1. Background
Providing a secure airway is fundamental to safe anesthetic practice and is critical for patients undergoing general anesthesia. Although most airway management procedures are uncomplicated, a small proportion may encounter difficulties. Complications during difficult intubation can lead to particularly adverse events such as hypoxemia, aspiration, airway trauma, brain damage, and even death (1).
Difficult tracheal intubation (DTI) is described as more than two attempts lasting more than 10 minutes each or requiring an alternative technique (2). DTI results from a multifaceted interaction of patient anatomy, clinical circumstances, and clinician skills (3). Various assessment methods have been proposed as predictors of DTI during preoperative clinical examination. The most comprehensive methods for evaluating DTI include the Cormack-Lehane system, thyromental distance (TMD), Mallampati score, mouth opening (MO), Upper lip bite test combined with sternomental distance, and body mass index (BMI). However, the sensitivity and reliability of these methods are low (3-5). Khan et al., in a prospective study, investigated whether combining different methods or creating a composite score could improve the ability to predict easy intubation compared to each test alone. They suggested that using a combination of assessment methods provided higher sensitivity (4).
Studies have shown that DTI occurs more frequently in obese patients (6-9). Obese patients typically have shorter and thicker necks, larger tongues, and excessive laryngeal tissue, necessitating assessment before any airway management (7, 10, 11). Additionally, a study identified the presence of a non-compliant submental space as indicative of difficult intubation (12).
To the best of our knowledge, none of the existing methods utilize neck submental fat as a quantitative predictive value for DTI.
2. Objectives
Considering the points raised above, we conducted a prospective study to evaluate the predictive value of neck submental fat diameter for difficult tracheal intubation as a new method. We also compared our results with the predictive values of other techniques, including the Mallampati score, Upper lip bite test, TMD, and neck movements. We hypothesized that increased submental fat would increase the difficulty of tracheal intubation. The effect of submental fat on intubation difficulty was considered the primary outcome of this study.
3. Methods
This cross-sectional study was conducted after obtaining approval from the Tehran University Research Ethics Board (IR.TUMS.MEDICINE.REC.1389.103). Two hundred and fifty adult patients (> 18 years of age) requiring tracheal intubation before elective surgery in the general surgery operation rooms of Shariati Hospital were included in the study from March 2018 to March 2019. Informed consent was obtained from all patients.
Patients with a BMI of more than 29 or less than 22, cervical spine or maxillofacial abnormalities, emergency procedures, known difficult intubation or upper airway disease, history of peritonsillar abscess, neck or thyroid masses, and pregnant individuals were not included in the study.
Patients were evaluated preoperatively by an anesthesiology resident. A complete medical history was obtained, including sex, age, surgical indication, comorbidities, and medications.
Patients' height and weight were measured, and BMI was calculated using these measurements.
Airway parameters, including the Mallampati score, mandibular protrusion, Cormack-Lehane score, Upper lip bite test, TMD, and neck movement (measured in centimeters), were assessed using a ruler and documented (11, 13). In the recovery room, patients' necks were carefully examined. Submental fat at the level of the thyroid cartilage was measured using a digital caliper. Preoperative investigations followed the institution's standard practices.
All patients were monitored using electrocardiogram (ECG), pulse oximetry, and noninvasive arterial blood pressure measurement. To facilitate intubation, patients were positioned with a Troop elevation pillow (Trudell Medical Inc, London, Ontario, Canada) to align the suprasternal notch with the external auditory meatus. All patients achieved an end-tidal oxygen concentration of more than 85% by receiving pre-oxygenation for at least 3 minutes pre-induction. General anesthesia was induced with fentanyl 3 µg/kg, midazolam 1 mg/kg, propofol 2 mg/kg, and cisatracurium 0.2 mg/kg to facilitate tracheal intubation. Muscle relaxation was monitored by TOF stimulation. Tracheal intubation was performed using direct laryngoscopy with a proper-sized Macintosh blade once all four responses to TOF stimulation were eliminated. Adjuncts to the blade were utilized if difficulties were encountered during intubation.
The anesthesiologists who intubated patients had at least five years of clinical experience in airway management. In this study, Cormack-Lehane classes III or IV were considered indicative of difficult intubation. Successful tracheal intubation was confirmed by observing the proper capnograph waveform.
