1. Context
Frontotemporal Dementia (FTD) is a clinical syndrome marked by progressive neurodegeneration, characterized by deteriorating behavior, executive function, and language capabilities. It ranks as the third most prevalent form of dementia, following Alzheimer's disease and Lewy body dementia, across all age groups and represents the primary type of dementia within a diverse group of disorders (1-3). Primary progressive aphasia (PPA) involves degeneration in the temporal and frontal cortices and the pre-Sylvian brain area (4, 5). Typically manifesting between the ages of 50 and 60, language difficulties, particularly naming dysfunction, emerge as early clinical signs (6). This issue is commonly observed in the disease's initial stages, serving as a crucial indicator for early identification and intervention in PPA (7). As the disease advances, other language abilities, including grammar, comprehension, and repetition, are also affected (6).
Based on current diagnostic criteria and clinical manifestations, PPA is classified into three variants: The logopedic variant PPA (lvPPA), the nonfluent/agrammatic PPA (nfaPPA), and the semantic variant PPA (svPPA). This classification is determined by clinical (syndromic) characteristics, supported by neuroimaging findings and underlying neuropathology (8).
Fluent speech, a disorder in semantic memory, and impaired comprehension of single words characterize the semantic variant (svPPA). Atrophy in this variant is typically observed in the anterior parts of the temporal lobes. The nonfluent/agrammatic variant (nfaPPA) is marked by effortful, halting speech (nonfluent speech) with grammatical errors and omissions, relatively good comprehension of sentences, a likelihood of motor speech disorders such as dysarthria or verbal apraxia, and atrophy in the inferior frontal gyrus, prefrontal areas, primary motor cortex, and posterior regions of the temporal lobe. The logopedic variant (lvPPA) manifests through a slow rate of spoken language, pauses due to word-finding difficulties, and an absence of frank agrammatism, with associated atrophy in the temporal-frontal cortex (9).
Although most individuals with PPA can be categorized into one of these three variants, a minority does not fit neatly into any category. This group exhibits mixed features or a singular language symptom, such as anomia or dyslexia, persisting over an extended period (10).
Regarding the treatment of PPA, it is noted that no pharmacological therapies exist to improve or stabilize the language deficits associated with this syndrome, leading to inevitable progression over time (11). However, recent studies suggest that individuals with PPA retain the capacity for language learning, indicating that language treatment may enhance neuroplasticity in PPA.
Since the primary issue in this syndrome is language disorders, particularly naming impairment, speech and language pathologists play a crucial and essential role in its management and rehabilitation. Evidence supports the effectiveness of language interventions in slowing the disease's progression and helping maintain the independence of individuals with progressive aphasia over the long term (5, 8). These interventions can enhance their quality of life and their level of activity and engagement (2).
In total, four types of treatments are utilized in PPA: (a) lexical retrieval treatment, (b) phonological and/or orthographic treatment, (c) semantic treatment, and (d) multimodality approach treatment (9).
Lexical retrieval treatments aim to reduce difficulties in word finding, particularly for words significant to the individual (12). This treatment employs a hierarchy of tasks designed to strategically utilize remaining semantic, orthographic, and phonological knowledge. Various treatments, such as lexical retrieval cascade treatment, repetition and reading in the presence of a picture (RRIPP), look, listen, repeat (LLR) treatment, errorless learning, and the cuing hierarchy approach, have been identified as effective for lexical retrieval (9).
Semantic treatment is considered a superior approach. Depending on the variant of the disorder, semantic interventions strive to strengthen the connections between the structural, cognitive, and functional aspects of items, either through retrieval or enhancement of information networks that facilitate communication. This treatment method is particularly suitable for patients with svPPA, who experience deficits in semantic memory (13).
Phonological and/or orthographic treatment focuses on facilitating word retrieval by activating residual phonology and enhancing the phonological retrieval of words by strengthening their orthographic representations (14).
