1. Introduction
Posterior reversible encephalopathy syndrome (PRES) is a clinical-radiological disease characterized by headache, seizures, neurological symptoms, and vision loss, as well as white matter vasogenic edema mostly affecting the posterior occipital and parietal lobes of the brain (1). It is frequently, but not always, accompanied by acute hypertension (2). If detected and treated immediately, the clinical condition generally disappears within a week (2), and the alterations revealed by magnetic resonance imaging (MRI) resolve over days to weeks (3).
Previously, it was reported a case of PRES in a 31-year-old female with COVID-19 (4) and also 8 COVID-19 infected patients (4 male) (5). So, PRES can be a neurological complication of SARS-COV-2 infection. In this paper, we reported a rare case of PRES in a pregnant woman and described the successful management of this case.
2. Case Presentation
A 31-year-old pregnant woman (G2 P1 Ab0 L1) in her 33 weeks of gestation was referred to Imam Khomeini Hospital complex (Tehran, Iran) complaining of restlessness and cognitive impairment. In her past medical history, she declared gestational diabetes mellitus (GDM), was treated with insulin, and had no other medical conditions, smoking, or addiction.
In the 10 previous days, with a diagnosis of SARS-CoV-2 infection, which was confirmed by immunoglobulin rapid test (I-RT) and nasopharyngeal polymerase chain reaction (PCR) of the virus, she received four doses of 8 mg of intravenous Dexamethasone (daily) and Remdesivir (200 mg on the first day, then 100 mg for 5 days) as an outpatient. The patient presented restlessness and dyspnea three days ago.
She was referred to the hospital due to cognitive disorder and loss of consciousness. At the Emergency Department, in arterial blood gas, metabolic acidosis has been represented (PH = 7.18, HCO3 = 6, PCO2 = 17), she was intubated following the loss of consciousness and ketonuria (+3), SO was referred to the General Intensive Care Unit (ICU) of Imam Khomeini Hospital complex (IKHC).
At the ICU (admission), she was intubated, under mechanical ventilation (MV) (SIMV+PSV, O2SAT = 93%) and sedated with fentanyl, Midazolam IV infusion. She presented tachycardia (PR:145) with blood pressure (BP = 120/80), and the pupils were Midsize and reactive to light.
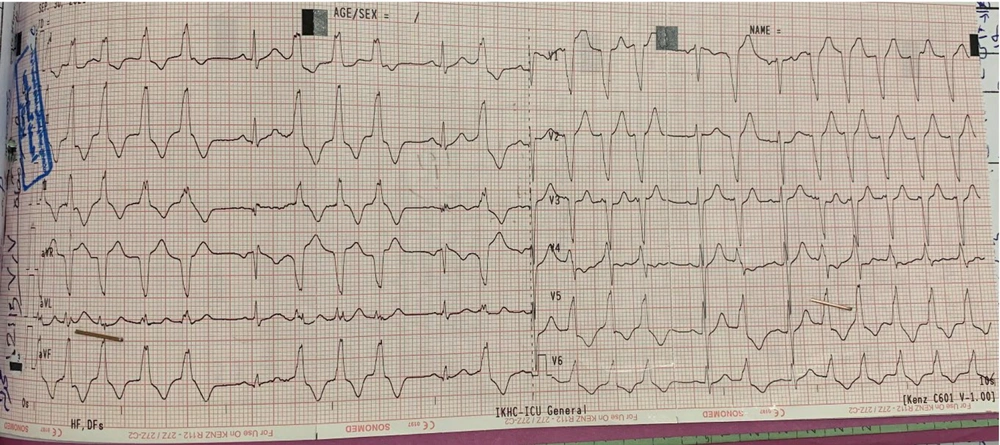
ECG showed sinus tachycardia Rhythm, bigeminy, trigeminy PVCs, and sometimes non-sustained VT (Figure 1).
We started ampicillin, ceftriaxone, aciclovir, vancomycin, metronidazole, methylprednisolone and adenosine, MgSO4 20% and, methohexital for arrhythmia. The bedside sonography of the fetus was normal.