3.1. Statistical Analysis
The Pearson chi-square test and Fisher exact test were used to compare each pre-operative parameter between the 2 groups of patients with easy or difficult intubation. Age and submental fat were compared between the two groups using the Mann-Whitney test.
Pre-operative parameters were classified into binary variables to find the best logistic regression model for predicting difficult intubation (Table 1). Univariate logistic regression was performed to assess the relationship between the pre-parameters and the difficulty of intubation. The multivariate logistic regression model was selected based on the best model fit and the lowest Akaike Information Criterion (AIC). To evaluate the discrimination ability of the models, receiver operating characteristic (ROC) curves were plotted, and the area under the curve (AUC) was calculated. McFadden's pseudo-R squared of logistic regression models is reported to compare the best model fit.
| Variables | Classification |
|---|---|
| MO groups 0;1 | MO ≤ 3MO > 4 |
| TMD groups 0;1 | TMD ≤ 2TMD = 3 |
| MP groups 0;1 | MP ≤ 2MP > 2 |
| JM groups 0;1 | JM = 1JM > 1 |
All statistical analyses were performed using Stata 14 (StataCorp. 2015. Stata Statistical Software: Release 14. College Station, TX: StataCorp LP).
4. Results
There were 250 patients in this study, comprising 132 (53%) males and 118 (47%) females. The median age of the patients was 43.5 years (range 18 - 72). Table 2 presents the demographic and preoperative characteristics of the patients, including those with and without difficult intubation, along with the P-values for the comparison of each variable between the two groups. Among our study population, 48 patients (19%) experienced difficult intubation. The median submental fat of the study population was 21 mm (IQR 15, 25). The Mann-Whitney test revealed a significant difference in submental fat between the 2 groups based on intubation difficulty (P-value < 0.001) (Figure 1).
| Variables | All Patients; N = 250 | Easy Intubation; N = 202 | Difficult Intubation; N = 48 | P-Value |
|---|---|---|---|---|
| Sex | 0.59 | |||
| Male | 132 (52.8) | 105 (52.0) | 27 (56.3) | |
| Female | 118 (47.2) | 97 (48.0) | 21 (43.8) | |
| Age, median (IQR) | 43.5 (29, 58) | 43.5 (29, 57) | 44 (30, 61) | 0.85 |
| Mouth Opening | < 0.001 | |||
| 3 | 68 | 55 | 58% | |
| 4 | 32 | 45 | 42% | |
| Tyro-mental distance | < 0.001 | |||
| < 6cm | 31 (12.4) | 0 (0.0) | 31 (64.6) | |
| 6cm | 117 (46.8) | 104 (51.5) | 13 (27.1) | |
| > 6cm | 102 (40.8) | 98 (48.5) | 4 (8.3) | |
| ULBT | 0.012 | |||
| Class I | 79 (31.6) | 72 (35.6) | 7 (14.6) | |
| Class II | 99 (39.6) | 74 (36.6) | 25 (52.1) | |
| Class III | 72 (28.8) | 56 (27.7) | 16 (33.3) | |
| MP | < 0.001 | |||
| Class I | 90 (36.0) | 85 (42.1) | 5 (10.4) | |
| Class II | 66 (26.4) | 65 (32.2) | 1 (2.1) | |
| Class III | 57 (22.8) | 34 (16.8) | 23 (47.9) | |
| Class IV | 37 (14.8) | 18 (8.9) | 19 (39.6) | |
| JM | < 0.001 | |||
| 1 | 47 (18.8) | 3 (1.5) | 44 (91.7) | |
| 2 | 131 (52.4) | 127 (62.9) | 4 (8.3) | |
| 3 | 72 (28.8) | 72 (35.6) | 0 (0.0) | |
| Neck ROM | < 0.001 | |||
| > 90° | 202 (80.8) | 202 (100.0) | 0 (0.0) | |
| < 90° | 48 (19.2) | 0 (0.0) | 48 (100.0) | |
| Sub-mental fat, median (IQR) | < 0.001 | |||
| PMH | 21 (15, 25) | 19 (14, 23) | 26 (24, 28.5) | 0.21 |
| No | 52 (20.8) | 41 (20.3) | 11 (22.9) | |
| DM | 60 (24.0) | 47 (23.3) | 13 (27.1) | |
| CVD | 75 (30.0) | 60 (29.7) | 15 (31.3) | |
| Thyroid disorders | 40 (16.0) | 37 (18.3) | 3 (6.3) | |
| Coagulopathies | 14 (5.6) | 9 (4.5) | 5 (10.4) | |
| Stroke | 9 (3.6) | 8 (4.0) | 1 (2.1) |
The results of univariate and multivariate logistic regression analyses for the association between difficult intubation and other variables are depicted in Table 3. Based on the best subset variable selection, submental fat, TMD (model 1) (Figure 2), and age (model 2) were chosen to participate in the multivariate regression model. Each one mm increase in neck fat was shown to increase the odds of difficult intubation by 30% (P-value < 0.001) in the univariate logistic model. After adjusting for MO, TMD, and age, the odds of difficult intubation were approximately 2 times higher in patients with 1 mm more neck fat (P-value 0.007).
