1. Background
Epilepsy is one of the oldest disorders known to mankind and is currently considered one of the most common neurological disorders. Epilepsy is a common neurological disorder that affects both children and adults. Epilepsy is characterized by recurrent and unprovoked seizures, in which a limited or extensive area of the brain shows spontaneous activity, and the proper functioning of the brain is disturbed (1, 2).
Epilepsy consists of different types and includes primary generalized epilepsy, simple focal epilepsy, and complex epilepsy with secondary diffusion. Although many drug treatments are prescribed for epilepsy, a percentage of these patients still suffer from epileptic attacks, even with the use of multiple drugs (3). Sudden unexpected death in epilepsy is one of the complications of epilepsy, which is more common in adults and individuals with long-term epilepsy (4).
Post-traumatic epilepsy (PTE) can occur at any age (5). Population aging causes problems in the field of demographics, diagnosis, and management of epilepsy; accordingly, individuals over 60 years of age, among all age groups, have a higher prevalence of epileptic attacks with acute symptoms and stable epilepsy (6). On the other hand, it is difficult to make an accurate clinical diagnosis due to the increase in the elderly population in the world and Iran (7, 8) and the difficulty of taking the age history in this age group (9). Additionally, children are more vulnerable due to their special age conditions and are vulnerable to all kinds of diseases (10, 11). Post-traumatic epilepsy is one of the causes of disability in children with traumatic brain injury (TBI), which occurs in about 10-20% of children after severe TBI (12). Epilepsy reduces the quality of life, self-esteem, and academic progress and causes social isolation and post-traumatic stress symptoms in children and their families (13, 14).
Post-traumatic epilepsy is one of the types of epilepsy, which is a complication of TBI that occurs after TBI or 7 days later. Post-traumatic epilepsy leads to a change in the quality of life, and the patient raises questions regarding the PTE recurrence rate, prediction of PTE risk factors, reduction of the PTE incidence rate, and PTE treatment (15, 16). Factors such as injury severity, post-traumatic amnesia, loss of consciousness, age, treatment methods, gender, and neuroimaging results are effective in causing PTE and can act as effective factors (15, 17, 18).
The TBI prevalence in the world and Iran is high, and TBI can affect the quality of life or even the survival of patients by causing complications such as PTE (19-21).
In a study by Amit Thapa et al. (22) entitled “Post-traumatic seizures: A prospective study from a tertiary level trauma center in a developing country”, they observed that PTE affects mainly young adults of the male gender. Road traffic accident is by far the leading mechanism of injury, leading to severe TBI in about two-thirds of cases. Contusions and epidural hematoma were the most common brain lesions on imaging. Generalized tonic-clonic seizures are the most frequent clinical seizure type. Despite the limited choice in antiseizure medications, seizure freedom was achieved in about two-thirds of patients after 2.5 years of follow-up. Further studies need to be performed to assess the long-term outcome and other clinical features of PTE, such as neuropsychological consequences and dissociative seizures (23).
2. Objectives
The present study aimed to determine the risk factors for PTE in patients with TBI.
3. Methods
This retrospective study investigated the computed tomography (CT)-scan results of all TBI patients admitted to Imam Khomeini hospital of Ilam, Iran (April to March 2016). The inclusion criteria included all patients over 20 years with TBI who were admitted to the emergency department of the hospital within 24 hours and underwent a CT-scan procedure. The exclusion criteria also included patients with multiple traumata, systemic and chronic disease, diabetes, endocrine disorders, bleeding disorders, pregnancy, chronic heart failure, history of epilepsy, and use of anticonvulsants. The data were collected using a checklist, including questions on age, gender, education, marriage, trauma mechanism, and CT scan findings (Tables 1 -4).
At first, initial evaluation, including the examination of airways, vital signs, and breathing, was performed, and the level of consciousness was checked according to the Glasgow Coma Scale (GCS) for all traumatic patients. Traumatic brain injury was confirmed based on history, state of consciousness, and CT scan, which was performed for all patients by the same machine. Then, the results of all CT scans were evaluated by a neurologist. If the patient had PTE, she/he was included in the study.
Obtaining the code of research ethics and keeping the patients’ information confidential were among the ethical principles in the study.
3.1. Data Collection Procedure
The Glasgow Coma Scale is a tool that measures the patient’s state of consciousness in 3 areas: Eye-opening and motor and verbal responses. The score is between 3 and 15 (23).
3.2. Data Analysis Procedure
Data analysis was carried out using descriptive statistics in SPSS software (version 16).