The multimodality stimulation approach combines various language exercises and strategies to improve communicative independence (15). Several treatment methodologies have been utilized in this context. Farrajota et al. reported that integrating different practices, such as naming images, describing actions depicted in pictures, comprehending complex verbal-auditory tasks, reading and writing, facilitating the expression of feelings and opinions, and enhancing conversational skills, could improve naming abilities and influence speech in patients with nfvPPA (15).
In treating svPPA, strategies to bolster semantic, phonetic, and written representations are employed. Some studies focusing on these representations aim at facilitating re-learning (12). Errorless Learning, based on the principles of learning memory, is one of the therapeutic approaches used. Employing this method has shown improvement in naming for the cases trained in this group (16).
Although limited, lexical retrieval studies focusing on the lvPPA variant have shown promising results. Techniques to enhance lexical retrieval in the Logopenic variant involve semantic, phonetic, and/or written cues (12).
Pagnoni conducted a systematic review in 2021, analyzing 48 studies on language treatment that focused on enhancing written and oral naming abilities from 2004 to 2020. The findings from this comprehensive review indicate that various treatment approaches are effective for individuals with PPA, and language training can significantly improve naming abilities across all variants of PPA (9).
In addition to language interventions, there is no evidence supporting the effectiveness of noninvasive brain stimulation (NIBS) in reducing verbal difficulties in patients with PPA. Research has shown that Transcranial Direct Current Stimulation (tDCS) is effective in enhancing lexical retrieval in these patients (17-20).
tDCS is a noninvasive approach based on the principle of neuroplasticity, wherein a weak direct current (1 to 3 mA) is applied to the scalp. This current can alter the resting potential of neurons in the targeted regions. The device uses two electrodes: an anode and a cathode. In most research, areas beneath the anode are activated, while those under the cathode are inhibited. Several studies have found that brain stimulation with direct current improves cognitive function in individuals with dementia. A majority of these studies have combined tDCS with language interventions (21). The evidence suggests that combining tDCS with language therapy yields positive outcomes (6). However, the sustainability and generalizability of tDCS results in PPA remain to be fully understood, indicating the need for further research (22).
2. Objectives
The current study aimed to compile all methods utilized in treating variants of progressive aphasia, a topic of critical importance as Iran undergoes demographic changes and its population ages. According to the 2016 census, the middle-aged population (30 to 64 years) constituted 44.8%, equating to 35.8 million people, while the elderly population (65 years and older) accounted for 6.1%, or 4.9 million people (23). International projections suggest that Iran's senior population will experience a more significant increase from 2036 compared to other regions of the world and even the global average, surpassing the world's average population growth by 2115 and outpacing Asia by nine years (24). With these shifts in the population pyramid, the prevalence of age-related conditions, such as dementia, is expected to rise (25). Speech therapists are likely to encounter PPA more frequently in the future and should thus be well-informed about it. Consequently, this study will gather various treatment methods, including both language and tDCS interventions, assess the level of evidence for these methods, and assist language and speech therapists in identifying the most effective treatment approach.
3. Mythology
3.1. Search
The systematic review was carried out by searching the Cochrane Library, PubMed, Scopus, Web of Science, Science Direct, and ProQuest databases from January 1, 2010, to December 31, 2022. Keywords used for this study included: (primary progressive aphasia OR semantic dementia OR frontotemporal dementia) AND (language training OR language treatment OR anomia training OR treatment for lexical retrieval OR anomia treatment OR word retrieval therapy) AND (transcranial direct current stimulation).