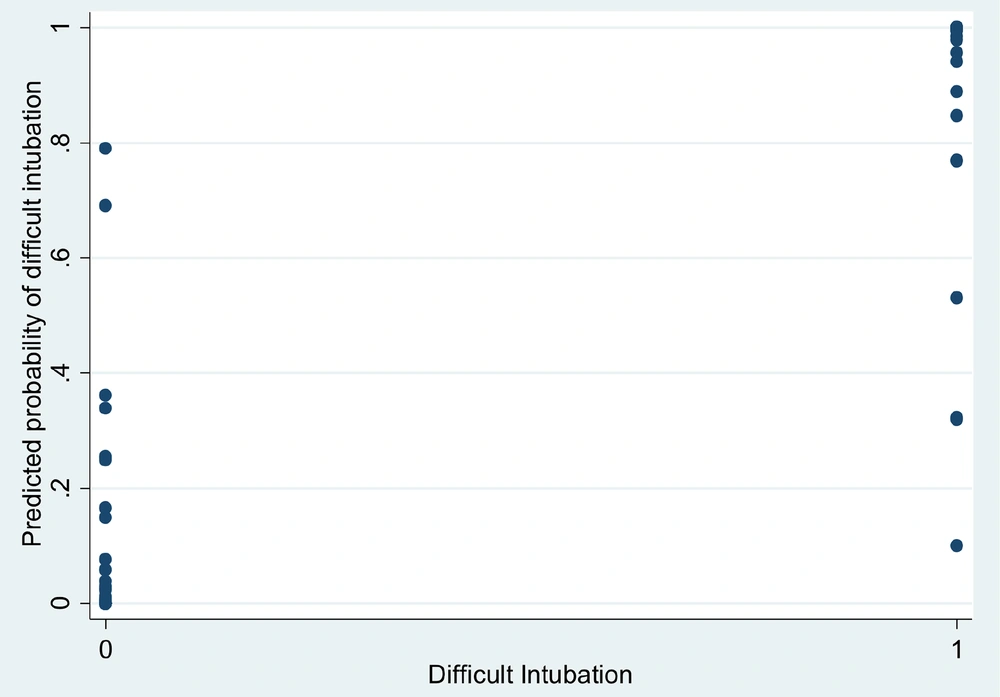
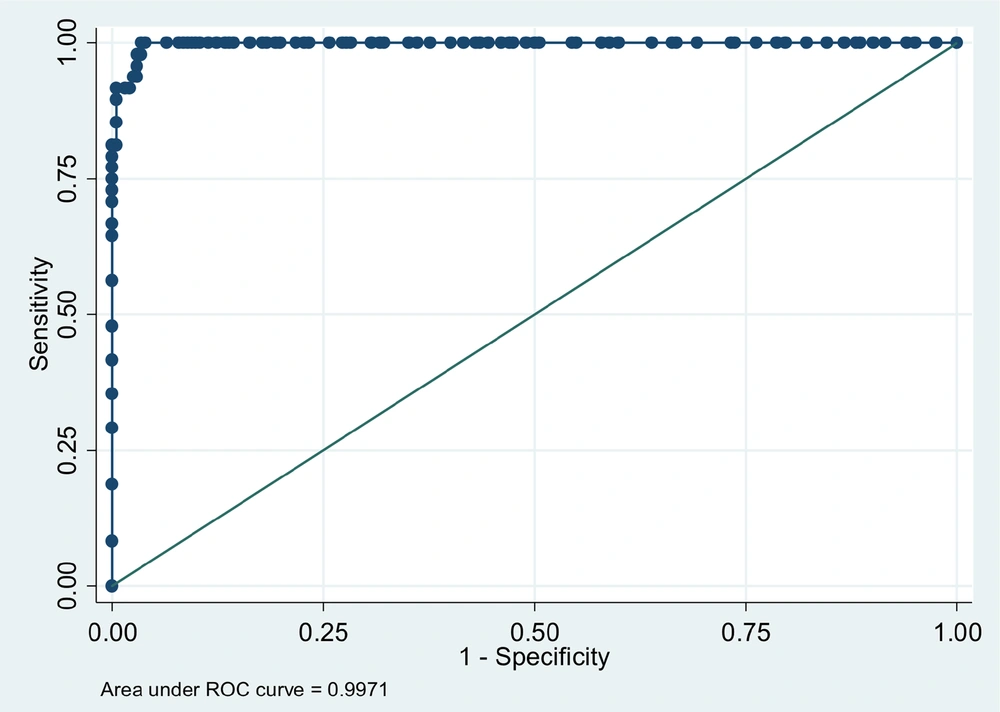
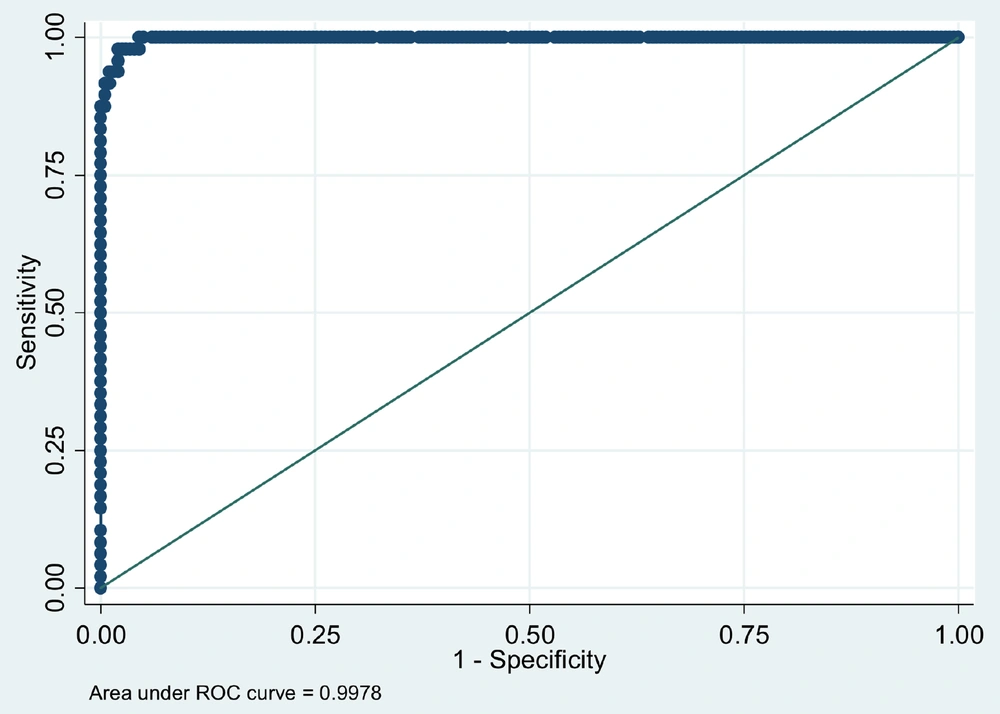
The multivariate model improved the model fit for predicting the probability of difficult intubation. Table 4 displays the Akaike Information Criterion (AIC), the area under the curve (AUC) of the ROC curve, and McFadden's pseudo-R squared of the univariate and multivariate models of selected variables. Figure 3 illustrates the probability of difficult intubation calculated by the multivariate logistic regression, incorporating the mentioned variables, compared to the actual intubation difficulty outcome. The AUC of the ROC curve and McFadden's pseudo-R squared of the multivariate model were 0.998 and 0.91, respectively (Figures 4 and 5).