4. Results
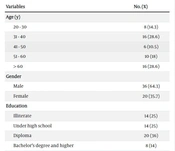
According to the results, mild, moderate, and severe GCS scores were reported in 8 (14.3%), 30 (52.5%), and 18 (32.2%) participants, respectively. Most of the patients were in the age range of 31-40 years (n = 16, 28.6%), male (n = 36, 64.3%), and married (n = 34, 60.7%) (Table 1). There was also a significant relationship between TBI severity and PTE status.
| Variables | No. (%) |
|---|---|
| Age (y) | |
| 20 - 30 | 8 (14.3) |
| 31 - 40 | 16 (28.6) |
| 41 - 50 | 6 (10.5) |
| 51 - 60 | 10 (18) |
| > 60 | 16 (28.6) |
| Gender | |
| Male | 36 (64.3) |
| Female | 20 (35.7) |
| Education | |
| Illiterate | 14 (25) |
| Under high school | 14 (25) |
| Diploma | 20 (36) |
| Bachelor’s degree and higher | 8 (14) |
| Marital status | |
| Single | 22 (39.3) |
| Married | 34 (60.7) |
Vehicle accidents were the main cause of TBI (n = 34, 60%), and the lowest TBI rate was due to other cases (n = 4, 7.2%) (Table 2).
| Mechanism of Trauma | No. (%) |
|---|---|
| Vehicles | 34 (60) |
| Falling from a height | 12 (21.5) |
| Strikes | 6 (10.3) |
| Other cases | 4 (7.2) |
| Total | 56 (100) |
The most and least frequent CT-scan findings were epidural hemorrhage (EH) (n = 24, 42.3%) and midline shift and intracerebral hemorrhage (n = 6, 10.8%) (Table 3).
| CT Scan Findings | No. (%) |
|---|---|
| Epidural hemorrhage (EH) | 24 (42.3) |
| Subarachnoid hemorrhage (SH) | 18 (32.2) |
| Subarachnoid hemorrhage | 14 (25) |
| Intracerebral hemorrhage | 6 (10.8) |
| Skull fracture | 10 (17.9) |
| Diffuse brain injury (DAI) | 12 (21.5) |
| Intracranial fracture | 8 (14.3) |
| Intracranial hemorrhage | 10 (17.9) |
| Normal | 2 (3.5) |
A total of 24 patients (42.3%) had tonic epilepsy, and 10 patients (17.9%) had epilepsy duration of more than 10 minutes (Table 4).
| Variables | CT Scan Findings | No. (%) |
|---|---|---|
| Seizure type | Tonic | 24 (42.3) |
| Clonic | 18 (32.2) | |
| Tonic-clonic | 8 (14.3) | |
| Seizure duration | Less than 5 minutes | 6 (10.8) |
| 5-10 minutes | 6 (10.8) | |
| More than 10 minutes | 10 (17.9) |
5. Discussion
There are different types of traumata, including vascular trauma (24), spinal trauma (25), orthopedic trauma (26), and TBI (27). Traumatic brain injury is defined as a trauma that affects brain function in the form of dizziness, epilepsy, coma, and loss of consciousness. Traumatic brain injury can be penetrating or non-penetrating (27, 28).
Considering the importance of neurosurgical diseases in the patient’s life, effective prevention, diagnosis, and treatment measures should be taken (29-31). The disease process is effective in causing acute and chronic complications for patients (32, 33).
The reported TBI incidence rate in the USA, Europe, Australia, and the Middle East is 538.2, 235, 322, and 45 cases per 100 000 individuals, respectively (34-37). Additionally, the reported TBI incidence rate among American 0-4-year-old children and older adults was equal to 1 188 and 234 per 100 000 individuals, respectively (38). Ahadi et al. reported in a study in Tehran, Iran, that the TBI incidence rates were 31.5% and 12.3% in the 21-30 and 41 - 50 age groups, respectively (39). Due to the high TBI incidence rate, various complications, such as PTE, are caused (40).
The most and least frequent CT-scan findings were EH (n = 24, 42.3%) and midline shift and intracerebral hemorrhage (n = 6, 10.8%), respectively. In Ahadi et al.’s study, concussion, diffuse brain injury (DAI), subarachnoid hemorrhage (SH), and EH occurred in 14 (0.4), 1 018 (26.7%), 551 (14.4), 787 (20.6), 1 018 (26.7%) participants, respectively (39). In Brown et al.’s study, SH, EH, and DAI rates were equal to 28%, 11%, and 2%, respectively (41). Additionally, in a study by Sødal et al., CT scan findings showed brain contusion, SH, EH, and skull fracture in 63%, 75%, 15%, and 49% of patients with confirmed PTE, respectively (42), which is consistent with the findings of the present study that suggests CT involvement of PTE patients.
5.1. Conclusions
The most frequent risk factors included vehicles, falling from a height, and strikes, respectively. Additionally, the most common CT scan findings included EH and SH. Motor vehicle accidents account for the highest rate of TBI-related PTE. For this reason, it is necessary to take preventive measures in this regard.