1. Background
Multiple sclerosis (MS) is a chronic, disabling neuroinflammatory demyelinating disease affecting the central nervous system. This disorder primarily manifests in young adults and causes a range of sensory, motor, and cognitive impairments (1, 2). Although MS often begins in youth, its symptoms can persist for a lifetime, making it a long-term condition that significantly impacts patients over many years (3). Typically, MS presents as a remitting-relapsing course characterized by inflammatory demyelination and neurological disability resulting from axonal damage (4). However, other MS phenotypes can include progressive clinical disability, with or without periods of relapse and remission (5). The presence of demyelinated lesions below the level of the cerebellar tentorium and involvement of the spinal canal can lead to increased disability in MS patients (6).
Cervical spondylosis (CS) is a common age-related condition with a chronic and progressive nature that affects the bone and cartilage of the cervical vertebrae (7). The cervical spinal structures, including bones, intervertebral discs, facets, and ligaments, are most commonly involved in CS (8). Severe cases of CS can exert pressure on the spinal cord and result in associated myelopathy. Although degenerative changes can occur at any age, they are not always symptomatic (9). Mechanical forces caused by cervical spondylosis contribute to local neuroinflammation by increasing the vascular permeability of the spinal blood barrier, which, over time, leads to apoptotic responses in neurons and oligodendrocytes (10, 11).
Symptoms related to cord compression due to CS can resemble those of MS and include spasticity, gait incontinence, sensory deficits, weakness in the lower and/or upper extremities, gastrointestinal and genitourinary dysfunction, Lhermitte's sign, and pain in the upper limbs or neck (12). The concurrent presence of MS and CS presents a challenge for neurologists and neurosurgeons in diagnosing, treating, and managing the conditions. There is often uncertainty about which disease is the primary cause and concern that spinal manipulation may trigger an MS relapse or exacerbation (13).
The issue of the association between MS and CS and their impact on each other was first explored by Brain and Wilkinson in 1957, who questioned whether the clinical characteristics of MS are affected by cervical cord compression due to degenerative changes. To address this question, they performed autopsies on only two patients, finding that the sites of demyelination were associated with the presence of spondylotic bars. They suggested that these bars might have had a compressive effect on the cord, leading to impaired blood supply. Therefore, both spondylotic changes and demyelinating plaques might have a reciprocal role. However, they concluded that further investigation was needed for a more definitive answer (14).
Twenty years later, neuropathologist Oppenheimer examined the spinal cords of 18 MS patients and found no association between plaque locations and degenerative changes. Instead, he noted that spondylotic lesions were typically fan-shaped and located in the lateral columns. Oppenheimer hypothesized that "mechanical stresses" might contribute to plaque formation due to the impact of fibrous adhesions on the dura, rather than compressive effects (15).
The key question remains: Can decompressive interventions reduce plaque formation and MS symptoms? Data on this topic are controversial. While it has been shown that carefully selected MS patients could benefit from decompressive surgery, comparisons with healthy individuals did not reveal significant differences (16, 17).
Magnetic resonance imaging (MRI) is the preferred method for assessing cord lesions in MS. Limited evidence is available on the association between myelopathy due to cord compression in CS and the deterioration or progression of MS lesions (5, 12, 18). Despite these efforts, previous studies have not utilized MRI with contrast to enhance the visualization of lesions.
2. Objectives
The current study aims to assess the association between CS and its effects on the spinal cord with enhanced MS cervical lesions.
3. Methods
3.1. Study Population
The current retrospective cross-sectional study was conducted on 104 MS patients with concurrent cervical spondylosis who were referred to outpatient MS clinics affiliated with Isfahan University of Medical Sciences from January 2019 to March 2021.
The study protocol adhered to the principles of the Helsinki Declaration, was submitted to the Ethics Committee of Isfahan University of Medical Sciences, and was approved under code number IR.MUI.MED.REC.1399.1167. Patients were informed about the potential use of their medical data for scientific research, assured of the confidentiality of their personal information, and provided written consent.