| Variables | Univariate Analysis | Multivariate Analysis (Model 1) | Multivariate Analysis (Model 2) | |||
|---|---|---|---|---|---|---|
| Predictors | OR | P-Value | OR | P-Value | OR | P-Value |
| Age | 1.00 | 0.80 | 0.91 | 0.05 | ||
| Gender | 0.84 | 0.56 | ||||
| Sub-mental fat | 1.30 | < 0.001 | 1.59 | 0.005 | 1.98 | 0.007 |
| MO group | 0.001 | < 0.001 | 0.0002 | < 0.001 | 8*10-6 | 0.003 |
| TMD group | 0.10 | < 0.001 | 0.04 | 0.04 | 0.003 | 0.02 |
| MP Group | 20.19 | < 0.001 | ||||
| JM Group | 0.0013 | < 0.001 | ||||
| ULB | ||||||
| Class II VS. I | 3.47 | 0.007 | ||||
| Class III VS. I | 2.94 | 0.027 | ||||
| Model With | AIC | Pseudo R Squared | AUC of ROC Curve |
|---|---|---|---|
| Sub-mental fat | 191.66 | 0.23 | 0.83 |
| MO group | 65.65 | 0.75 | 0.95 |
| TMD group | 217.88 | 0.13 | 0.70 |
| Model 1 | 37.87 | 0.89 | 0.997 |
| Model 2 | 34.67 | 0.91 | 0.998 |
5. Discussion
The results of our study revealed that the probability of DTI increased in patients with greater submental fat. When incorporating this variable with other measures for predicting difficult intubation in both univariate and multivariate analyses, favorable odds ratios were observed. In the univariate model, each 1 mm increase in submental fat was associated with a 30% increase in the odds of difficult intubation. After adjusting for MO, TMD, and age, the odds of airway difficulty reached approximately 60%. The pseudo-R squared of the multivariate model was high, with values of 0.998 and 0.91 for models 1 and 2, respectively.
As mentioned previously, we were unable to find any manuscripts directly comparing airway difficulty with submental fat. Only in a study conducted by Javid (12), it was concluded that the presence of a non-compliant submental space was correlated with difficult intubation and ventilation, termed the "positive submental sign." However, this study offered a non-quantitative index for the prediction of difficult airway management. Additionally, while the submental sign was associated with the Cormack-Lehane classification, it did not provide predictive criteria for difficult intubation. Consequently, there is a lack of confirmed studies regarding the submental sign.
There is no single variable that effectively predicts difficult intubation. Some traditional measures, such as the Mallampati classification, were found to be unreliable. In a study, the reliability of predicting DTI increased when using several variables (3-5) together; however, the results varied. Other measures such as the Upper Lip Bite Test (ULBT), neck range of motion, neck circumference, and thyromental distance are useful tools, but they should be used together to enhance the sensitivity and specificity of predicting a difficult airway. In our study, by incorporating submental fat diameter with other predictors, the ability to predict DTI increased significantly.
This study had several limitations. Firstly, obese patients (BMI > 29) were excluded, which could affect the generalizability of the results to this population. Conducting a study specifically on obese patients could validate the findings of the present study in this demographic. Additionally, the exact volume of submental fat might serve as a better predictor of DTI than the diameter of submental fat measured in this study. An ongoing study utilizing ultrasound to measure submental fat volume more accurately may shed further light on this aspect. However, it is worth noting that using ultrasound for this purpose may be more challenging and time-consuming than measuring fat diameter, and a cost-benefit analysis of employing ultrasound should be considered in future investigations.
Future studies could aim to validate the results of the present study or compare DTI with submental fat in conjunction with other airway difficulty measurements. Furthermore, exploring DTI and submental fat in different head positions could provide valuable insights.
5.1. Conclusions
There is a significant association between submental fat and DTI. Therefore, we recommend measuring submental fat before administering general anesthesia to mitigate the risk of encountering an unpredicted difficult airway.
![Difficult intubation probability calculated by multivariate logistic regression vs. the actual difficulty (0 = easy intubation, 1 = difficult intubation) [model 1] Difficult intubation probability calculated by multivariate logistic regression vs. the actual difficulty (0 = easy intubation, 1 = difficult intubation) [model 1]](https://services.brieflands.com/cdn/serve/3170b/9d4196e8624dcfdda2d9c7f30eb6cea903f740da/ans-144272-i002-F2-preview.webp)
![Difficult intubation probability calculated by multivariate logistic regression vs the actual difficulty (0 = easy intubation, 1 = difficult intubation) [model 2] Difficult intubation probability calculated by multivariate logistic regression vs the actual difficulty (0 = easy intubation, 1 = difficult intubation) [model 2]](https://services.brieflands.com/cdn/serve/3170b/1b2dedc7030d8b4d3e57e86dc4c07c5768799a61/ans-144272-i003-F3-preview.webp)