1. Context
Obstructive sleep apnea (OSA) is one of the most common sleep disorders, characterized by recurrent episodes of interrupted breathing during sleep. This leads to reduced airflow and disruptions in sleep patterns. OSA can result in sleep disturbances, excessive daytime sleepiness, an increased risk of motor vehicle accidents, and a reduced quality of life (1). The prevalence of moderate to severe OSA is estimated to be between 6% and 17% in the general adult population (2), affecting approximately 425 million adults worldwide. Additionally, mild to moderate OSA is even more prevalent, impacting approximately 936 million adults globally (3). This condition tends to affect more men than women (4). However, a significant proportion of cases go undiagnosed because OSA is not easily detected by patients during their sleep (4, 5).
OSA is also associated with several other health conditions, including cardiovascular diseases such as hypertension, arrhythmias, heart failure, and stroke (6, 7), as well as neuropsychiatric effects like depression and cognitive impairments (8). Managing OSA can be challenging, particularly in individuals with higher body mass index (BMI), females, those experiencing depression, and individuals with lower total sleep time (9).
Due to its significant burden and prevalence, the treatment of OSA is of paramount importance, and treatment should commence immediately following diagnosis for patients with OSA. Current treatments designed to reduce the frequency of sleep events in OSA include continuous positive airway pressure (CPAP) (10), weight loss, lifestyle modification (11, 12), surgical procedures (13), and pharmacotherapy (14). In recent decades, CPAP (10) has been the standard treatment for managing clinically significant OSA. CPAP is associated with the reduction of apnea and hypopnea events, the elimination of hypoxia, a significant decrease in blood pressure in patients with hypertension, and improved cardiovascular outcomes (15). However, compliance with CPAP treatment is as low as 60% in patients with OSA. Furthermore, CPAP only suppresses respiratory disturbances during sleep while the devices are in use and does not offer a permanent resolution (16, 17). In addition to CPAP, pharmacotherapy, weight loss, and lifestyle modification may be recommended as long-term alternatives for patients in whom CPAP treatment fails. Surgery may also be considered for patients with evident anatomic obstructions, such as lingual tonsils, or for those who do not respond to CPAP or other treatments (18, 19).
Given the limitations of common treatments for OSA, many alternative therapies have been explored, including mandibular advancement devices (MAD) and hypoglossal nerve stimulation (20, 21). Among these alternatives, acupuncture emerges as a traditional yet novel treatment for OSA. Acupuncture is widely accepted by both patients and specialists in various related fields and is commonly used to treat a wide range of conditions, including low back pain, arthritis, gastrointestinal disorders, headaches, asthma, alcohol and substance dependence, and other mental disorders. Acupuncture is also widely recognized in many Western countries as a complementary therapy (22, 23).
The apnea-hypopnea index (AHI) is an important outcome measure in assessing the effectiveness of OSA treatment, although there is no clinically meaningful significant threshold (24). Several studies have indicated that acupuncture is effective in improving the AHI (25, 26).
2. Objectives
The objective of our current study was to review the clinical effectiveness of acupuncture therapy in treating OSA, which could offer an effective and affordable treatment option for this condition.
3. Acupuncture
Acupuncture involves the insertion of fine needles, known as acupoints or meridian points, into specific areas of the body for therapeutic purposes. These acupoints are located on the body's surface and can have therapeutic effects when stimulated. Traditional Chinese Medicine has long employed acupuncture as a primary treatment modality for various illnesses, with a history dating back over two thousand years in China (27). Acupuncture operates on complex theories that regulate forces, such as Yin and Yang, Qi (air), blood, and body fluids. According to Chinese Medicine, pain or illness results from an imbalance in the body's Yin and Yang forces or an excess or deficiency of Qi, blood, or other body fluids. Acupuncture helps restore balance by stimulating different acupoints corresponding to different body parts and their interactions, thereby rebalancing Yin and Yang forces and normalizing Qi, blood, and other bodily fluids (28).
Aside from traditional needle acupuncture, various other forms of acupuncture exist, including electroacupuncture (EA), laser acupuncture, acupressure, auricular therapy, magnetic acupressure, and transcutaneous electrical acupoint stimulation (TEAS) (29). EA involves connecting acupuncture needles to a machine that generates continuous electric pulses, creating a small electric current between needle pairs. Laser acupuncture employs a laser beam to stimulate acupoints instead of traditional needles. Acupressure entails applying firm pressure to acupoints (30). Auricular therapy focuses on stimulating acupoints on the auricles (ear) using needles, seeds, or magnetic beads. Magnetic acupressure involves the use of small magnets to apply pressure and magnetic stimulation to acupoints (31). The TEAS method employs electrode pads to stimulate acupoints through a combination of acupuncture and transcutaneous electrical nerve stimulation (32).