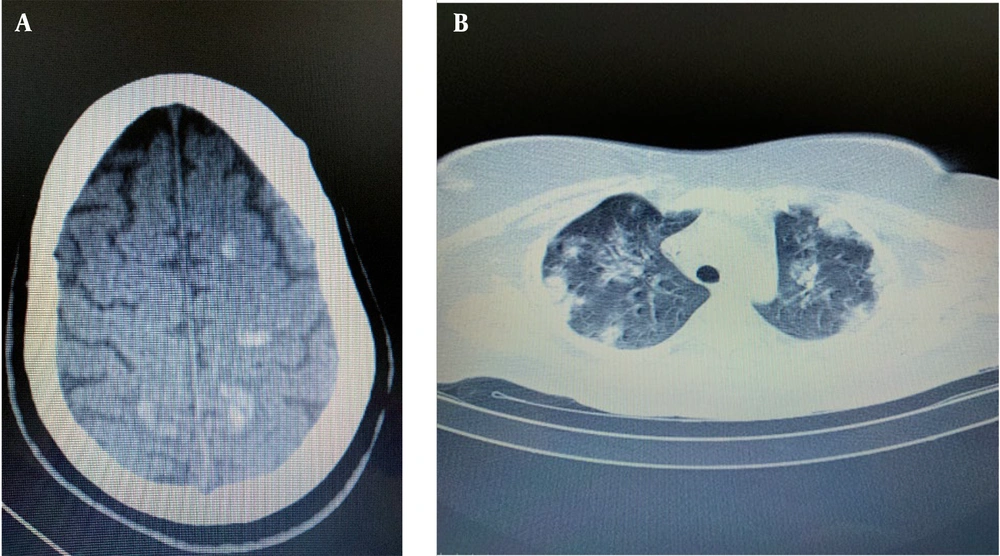
Echocardiography was normal. A Doppler ultrasonography of the lower extremities was normal. The initial brain CT (Figure 2) and LP results were normal. Spiral chest CT (Figure 2) showed bilateral diffused ground glass opacities with consolidations indicative of the late phase of COVID-19. According to bedside sonography, the BPP was 2/8 (Table 1).
| Services | Results |
|---|---|
| Echocardiography | LVEF = 50 - 55%, PAP = 25 mmhg, NO PE, NO MS, Mild MR, NO AS, NO AR, NL RA, NL RV, NL LA, NL LV |
| Lumbar puncture (LP) | WBC = 0 - 1, RBC = 0 - 1, Glu: 207 |
| Spiral chest CT | 40 - 50% pulmonary involvement with pneumomediastinum |
| Cesarean section | BP = 100/50 with drip NEP 5 µg/h IV infusion; Anesthesia: Fentanyl 150 µg and propofol 200 mg; After delivery: Atracurium 40 mg and isoflurane for maintenance of the anesthesia. |
| ABG | PH = 7.39 PCO2 = 30.7 HCO3 = 18.8 |
| Portable EEG | Severe encephalopathy and no evidence of non-convulsive status epilepticus (NCSE); localized the painful stimulations GCS: 9/15 |
| Cardiac consultation for dysrhythmia | Echocardiography: EF = 50 - 55%, PAP = 25. |
| Lupus work-up | Anti DS DNA = 1.8, ANA = 2.32, anti-cardiolipin = 1.7, B2 glycoprotein IGG = 1.4. |
| LP | WBC = 0 - 1; RBC = 320; GLU = 79; Pr = 99; LDH = 70; HSV & TB PCR: NEG |
| Tumor biomarkers | CEA = 3.6, CA125 = 53.4, CA15 = 38.3 CA19-9 = 39, HCG = 25, AFP = 16.6 HE4 = 193, ROMA = 68.5. |
| Brain MRA | No evidence of aneurysm, AVM, or cerebral venous sinus thrombosis was detected on brain MRA/MRV. |
| Thyroid lab test | TSH = 10, T4 = 9.8, T3 = 86 |
An emergency C-section was performed with general anesthesia in the ICU due to acidosis and instability of the mother and fetus. The baby boy was born with an Apgar score of 8 and no obvious anomalies and was intubated. After the section, the ABG was normal.
According to the result of endotracheal tube culture, which was Klebsiella, we started imipenem and vancomycin instead of cefteriaxone and ampicillin. The portable EEG (2021.10.03) was consistent with severe encephalopathy and no evidence of non-convulsive status epilepticus (NCSE). After five days of hospitalization, the patient localized the painful stimulations (GCS:9/15), therefore was extubated.