3.2. Selection Criteria
The PICO approach was employed to formulate clinical questions (Table 1), and inclusion and exclusion criteria were established.
| Criteria | Explanation |
|---|---|
| Population | Adults with primary progressive aphasia, regardless of their age, gender, and race |
| Intervention | All language interventions and tDCS to improve naming |
| Comparisons | No comparison |
| Outcomes | Improvement of naming ability in patients with primary progressive aphasia |
The JBR guidelines were adhered to throughout the review process. The authors conducted the search individually. All titles and abstracts were reviewed, and relevant original research articles were thoroughly examined. Studies were selected based on the following criteria: (a) original articles published in English; (b) conducted on patients with PPA; (c) involving the use of language intervention, tDCS, or a combination of both treatments; (d) aimed at improving naming abilities; (e) published between the start of 2010 and the end of 2022; (f) excluding animal studies, secondary data reports, such as meta-analyses, review articles, and study protocols. Following this phase, the authors convened a meeting to discuss the selected articles from each database. Cases of disagreement were reviewed, and an article was excluded or included based on the consensus of at least two researchers.
Full texts of the selected articles were then thoroughly reviewed. If the full text of an article was unavailable, three attempts were made to contact the authors via email. In the absence of a response, those articles were excluded from the systematic review.
3.3. Data Collection and Analysis
Data from each included study were extracted using a template for critical appraisal (26). The collected information covered publication details (author, title, year of publication, and source), type of study, study population, inclusion and exclusion criteria, sample size, study objectives, interventions and their implementation methods, control interventions, main outcomes, follow-up periods, and retention of study results.
Language treatment methods were categorized into four groups according to Pagnoni et al.: Lexical retrieval treatment, phonological and orthographic treatments, semantic treatment, and the multimodality stimulation approach. Identified treatment techniques for lexical retrieval include cueing hierarchies, lexical retrieval in context, RRIPP, the errorless learning approach, LLR treatment, and lexical retrieval cascade treatment (9).
3.4. Risk of Bias and Quality Assessment
Efforts were made to mitigate various biases throughout the review process. The risk of bias, including selection and detection bias, was evaluated by two reviewers, with any disagreements resolved through consensus.
All articles were systematically reviewed using JBI checklists for case-control studies, case series reports, quasi-experimental studies, and randomized controlled trials (27). Single-subject design studies were assessed using the SCED Scale checklist (28). Articles scoring higher than 50% on the respective checklists were selected for inclusion. After this phase, a qualitative synthesis of the information was conducted. The tests of the selected articles were reviewed and categorized based on the variant of progressive aphasia. The articles were analyzed according to the objectives of the study.
4. Results
4.1. Study Selection
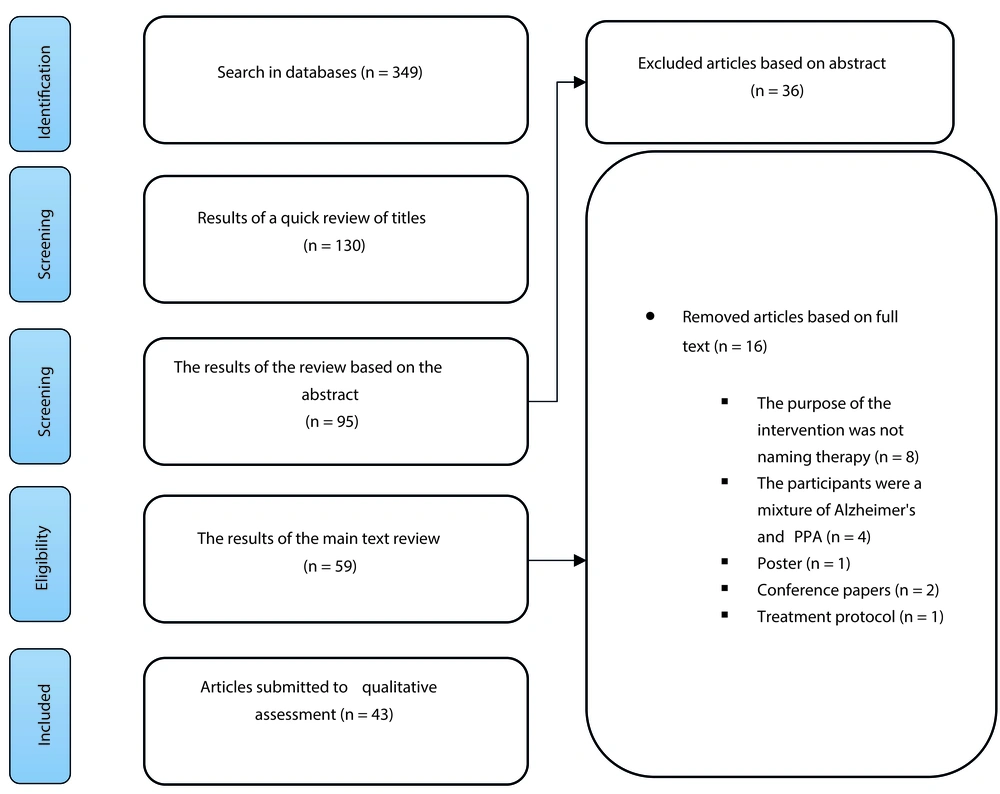
In the initial search, 349 articles were found. After removing duplicates, 130 articles were screened for titles leaving 95 articles based on their titles. After the detailed review of abstracts and inclusion and exclusion criteria, 59 articles remained. Out of these, 43 articles were selected for data extraction. Figure 1 illustrates the flowchart of the selection process. In the end, a total of 43 articles were chosen. Among these, 27 studies examined language treatment methods, 3 explored treatments with tDCS, and 13 investigated the concurrent use of language interventions and tDCS. The methods are detailed in Tables 2 - 4.