4. Clinical Effect of Acupuncture on Obstructive Sleep Apnea
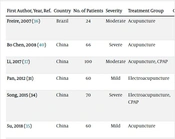
Several randomized controlled studies have been conducted to evaluate the efficacy of acupuncture in the treatment of OSA (24, 25, 27, 28, 33-37) (Table 1). The majority of these studies were conducted in China (33-40). The primary outcome of interest in all these studies is the apnea-hypopnea index (AHI). Some of these studies also measured secondary outcomes such as the Epworth Sleepiness Scale (ESS), adverse events, and lowest oxygen saturation (LSpO2).
| First Author, Year, Ref. | Country | No. of Patients | Severity | Treatment Group | Control Group | Duration, Frequency | Outcomes | Mean Difference for AHI (95% CI) |
|---|---|---|---|---|---|---|---|---|
| Freire, 2007 (43) | Brazil | 24 | Moderate | Acupuncture | Receiving no treatment | 10 weeks, 1 session per week | AHI, adverse effects | -18 (-28.77, -7.43) |
| Bo Chen, 2008 (40) | China | 66 | Severe | Acupuncture | CPAP | 20 days, 7 sessions per week | AHI, LSpO2, | -4.02 (-7.43, -1.75) |
| Li, 2017 (37) | China | 100 | Moderate | Acupuncture, CPAP | CPAP | 4 weeks, 7 sessions per week | AHI, ESS, LSpO2 | -9.60 (-10.53, -8.67) |
| Pan, 2012 (36) | China | 60 | Mild | Electroacupuncture | CPAP | 20 days, 7 sessions per week | AHI, LSpO2, | -2.10 (-3.98, -8.16) |
| Song, 2015 (39) | China | 70 | Severe | Electroacupuncture, CPAP | CPAP | 6 weeks, 3 sessions per week | AHI, ESS, LSpO2, adverse effects | -10.77 (-13.38, -8.16) |
| Su, 2018 (35) | China | 60 | Mild | Acupuncture | CPAP | 4 weeks, 7 sessions per week | AHI, ESS | -0.07 (-2.46, -2.60) |
| Xu, 2017 (34) | China | 80 | Mild | Electroacupuncture, Chinese medicine | Chinese medicine | 8 weeks, 3 sessions per week | AHI, LSpO2 | -2.30 (-.364, -0.96) |
| Zhang, 2014 (38) | China | 90 | Moderate | Acupuncture | CPAP | 4 weeks, /NA | AHI, adverse effects | -7.16 (-11.07, -0.85) |
| Zhao, 2015 (33) | China | 34 | Severe | Acupuncture | Western medicine | 4 weeks, 6 sessions per week | AHI, ESS | -7.30 (-13.77, -0.85) |
Abbreviations: AHI: apnea-hypopnea index; NA: not assessed; CPAP: continuous positive airway pressure.
However, it is important to note that many of the studies in this field have limitations and a high risk of bias. Despite this, most published clinical trials suggest that acupuncture significantly improves AHI (26). Acupuncture appears to be particularly effective in reducing AHI in moderate and severe cases of OSA, compared to mild cases. Furthermore, acupuncture has shown effectiveness in reducing ESS scores, especially in moderate and severe cases of OSA (26). On the contrary, studies have indicated that acupuncture tends to improve LSpO2 levels in mild and moderate patients with OSA rather than those with severe cases.
Common adverse events reported in these studies include infection, hematoma, fainting during acupuncture, and needle bending (28, 33-40). The most commonly used acupoints for the treatment of obstructive sleep apnea are Zhaohai (KI6), Sanyinjiao (SP6), Sishencong (EX-HN1), Shenmen (HT7), Zusanli (ST36), and lianquan (CV23). The selection of acupoints is critical to the success of the treatment, and the needles must be inserted properly in order to achieve the desired effect (26).
In summary, a comprehensive review suggests that manual acupuncture (MA) is more effective than nonspecific therapy in improving AHI, apnea index, hypopnea index, and mean SpO2. EA may further reduce the AHI and apnea index. However, no significant difference was observed in improving the hypopnea index and SpO2 when comparing MA to CPAP therapy (25).