New spiral brain CT without contrast showed multiple hyperdense lesions sporadically with surrounding edema suspected of cerebral choriocarcinoma. The chest CT did not show ground glass opacities due to COVID-19.
The left eye became inflamed and red, so we used an ophthalmology consultation, which they ordered: Orbital MRI with GAD+fat suppression, and with suspicion of Mucormycosis, ENT consultation was performed. It was recommended to perform a diagnostic endoscopy in the OR. Also, due to the clear sinuses, the probability of Mucor is very low. Three days later, cardiac arrhythmia persisted, and scattered PVCs were seen. Cardiac consultation believed in arrhythmias due to autonomic conflict and an increase in ICP.
Tests based on lupus were performed, and lupus was ruled out. Four days later, she was conscious but had no communication. Following a neurological examination, LP was performed. A day after, she was oriented.
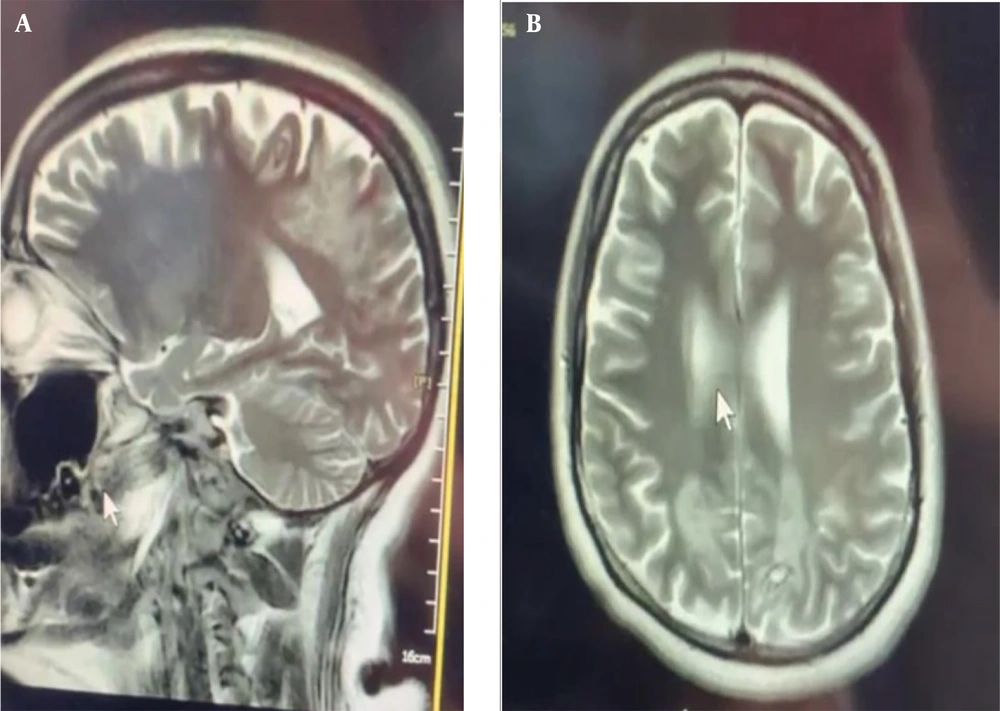
Brain MRI noted a multifocal abnormal signal intensity in subcortical and deep white matter in both the Parieto-occipital regions containing hemorrhagic foci without enhancement. The possibility of increased vascular resistance was suggested due to evidence of decreased distal branches of PCAs, which could be secondary to decreased venous flow drainage.
Based on neurological problems and multiple hypersignal lesions and subcortical hemorrhagic foci on brain MRI (Figure 3), which were mainly distributed in bilateral parieto-occipital regions, the main differential diagnosis considered was posterior reversible encephalopathy syndrome (PRES) in the context of preeclampsia. Other potential diagnoses included vasculitis, cerebral venous sinus thrombosis, nonherpetic viral infection, and, less probably, hemorrhagic metastasis such as choriocarcinoma.
The Circle of Willis and major intracranial vascular structures appear normal. All tumor markers were negative.
Thyroid tests indicate subclinical hypothyroidism. With the impression of PRES and conservative management, the patient improved clinically during two weeks and was discharged from the hospital (14 days after hospitalization).
Two months later, the patient was visited for follow-up. She didn’t mention any complaints and only complained of occasional headaches when tired. Her physical examinations were normal. A follow-up brain MRI with/without contrast was also normal.
