inforce this notion that spine surgeon have tendency to over-bend the rods when provided with angles-alone and accuracy improves when a template or moulage is at disposal. These discrepancies between planned curves and the actual achieved angles by bending the rods might be a major contributing factor to junctional kyphosis and hardware failure.
Our study further investigates correlations between surgeon factors and accuracy in rod bending, and a novel correlation was discovered with years in experience and field of practice. Surgeons with more than 5-years of experience showed better accuracy in rod bending. In our opinion this is predictable outcome, as accuracy and outcome improves with surgeon experience. However, another interesting observation that we noted is relationship to field of practice. Fellowship trained orthopedic surgeons showed better accuracy in rod bending and their final bend were closer to target value, when compared with fellowship trained neurosurgeons. This discrepancy can be attributed to the fact that orthopedic surgeons perform more spine instrumentation surgeries than neurosurgeons.
Frequent rod contouring by the surgeon can affect the rod material, eventually leading to several complications including hardware failure. In addition to the biomechanical complications, it may also affect the surgical outcomes (15, 16). These challenges and the importance of restoring the balance of spine captured our attention to focus on problems encountered during contouring of the rod.
Few authors explored the potential of patient specific rod (PSR) implantation technique (17, 18). A proper sized rod is pre-bend based on correction required from Pre-OP planning and then sterilized. The authors report reduced operating time and improved accuracy in rod bending. However, this technique is not yet popular among surgeons, partly due to challenges in logistics. Alternatively, we propose a novel bending instrument, similar to orthopedic plate bender, it can be sterilized and used intra-operatively. Most importantly, this tool should have measurement in-grained so that accurate rod contouring can be performed. In future, we recommend performing biomechanical studies towards the development of such rod bending device.
5.1. Conclusions
Obtaining adequate and matched pre-operative planned alignment remains a challenge for spine surgeons. Surgeons tend to over-bend rods, when given target angles and when correction is needed. However, when provided with template, a 3D printed moulage in our study, accuracy of rod bending improved significantly. The over-bending of the rod can lead to unfovarable patient outcomes with increased risk of junctional kyphosis. Our study warrants that further research is needed to enable surgeons to better execute pre-operative alignment plans.