| Study | Number of Patients | Mean Age, year | Protocol Design | Language Intervention and Duration | Follow-Up | Outcome Measure | Result |
|---|---|---|---|---|---|---|---|
| Dressel et al. 2010 (29) | 1 man with svPPA | 48 | Single case study | Phonological and semantic cueing hierarchies (4 weeks) | 2 months | Oral naming abilities | Both types of treatments were useful. The result of therapy decreased over time. Changing in cortical activity, mainly in the right temporal cortex, were found |
| Jokel et al. 2010 (30) | 1 man with svPPA | - | Single-subject multiple-baseline across behaviors design | Errorless learning (12 sessions,60 minutes,4 weeks) | 1 to 3 months later | Verbal expression, auditory comprehension, reading, writing, semantic knowledge, cognitive screening | Errorless learning treatment in semantic dementia is effective in relearning lost words, and improved naming ability was maintained at all-time intervals. The patient retained the ability to name all the practiced words but could only name half of the unpracticed words. This study highlighted the feasibility of computer-based treatments for anomia in progressive disorders. |
| Farrajota et al. 2012 (15) | 10 intervention group (svPPA, vPPA, svPPA), f/m = 4/6 10 control group, f/m = 2/8 | Intervention group = 68.0 ± 7.8; control group = 66.2 ± 7.7 | Quasi experimental design | Multimodality approach treatment (1 h/week for 11 months) | Variability of follow-up times in the intervention and control groups | Change in the Snodgrass and Vanderwart | Naming was improved in the intervention group compared to the control group. The results showed that Language-based intervention in people with early progressive aphasia may slow the progression of some language deficits. |
| Jokel and Anderson 2012 (31) | 7 with svPPA f/m = 3/4 | 56 - 87 | Case series | The effectiveness of errorless versus errorful learning and active versus passive learning (12 sessions, 60 minutes, 4 weeks) | 1 - 3 month | Oral naming in trained and untrained nouns | Naming deficits in semantic dementia can be improved through therapy. Errorless learning is introduced as the best therapeutic method to do this. The errorless learning treatment was significantly more effective than the errorful learning treatment. The effect of active learning and its interaction with errorless learning was not significant. The generalization of treatment effects in semantic and naming fluency was somewhat evident. |
| Henry et al. 2013 (32) | 2 men; 1 with svPPA; 1 with lvPPA | svPPA = 60; lvPPA = 54 | Single subject | Lexical retrieval cascade + homework svPPA:8 sessions (60 min, 4 weeks) plus 20 sessions of homework (30 min, 4 weeks) homework: 12 sessions (120 min, 2.5 weeks) plus 12 sessions of homework (60 min, 2.5 weeks) hvPPA:6 sessions (60 min, 8 weeks) plus 18 sessions of homework (60 min, 6 weeks) | 3 - 6 months | Naming trained and untrained | This treatment method is efficacious in improving the naming skills of both participants. Maintained achievements, a generalization to untrained vocabulary items, improved word retrieval during the conversation, and greater confidence in communication were seen. |
| Savage et al. 2013 (33) | 4 men with svPPA | 62.3 (5.5) | A single-subject experimental design, using a 'multiple-baseline-across-behaviors | LLR only or LLR + sentence generation;30 - 60 min/day over 6 weeks | 1 - 2 months | Oral naming of trained and untrained nouns | Both treatments had evidence of effectiveness. All four participants showed significant improvements in their ability to name the trained items, with no change in the untrained items over the same period. Improvements were evident within three weeks after training. A substantial treatment effect size was found in patients with severe impairment. Retention of learning was observed at some follow-up assessments, although continued practice is likely required to maintain naming performance. |