Patients over eighteen years old with a documented diagnosis of multiple sclerosis based on McDonald Criteria 2017 (19), who underwent both enhanced and unenhanced cervical MRI during the study period and had an active medical record in the referral MS clinics, were included. Exclusion criteria included having more than 20% missing data in medical records, a history of spinal surgery, or the presence of other pathologies such as congenital spinal deformities, spinal tumors, cervical vertebrae fractures, or spinal cord trauma (17).
The study population was selected through convenience sampling. All MRI images were interpreted by a panel consisting of two neuroradiologists and one neurologist, all of whom are experts in neuroimaging interpretation.
3.2. Data Collection
The retrieved demographic and medical data of the patients included age at disease onset, gender, MS phenotype (remitting-relapsing MS (RRMS), primary progressive MS (PPMS), secondary progressive MS (SPMS), and progressive-relapsing MS (PRMS)) (20), disease duration, medication history, and the Extended Disability Status Scale (EDSS) (21) at the time of the study.
The MRI images were acquired using a 1.5 Tesla MRI, following the MS Centers' consensus 2019 guidelines. Gadolinium-based contrast (287 mg/mL) was administered intravenously at a dosage of 0.1 mmol/kg for 30 seconds, and imaging was performed within the subsequent 5 minutes (22). Table 1 presents the MRI protocols used in the current study (23).
Abbreviations: FSE, Indicates fast spin-echo (or turbo spin-echo); PD, proton density-weighted (long TR, short TE sequence); T2, T2-weighted (long TR, long TE sequence); T1, T1-weighted (short TR, short TE sequence).
a PD series may depict lesions less apparent on heavily T2-weighted series.
b Increases confidence in the findings of sagittal series; may provide classic lesion characteristics.
c Standard dose of 0.1 mmol/kg injected over 30 s; scan starting 5 min after start of injection.
The images were interpreted to identify the presence of cervical spondylosis and demyelinated cervical plaques (active or inactive). Cervical spondylosis was categorized into 4 grades using the Muhle scale (Table 2) (24).
| Grade | Definition |
|---|---|
| 0 | Normal spinal canal diameter, without anterior or posterior subarachnoid space stenosis |
| I | Incomplete obliteration of the anterior or posterior subarachnoid space or both |
| II | Complete obliteration of the anterior or posterior subarachnoid space or both |
| III | Compressive effect on the spinal cord anteriorly or posteriorly or both |
The MS plaques were evaluated in terms of extension, enhancement, and cervical plane. Spinal cord lesion extension was categorized as: No spinal plaque, solitary cervical plaque, multiple non-contiguous spinal plaques, and multiple contiguous spinal plaques. The plaques were classified as either enhanced (active) or non-enhanced (inactive). Additionally, the spinal cord cross-sectional area (SC - CSA) was measured at the C2 - C3 cervical spine level (25).
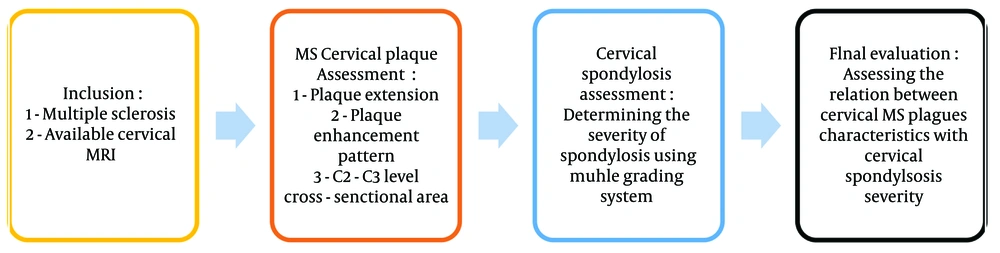
Figure 1 illustrates the process of the study.