In an RCT study involving forty-four patients with obstructive sleep apnea and comorbid hypertension, there were no differences in pre-intervention and post-intervention AHI, daytime or nocturnal BP, or quality of life between the acupuncture and control groups. This leads to the conclusion that acupuncture therapy does not reduce the severity of obstructive sleep apnea, daytime or nocturnal BP, or quality of life in patients with obstructive sleep apnea and comorbid hypertension (41).
Another study focused on assessing the effectiveness of acupuncture in improving sleep quality and neurological function in stroke patients with sleep apnea syndrome. The results indicated that combining Western medicine treatment with acupuncture significantly reduced clinical symptoms in stroke patients with sleep apnea syndrome and improved their sleep quality and neurological function (42). Within this study, parameters such as sleep onset latency, sleep time, sleep efficiency, minimum oxygen saturation (SpO2 min), longest apnea, and AHI showed improvements in both groups after treatment. However, the observation group exhibited more significant changes. Additionally, the observation group had a higher overall efficacy rate compared to the control group. Serum levels of neuron-specific enolase (NSE) and S100 calcium-binding protein β (S100β) were lower in both groups after treatment, with the observation group showing lower levels than the control group. Furthermore, the Montreal Cognitive Assessment (MoCA) score improved in both groups after treatment, with the observation group having a higher score than the control group (42).
Acupuncture offers several advantages as an adjunct therapy for OSA. One notable advantage is its ability to provide a rapid treatment effect on the AHI and the number of nocturnal respiratory events in patients with OSA (43). Currently, CPAP is the most effective therapy for OSA, delivering constant positive pressure during inhalation and exhalation. However, CPAP requires patients to make significant efforts to maintain equipment and correctly position the mask. Additionally, acupuncture is a more cost-effective option and carries a lower risk of side effects.
The use of CPAP has been associated with various direct side effects, including headaches, chest discomfort, and sensations of suffocation or difficulty exhaling. These adverse effects can lead to poor sleep quality and disruptions, potentially reducing patient adherence to CPAP treatment (16, 18). In cases where treatment intolerance arises due to side effects, complementary therapies like acupuncture may be considered. In summary, acupuncture is an effective and safe treatment for OSA, offering affordability and a high success rate.
A recent meta-analysis, based on 19 studies involving 1365 participants, revealed statistically significant changes in various indicators, including the apnea-hypopnea index, LSpO2, ESS, interleukin-6, tumour necrosis factor-alpha (TNF-α), and nuclear factor-kappa B (NF-κB) (44).
5. Mechanism of Action
The specific physiological or biochemical pathways through which acupuncture improves sleep quality are not well understood. However, several studies have demonstrated that acupuncture can trigger various physiological responses (45). According to a review paper, needling stimulation and EA may activate the neurological system, neurotransmitters, and endogenous chemicals, potentially mediating pain relief and other therapeutic effects (46). In studies involving rats, acupuncture was found to stimulate the opioidergic system, leading to increased levels of beta-endorphin, which could have a sleep-promoting effect (47). Acupuncture has also been shown to enhance the release of melatonin, a hormone associated with improved sleep (48, 49). By increasing melatonin secretion, acupuncture can reduce nighttime insomnia and anxiety. The deficiency of melatonin may be a key factor in anxiety-related insomnia, and acupuncture acts by promoting melatonin production in the pineal gland and the hippocampus (48).
Furthermore, certain acupoint stimulation has been found to elevate nitric oxide levels in the brain and blood, which has been linked to improved sleep in clinical studies (50).
Most of the studies have focused on the use of REN23 as a commonly applied acupoint. REN23, located in the larynx, sits at the intersection of yin and yang meridians. Beneath this acupoint lie branches of the sublingual and glossopharyngeal nerves. Pressure on this acupoint can reduce oral cavity constriction and stabilize it while strengthening its muscles through direct stimulation of the submandibular and glossopharyngeal nerves (51).
Acupuncture can also lead to an increase in the inhibitory neurotransmitter gamma-aminobutyric acid (GABA), which can contribute to better sleep (52). Additionally, acupuncture has an impact on the autonomic nervous system, influencing both the sympathetic and parasympathetic systems, which may explain its sleep-inducing properties (52).