| Savage et al. 2014 (34) | 5 men with svPPA; f/m = 1/4 | 61.8 (5.6) | Case series pre-post design | Semantic treatment 40 sessions (30 min, 8 weeks) | - | Oral naming trained and untrained; video description task. | All participants showed significant improvements in naming the trained pictures after the intervention. No significant improvement was observed in the control list (untrained) during the same period. The learning rate in mild patients was 90% or more, and in severe patients, between 48 and 84%. Improvements were also observed for the trained items in reading comprehension tasks. |
| Andrade-Calderón et al. 2015 (5) | 1 man with nfvPPA | 84 | Case report | phonological and orthographic treatments; 1 session in a week/12 months | - | Language development, fluency, and content of spontaneous speech, repetition, reading aloud, and oral-phonics performance. Aspects of cognitive, social and emotional functioning | Long-term speech therapy can improve language processing and have a positive effect on other cognitive and social-emotional processes in progressive aphasia. |
| Hoffman et al. 2015 (35) | 3 women with svPPA | 64.3 (0.5) | Single subject | Relearning training through semantics/writing and repetition. 15 sessions (20 min, 3 weeks) | 1 week,1 month,4-7 months | Oral naming of trained and untrained nouns; word-picture matching | Increasing the variability of the learning experience resulted in more durable word learning. The intervention did not improve the naming of untreated items. |
| Savage et al. 2015 (36) | 6 svPPA; f/m = 3/6 | 62.6 (5.8) | A single-subject experimental design (multiple-baseline across behaviors) | pairing of a photograph of each object with a visual and audio presentation of the word on the computer; LLR; 4 weeks | 2 month; 6 months | Oral naming of trained and untrained nouns | Improvements in naming can be sustained in svPPA with the support of less intense but ongoing revision. Results demonstrate that revision, through less intense forms of training, can help SD patients sustain words over a 6-month period. |
| Croot et al. 2015 (37) | 2 PPA f/m = 1/1 | 67 (18.37) | a single-blind, single-case experimental design (single subject) | RRIPP (repetition and/or reading in the presence of a picture) 2 weeks, 5 sessions per week | 1 month; (80-year-old male); 9 months; (54-year-old female) | Generalization to oral naming of trained and untrained nouns | RRIPP in the Presence of a picture improves naming in treated cases. Generalization of untreated items and retrieval of similar words was not seen in a structured interview. |
| Milano et al. 2015 (38) | 1 woman with svPPA | 70 | Case report | a semantic category cue | - | - | Using a semantic cueing strategy may help patients with svPPA. |
| Suárez-González et al. 2015 (39) | 1 woman with svPPA | 75 | A single-case, quasi-experimental design | Naming therapy vs. conceptual enrichment therapy: Each therapy ran for 3 months, with a 3-month time gap. | - | Oral naming of trained and nouns untrained; generalization measures: oral naming a visually; dissimilar example task; - description-to-naming task; - naming-to-description task | Both treatments caused an improvement in the naming of trained nouns but no improvement in untrained nouns. Generalization after conceptual enrichment therapy was more significant than naming therapy |
