1. Introduction
Dementia presents with a variety of behavioral and psychiatric disorders, including a range of psychosis, anxiety, depression, behavioral aggression, and delirium (1). However, there are few reports of the occurrence of trichotillomania (TTM) in dementia (2). TTM is a compulsive desire to pull out one's hair; in rare cases, eyelashes or eyebrows may also be affected. Comparing the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (DSM-IV) to the DSM-5, TTM is classified as obsessive-compulsive disorder or related disorder. The feeling of tension immediately before pulling hair out, satisfaction, or relief from pulling out hair was deleted in the DSM-5 (3, 4). Therefore, a patient with dementia who cannot recall or describe a feeling of tension before pulling out hair, or who does not experience pleasure in doing so, may meet these criteria.
According to a recent meta-analysis, TTM has a prevalence of 1.14% of the population, while any hair-pulling behavior has a prevalence of 8.84% (5). TTM has been observed in up to 3.6% of nursing home residents with moderate to severe dementia. The literature on TTM in dementia deals almost exclusively with case reports (2, 6-10) (Table 1). Therefore, it is advisable to further investigate, understand and report the phenomena of TTM in dementia and its relevant cases. This study aimed to report a patient who had developed TTM subsequent to his dementia and review the literature on TTM in dementia case reports.
| Publication Date | Age (y) | Gender | Underlying Disease | Neuroimaging | Treatment | References |
|---|---|---|---|---|---|---|
| 2001 | 67 | Male | - | Mild cerebral atrophy, ischemia in the right hemisphere in white matter, asymmetrical lateral ventricles | Citalopram and Trazodone | Mittal et al. (6) |
| 2011 | 87 | Male | Binswanger’s disease | Periventricular hypodensity and ventricular enlargement | No improvement with any drugs | Caixeta and Lopes (7) |
| 2013 | 79 | Male | Multiple infarcts in the brain | Multiple infarcts in cortical and subcortical regions of the brain | No improvement with any drugs | De Sousa and Mehta (9) |
| 2016 | 54 | Female | Alzheimer’s disease | MRI, Mild generalized atrophy, predominant in the parietal lobe; PET, sever hypometabolism in parietal lobes and the posterior cingulate cortex and bilateral temporal | Quetiapine | Paholpak and Mendez (8) |
| 2018 | 47 | Male | - | sever atrophy of the temporal and frontal lobes, dilatation of the frontal horn with relative preservation of the occipital and parietal lobes | Memantine and Fluoxetine | Issac et al. (2) |
| 2020 | 90 | Female | - | Age-related atrophy of the cerebral cortex | Escitalopram Clonazepam | Sutar et al. (10) |
2. Case Presentation
A 74-year-old male patient was brought by his wife to the psychiatric ward of a university-affiliated hospital in Sari, northeastern Iran, in October 2020. He was a right-handed man with a gradually progressive deterioration of his memory for five years. He was illiterate and a laborer. His problem began after a head trauma that lasted four days in a coma. His family reported that the patient's problems were intensified, and he had problems for a month. At home he was bored and irritable, and talked to himself. He was pessimistic about others and believed that others kept taking his belongings away. He blamed himself for his illness and unemployment. His orientation to place, time, and people was normal. He had no delusion and no suicidal thoughts.
At home, the patient was unable to perform his daily activities independently, and his family reported abandonment of personal interests, neglect of hygiene, a progressive loss of autonomy, and severe apathy.
According to his medical history, he had learning difficulties in childhood and could not do arithmetic. He also had hypothyroidism and was treated with levothyroxine. Due to these disorders, he was exempted from military service. His mother was known to have Alzheimer's disease. On examination, the patient scored 5/20 on the Montreal Cognitive Assessment (MoCA), and had marked difficulties with memory, delayed recall, calculation, attention, abstraction, and language. He was unable to perform executive tasks, search for dots and words, and copy visuospatial figures. Examination of his gait and coordination, reflexes, motor function, cranial nerves, and sensory function revealed no abnormalities.
Five years after the onset of his disease, he developed urinary incontinence, excessive sleep, irrelevant speech, and slow movements, as well as restless and aggressive behavior. Most noticeable was the uncontrolled pulling out of the hairs on his eyebrows. He did not play with the pulled-out hair or eat it. He did not bite his nails or pluck his fingers. Due to his dementia, he could not give a reason for his TTM.