3.3. Statistical Analysis
The obtained data were entered into the Statistical Package for Social Sciences (version 20, IBM Corporation, Armonk, NY). Descriptive statistics were presented as means, standard deviations, absolute numbers, and percentages. The independent t-test or one-way ANOVA test was used to compare continuous data. Categorical information was compared using the chi-square test or Fisher’s exact test. A P-value of 0.05 was considered the level of significance.
4. Results
The current investigation was conducted on 104 MS patients with a mean age of 34.8 ± 7.9 years (range: 18 - 56 years). The study population predominantly consisted of females (n = 69, 66.3%). The Muhle grading system revealed that most patients had cervical spinal cord alignment within the physiological range (40.4%), followed by grades 1 (27.9%) and 2 (20.2%) (Table 3).
| Variables | Measurement |
|---|---|
| Age (y) | 34.8 ± 7.9 |
| Duration of the disease (y) | 4.6 ± 0.3 |
| Extended Disability Status Scale | 1.8 ± 0.1 |
| Gender | |
| Male | 69 (66.3) |
| Female | 35 (33.7) |
| Muhle cervical spondylosis grading | |
| 0 | 42 (40.4) |
| I | 29 (27.9) |
| II | 21 (20.2) |
| III | 12 (11.5) |
a Values are expressed as No. (%) or mean ± SD.
Table 4 demonstrates the association of SC grading with various demographic and clinical categories.
| Variables | 0 | I | II | III | P-Value |
|---|---|---|---|---|---|
| Age (y) | 30.4 ± 6.7 | 34.03 ± 6.2 | 39.1 ± 6.4 | 44.4 ± 6.6 | < 0.001 |
| Disease duration (y) | 3.9 ± 0.5 | 4.3 ± 0.7 | 5.4 ± 0.8 | 6.05 ± 1.1 | 0.04 |
| EDSS | 1.5 ± 0.2 | 1.8 ± 0.3 | 2 ± 0.3 | 2.3 ± 0.4 | 0.03 |
| Gender | 0.90 | ||||
| Male | 14 (33.3) | 10 (34.5) | 6 (28.6) | 5 (41.7) | |
| Female | 28 (66.7) | 19 (65.5) | 15 (71.4) | 7 (58.3) | |
| Plaque extension | 0.13 | ||||
| Without spinal plaque | 17 (40.5) | 11 (37.9) | 7 (33.3) | 3 (25) | |
| Solitary cervical plaque | 16 (38.1) | 11 (37.9) | 6 (28.6) | 4 (33.3) | |
| Multiple non-contiguous spinal plaques | 6 (14.3) | 5 (17.3) | 5 (23.8) | 3 (25) | |
| Multiple contiguous spinal plaques | 3 (7.1) | 2 (6.9) | 3 (14.3) | 2 (16.7) | |
| Enhancement pattern | 0.25 | ||||
| Enhanced (active plaque) | 4 (18.2) | 3 (15.8) | 4 (28.6) | 3 (37.5) | |
| Unenhanced (inactive plaque) | 18 (81.8) | 16 (84.2) | 10 (71.4) | 5 (62.5) | |
| C2 - C3 level cross-sectional area (mm2) | 73.8 ± 3.4 | 72.7 ± 3.7 | 71.7 ± 3.8 | 68.5 ± 3.7 | < 0.001 |
a Values are expressed as mean ± SD or No. (%).
5. Discussion
However, although spondylosis can begin at any age, it is generally associated with aging (26). Consequently, potential compression on the spinal cord can adversely affect patients with multiple sclerosis (27). In the current study, we investigated factors related to the severity of cervical spondylosis in MS patients and found that older age, longer duration of MS, worse EDSS scores, and a smaller C2 - C3 cervical level cross-sectional area were associated with more severe spondylosis. However, other characteristics, including gender, the extension of MS plaques, and the activity of the plaques, did not show any correlation with the severity of spondylosis.
Given the nature of spondylosis, it is not surprising to find a direct association between patients' age and the severity of cervical spondylosis. Literature consistently shows greater progression of spondylosis among older individuals compared to younger ones, regardless of whether they have a disease (9, 28, 29). In agreement with our findings, Bomprezzi et al. also reported more severe spondylosis among older MS patients (18).