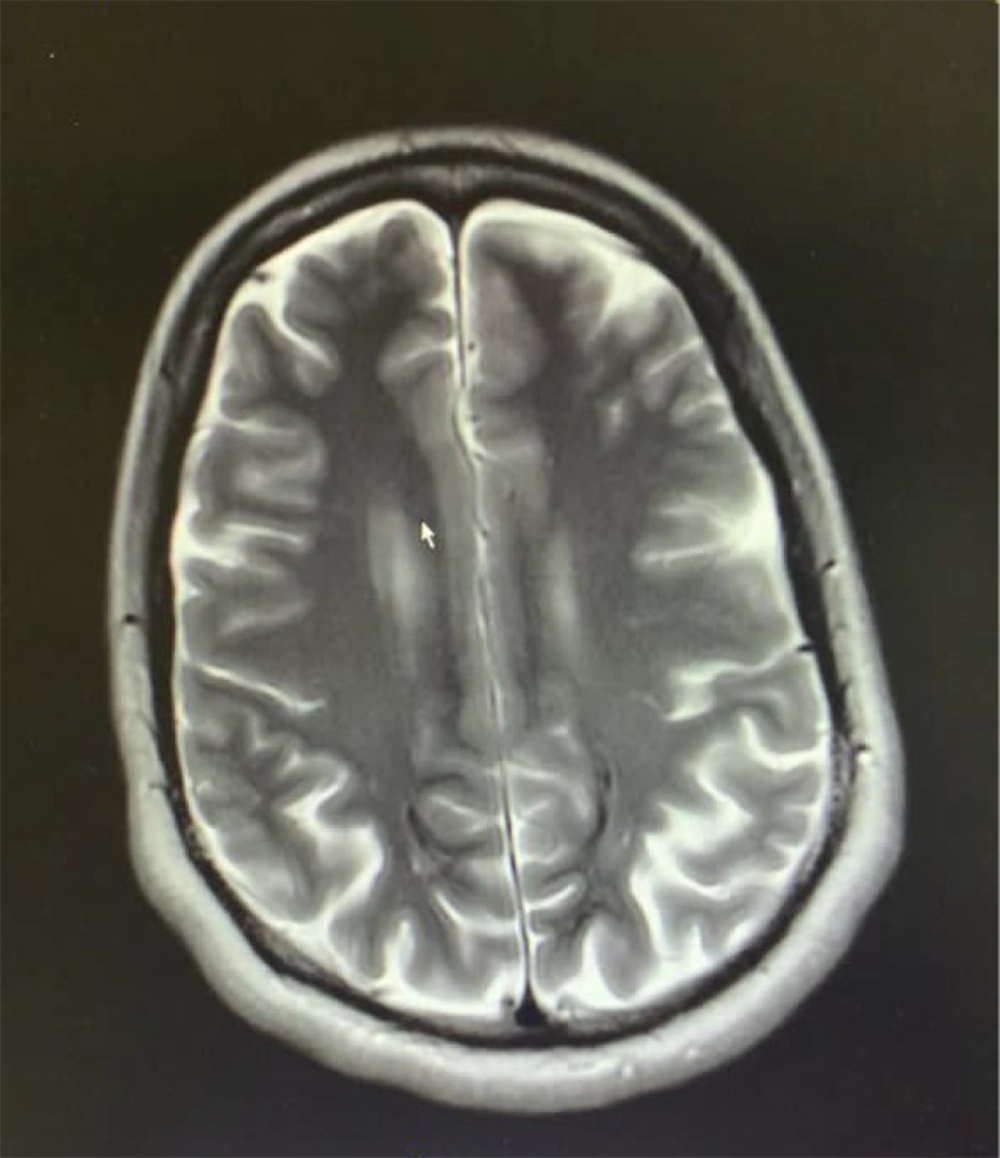
At the final follow-up 6 months after discharge, the patient's MRI (Figure 4) showed the presence of laminar necrosis in the two occipitoparietal cortex areas, especially on the left side. However, the patient was symptom-free and did not report any complications.