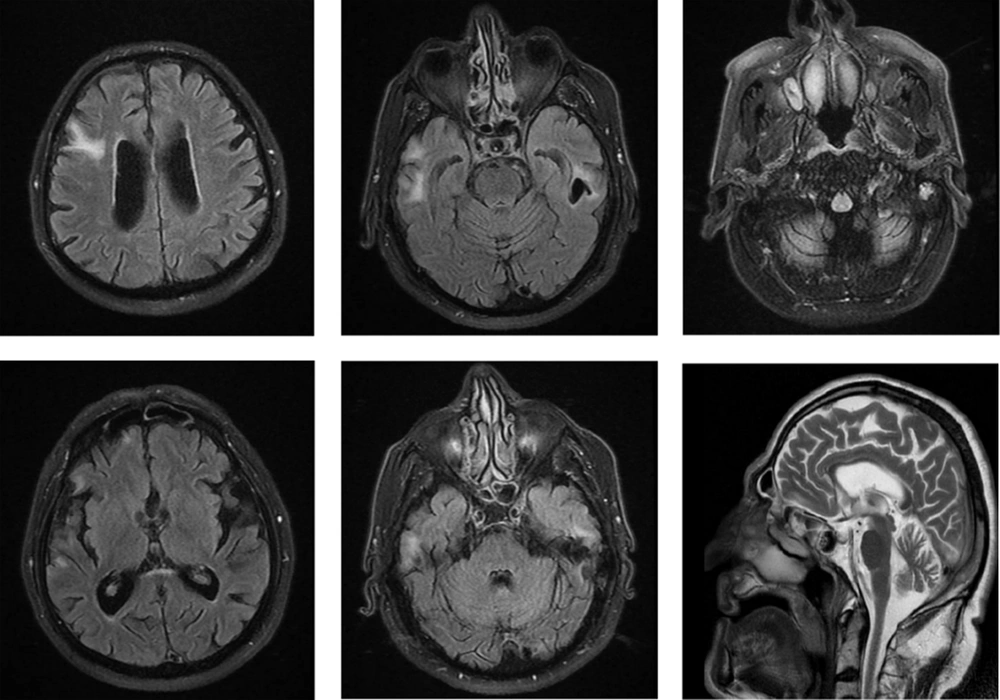
Laboratory test results were unremarkable except for a folic acid deficiency. Magnetic resonance imaging (MRI) of the brain showed moderate global brain atrophy, focal encephalomalacia with peripheral gliosis in the left frontal lobe, and subcortical edema in the right temporal and frontal lobes (Figure 1).
The patient was initially treated with Quetiapine 100 mg, Navalprotate 600 mg, Memantine 5 mg, Donepezil 5 mg, Levothyroxine 0.05 mg, and Folic acid 5 mg on a daily basis. At this dose, cognitive impairment decreased significantly, and his hair-pulling persisted for over 12 months.
3. Discussion
A case with the symptom of TTM associated with progressive dementia was presented in this report. Similar previous reports have mostly involved cases of right-handed men aged > 65 years, as in the present case.
Age is an important factor in the development of cognitive impairment and resulting psychiatric symptoms (11). In addition, older patients are less responsive to treatment. Two cases were reported below the age of 65 years, one with Alzheimer's disease (8) and the other with frontoparietal dementia (2). Evidence has shown that age-related changes in left frontal lobe structures correlate with declines in performance on cognitive tasks requiring rapid processing (12, 13). Although there is some heterogeneous evidence for the presence of brain abnormalities in individuals with hair-pulling behavior, no definitive conclusion has been drawn yet (14). Previous neuroimaging studies of TTM have all used region-of-interest approaches rather than examining distributed abnormalities over the whole brain. Structural MRI studies revealed changes in the frontostriatal motor circuit, including decreased volume of the left putamen and decreased volume of the left inferior frontal gyrus (15). Thus, there were consistent findings for structural abnormalities in the frontal regions in our case. One inconsistent finding was hair pulling from the eyebrows in our patient compared to patients from previous reports in the literature suggesting that hair pulling usually came from the different regions of the scalp.
In this case, hair pulling was due to dementia following head trauma. According to the literature, the patient may present with neuropsychiatric complications at any time after a brain injury. After head trauma, there are acute neurotransmitter changes that result in psychiatric presentations by altering dopamine, norepinephrine, serotonin, and acetylcholine levels. Several studies have demonstrated that traumatic brain injury leads to a decline in dopamine levels in the ascending monoaminergic projections, which has a poor prognosis. Serotonin pathways to the frontal cortex are disrupted by both axonal injuries and contusions, leading to impairment in the neurotransmitter acting (16). Following severe traumatic brain injury, loss of cortical cholinergic afferents is noted with concomitant preservation of postsynaptic nicotinic and muscarinic receptors. Memory and attention impairments are the most common cognitive dysfunctions manifested by patients after traumatic brain injury (17). This could follow primary brain injury or secondary problems such as sleep disturbances. Impairment of executive function is the next important under-reported cognitive sequel of traumatic brain injury. Executive function is primarily controlled by the prefrontal cortex. Dysfunction orbitofrontal/ventromedial pathways impact on a person’s ability to live independently in the community.
3.1. Conclusion
Although preclinical studies increased the knowledge of brain disorders, human studies such as case reports of rare cases greatly facilitated the understanding of clinical relevance. This study reviewed the literature on TTM in dementia case reports that had mostly investigated the cases of right-handed men aged > 65 years. TTM Patients with the underlying disease had not any improvement. Although there was some heterogeneous evidence for brain abnormalities in individuals with hair-pulling behavior, no definitive conclusion was drawn. Mild to severe generalized atrophy in the cerebral cortex was observed in the frontal, parietal, temporal, occipital, and cingulate lobes.