The current study also revealed that patients with a longer duration of MS and more severe disabilities based on the EDSS experienced more severe cervical spondylosis. Consistent with these findings, another study on MS patients with cervical spine degenerative disorders showed that those with exacerbated MS symptoms had worse manifestations of spondylosis, including disc degeneration, posterior disc protrusion, endplate changes, and canal and foraminal stenosis (30). These results were supported by other studies (16, 17). We hypothesize that these findings may be due to the higher age of these patients, who are potentially at increased risk for cervical degenerative disorders. However, patients with longer MS duration and more severe EDSS scores might experience more severe MS-related disabilities, which could lead to chronic positioning in inappropriate alignments to alleviate pain or compensate for disabilities. This chronic positioning might accelerate the development of spondylosis over time (17, 31). Additionally, researchers have suggested that reduced exercise tolerance, a high Body Mass Index, and reduced core muscle strength, along with excessive or non-mechanical pressure on the spinal column, can cause abnormal posture and loss of normal spinal curvature (32, 33). Furthermore, Chhugani et al. identified suboptimal bone health and vitamin D deficiency in MS patients as factors contributing to the exacerbation of cervical spondylosis. They suggested that the inflammatory nature of MS may trigger the early onset or accelerate the progression of degenerative disease, indicating a bidirectional association where each condition might worsen the other (30). However, Bomprezzi et al. did not find an association between EDSS and cervical spondylosis, even after adjusting for age, gender, disease duration, and MS phenotype (18). Similarly, Alkrenawi et al., in their assessment of discopathy in MS patients, reported no association between MS symptoms and the severity of cervical disc degeneration (34).
Another expected result of the current study showed an inverse association between the area of the cervical cord at the C2 - C3 level and the severity of spondylosis. Similar outcomes have been reported in the literature, as more severe spondylosis is potentially associated with canal and foraminal stenosis (30). Gratch et al. even suggested that as cervical spondylosis progresses, the interrupted blood supply to the cord could potentially cause MS lesion progression. They proposed that the increased pressure from nearby tissues might play a role in the pathogenesis of MS. However, they also noted that cervical spondylosis is not the sole factor contributing to the pathogenesis of MS (17).
Despite these findings, we found no relation between MS plaque extension or activity and the severity of cervical spondylosis. Data from other studies on this topic are controversial. Ocak et al. reported that discopathy was associated with MS plaque formation by generating microtraumas that disrupt the blood-brain barrier (5). Conversely, Gratch et al. found that segments with at least moderate cervical spondylosis were significantly associated with the presence of MS lesions in the same segment (17). Other studies have proposed that repetitive trauma at the site of stenosis leads to the breakdown of the blood-spinal cord barrier, allowing immune cells to invade the central nervous system and contribute to plaque formation (18, 35). Compromised blood supply to the blood-spinal cord barrier due to recurrent mechanical forces may contribute to neuroinflammation, another mechanism by which MS lesions might form (11, 17). Additionally, atrophy due to continuous pressure on the cord, friction, or traction on the affected spinal cord portion might worsen MS disabilities, not only impairing blood supply but also affecting the functions surviving from MS activities (36, 37).
Although, to the best of our knowledge, the current study is the only one using contrast to assess the association between MS plaque activity and the severity of, our findings were inconsistent with the hypothesized relationship. This discrepancy might be due to the larger sample size or a failure to control for potential confounding variables affecting CS severity, MS symptoms, clinical manifestations, or neuroimaging characteristics.
5.1. Conclusions
Based on the findings of this study, the severity of CS was associated with age, duration of MS, EDSS, and the C2 - C3 cervical spine cross-sectional area. However, there was no observed relationship between CS and the extension or activity of MS plaques. Although the interactions between MS and CS, as well as approaches for their management, have long been a topic of investigation with ongoing controversies, further research is needed to enhance our understanding and guide decisions on surgical versus conservative management for these patients.