EA has been extensively used in clinical and fundamental research as an alternative to MA. However, the underlying mechanisms of EA and MA may differ to some extent. EA promotes the release of both beta-endorphin and adrenocorticotrophic hormone (ACTH) into the plasma, whereas MA primarily releases beta-endorphin (53, 54). According to Sugai et al., after treatment, the MA and 10 Hz EA groups showed significant differences from both the 2 Hz EA and control groups in all polysomnographic parameters, particularly in the key outcome, AHI. Sugai et al. attributed this improvement to the involvement of serotonergic pathways in acupuncture-mediated responses, as well as its anti-inflammatory activity (55, 56).
The central mechanism responsible for reducing the activity of airway dilator muscles during sleep is not fully understood. However, it has been demonstrated that caudal raphe serotonergic neurons are strongly projected to upper airway motor neurons at night, and the firing of caudal raphe neurons decreases, especially in REM sleep, resulting in reduced respiratory muscle tone (57). Consequently, impaired serotonin-mediated stimulation of excitatory neurons in the caudal raphe may lead to reduced upper airway motor activity associated with sleep in OSAS patients. Studies have shown that L-tryptophan, a serotonin precursor and a serotonin reuptake inhibitor, can be administered to address this issue (58).
Additionally, acupuncture has been shown to regulate different neurotransmitters, including endorphins, serotonin, norepinephrine, ACTH, cortisol, acetylcholine (Ach), melatonin, substance P, other neuropeptides, and nitric oxide, as well as endocrine factors, in both basic science and clinical trials. All of these play significant roles in sleep regulation (52).
The regulation of neurotransmitters by acupuncture is complex and can exert opposite effects depending on the locations of acupoints and techniques used in clinical applications. For instance, ACTH levels can be elevated when CV-4 (Guanyuan) is stimulated with moxibustion (heating of acupoints) to improve immunity but can be suppressed when acupuncture is used to treat addiction in heroin addicts (52, 59).
6. Neurophysiological Pathways of Acupuncture
Based on a series of studies on the neurophysiological consequences of acupuncture, the neurophysiological pathways of acupuncture have become clearer. Sensory signals follow the spinothalamic tracts to the thalamus and then to the primary sensory cortex, transmitted via sympathetic nerves. Neurons within these ascending tracts synapse with motor neurons that activate various organs of the respiratory system, including the diaphragm, nose, larynx, scalene muscles, trachea, lungs, intercostal muscles, and supporting abdominal muscles (59, 60).
The sensory signals at the neocortex are subsequently relayed to motor neurons in the primary motor cortex. These activated neurons primarily project along two descending tracts: the anterior and lateral corticospinal tracts. Neurons within these tracts project to once again activate various respiratory organs, as well as motor neurons related to the digestive system, including the large intestine. Through interneuron relay, these neurons synapse with motor neurons that mobilize the organs of the respiratory and digestive systems to function (60, 61).
7. Side Effects of Acupuncture
Several adverse effects were described in the most recent systematic review conducted by Xu et al., including syncope, organ or tissue injury, systemic reactions, infection, erythema, neuromuscular disease, aggravation of symptoms, skin allergy reactions, swelling, numbness, and other adverse events related to acupuncture. However, no adverse events were reported in any of the trials related to acupuncture for OSA (51).
8. Conclusions
Acupuncture appears to be a potentially effective and safe therapy option for patients with OSA. It may help improve patients’ LSpO2 levels and reduce their AHI and ESS, particularly benefiting those with moderate to severe OSA. This evidence could be valuable for medical practitioners, patients, and healthcare policymakers considering the use of acupuncture in managing OSA.
In future studies, it is advisable to consider secondary outcomes such as polysomnography (PSG) results, sleep quality, emotional well-being, and cognitive function during sleep. Additionally, to assess neuroplasticity changes, including gray matter density, white matter integrity, and functional connections, fMRI scans could be conducted before and after acupuncture treatment (52, 58).
However, it's important to note that methodological limitations in many trials within this field may restrict the extent of conclusions and potentially exaggerate the clinical efficacy of acupuncture therapy. Nonetheless, acupuncture can be a valuable addition to other treatment approaches for addressing sleep challenges and improving sleep efficiency (62). The absence of blinding techniques in randomized controlled trials (RCTs) could potentially influence the study outcomes. Moreover, acupuncture has the potential to generate strong placebo effects (40, 63). Therefore, to establish the effectiveness and safety of acupuncture for patients with OSA, further high-quality RCTs are warranted.