3. Discussion
Pregnant women with COVID-19 are at greater risk of severe disease than their non-pregnant PRES, and yet they are frequently denied investigations or treatments because of unfounded concerns about the risk to the fetus (6). The basic principles of diagnosing and managing COVID-19 are the same as for non-pregnant patients, and a multidisciplinary, expert team approach is essential to ensure optimal care (7, 8). The unique feature of our case was being pregnant and simultaneously infected with COVID-19. During pregnancy, corticosteroid treatment should be modified to use non-fluorinated glucocorticoids (6). Il-6 inhibitors, monoclonal antibodies, and specific antiviral therapies may also be considered. Prophylaxis against venous thromboembolism is important for hospitalized COVID-19 patients (9). Pregnant women may require respiratory support with oxygen, non-invasive ventilation, ventilation in a prone position (either awake or during invasive ventilation), intubation and ventilation, and extracorporeal membrane oxygenation (ECMO) (7-9). Pregnancy is not a contraindication for any of these supportive therapies, and the criteria for providing them are the same as in the general population (6). In the presented case, all necessary diagnostic tests (blood test, echocardiography, X-ray, and LP) and appropriate COVID-19 treatments (antimicrobial, Dexamethasone, and Remdesivir) were provided on time.
Additionally, Decisions regarding timing, place, and mode of delivery should be made with a multidisciplinary team including obstetricians, physicians, anesthetists, and intensivists experienced in caring for COVID-19 pregnant women (8). Ideally, these decisions should occur in consultation with centers with experience and expertise in all these specialties. In our case, a multidisciplinary team was involved, including a critical care specialist, an anesthesiologist, a gynecologist, an internist, an infectious disease specialist, a pharmacotherapist, a cardiologist, and critical care nurses.
PRES is a well-known and recognized complication of immunosuppressive drugs. However, its association with disorders such as renal insufficiency, malignant hypertension, preeclampsia, eclampsia, and some autoimmune disorders has been reported. Interestingly, our case was neither preeclampsia nor eclampsia, nor did it have any history of cancer or autoimmune disorders. Recently, several cases of PRES in the setting of COVID-19 have been reported (10-12). PRES is suggested when neurological manifestations, including headache, seizure, confusion, focal neurological deficit, or decreased level of consciousness in a setting of the situations mentioned above, are associated with typical brain MRI findings (10-12). In common with previous reports (10-12), in our case, the patient, who was a confirmed COVID-19 case and received initial treatments (dexamethasone and remdesivir), was referred to the hospital with a decreased level of consciousness. Parieto-occipital hyperintensity in fluid attenuated inversion recovery (FLAIR) and T2-weighted images (T2WI) is the most characteristic feature of PRES. In our case, hemorrhagic foci on brain MRI were primarily distributed in bilateral parieto-occipital regions. However, involvement of the temporal, frontal, basal ganglia, cerebellum, and brain stem is not unusual, especially when diagnosis is delayed.
Meanwhile, about 15 - 20% of PRES cases develop hemorrhagic brain lesions, mainly petechial bleeding, and rarely intraparenchymal hematoma, as in our patient, which is usually associated with poor outcomes. Accordingly, PRES may be associated with cytogenic edema and diffusion restriction patterns on brain MR imaging (12). Compared to other studies, the most important highlight of our study is that our patient had no underlying disease. Previous studies reported mostly elderly patients with a history of hypertension or in cases of pregnancy with conditions such as preeclampsia. Most PERS cause brain damage, such as edema and ischemia, by changing autoregulation. A small percentage is associated with intracerebral hemorrhage. Intracerebral hemorrhage in the reported case is associated with differential diagnoses, such as choriocarcinoma metastasis to the brain, which was rejected in the subsequent assessments. In this disorder, the brain stem is less involved (cardioexcitatory system), and autonomic changes are less visible. As a result, complications caused by cardioexcitatory involvement, such as arrhythmias, may be less common. However, in our case, more autonomic changes were seen (ECG).
Unlike the general population, pregnant women are prone to infection by acute respiratory diseases and severe pneumonia, especially if they have chronic diseases. SARS infection during pregnancy can be severe, causing spontaneous abortion, preterm delivery, and limited growth. Nevertheless, no evidence supports vertical transmission of SARS infection from mother to fetus (1, 3).
3.1. Conclusions
Pregnant women with COVID-19 infections admitted to a critical care setting may need an emergent C-section, which clinicians should keep in mind. Additionally, PRES can be a potential consequence of COVID-19 disease even in pregnant women and is suggested to be considered for differential diagnosis.