| Beales et al. 2016 (4) | 3 with svPPA; 1 l with vPPA; f/m = 1/3 | Men: 61 (7.0); Woman: 58 | case-series A multiple baseline across-behaviors design | The intervention integrated semantic, phonological, and orthographic levels of language production and drew on autobiographical memory. Eight 90-minute twice-weekly therapy sessions in 4 weeks | 4 weeks for one svPPA 5 weeks | Oral naming treated items oral naming untreated words generalization measures: Discourse Self-assessment of change | All participants showed significant improvements in naming treated items across all word classes. Different patterns of generalized improvement to untreated words were found for each participant. In discourse, the semantic variant participants demonstrated a significant increase in correct information units, unlike one participant with the logopenic variant, who remained stable. |
| Jokel et al. 2016 (40) | 4 with svPPA; f/m = 2/2 | 61.3 (7.8) | Quasi-experimental (pre-post design) | Semantic and phonological training based on errorless learning 20 weeks (10 weeks for each therapy); each session lasted approximately one hour 2 times a week. | - | Oral naming of trained and untrained nouns; generalization measures: - oral sentence production test; - semantic knowledge task - semantic and phonemic fluency | Improvement in trained nouns was seen in two approaches, but semantic treatment was better. Improvement in untrained nouns and generalization was seen in two or three of the patients. Only the patient indicated better function in semantic fluency |
| Hameister et al. 2016 (41) | 2 with nfvPPA; f/m = 1/1 | Single subject | CIAT-based group therapy + computerbased home training; nine 60-minute sessions in two consecutive weeks | 2 months | Oral naming of trained and untrained verbs and nouns; grammatical structure of trained and untrained items; untrained connected speech | Both participants achieved significant improvements in their noun and verb naming accuracy and their grammatical structure for trained items. Generalization to different pictures of the same item was found for both participants, and one participant also showed improved grammatical structure when describing untrained pictures. No significant generalization to untrained connected speech samples was observed for either participant. | |
| Kim 2017 (42) | 2 with lvPPA; In first phase: 1 man with lvPPA; In second phase: 2 man | 68 (7.7) | single subject case design | Lexical Retrieval Cascade Treatment: two 50-minute sessions each week (8 sessions) plus daily homework | 5 months (20 weeks) | Oral naming of trained and untrained nouns; generalization measure: - Discourse measures | Both participants improved in trained nouns but did not improve in untrained nouns. Small effect in discourse |
| Jafari et al. 2018 (43) | 1 woman with nfPPA | 56 | Single-case experimental ABAB design | Semantic and phonological cueing at the single word level and the integration of these methods in narrative discourse context. 8 sessions (60 min, 4 weeks) | 2 weeks | Oral naming of trained and untrained nouns and verbs | Both treatment programs lead to improvement in word retrieval ability. Generalization of untreated cases and maintenance of treated cases also occurred. The use of words in the story's context has a more facilitating role than the treatment of single words in processing and retrieving words. |
| Suarez-Gonzalez et al. 2018 (44) | 1 woman with svPPA | 62 | Single case experimental design; (AB1 AC AB2) (single subject) | Conceptual enrichment (COEN) training vs. Classical naming training; 1 hour for 7 days (first 5 consecutive, a gap of 2 days of no therapy and 2 more days) | 3 and 6 weeks | Oral naming of trained nouns | Both treatments were effective. However, words trained using the Conceptual enrichment training showed a significantly higher degree of generalization than those trained under the naming treatment. Furthermore, only words taught with the conceptual enrichment training showed significant improvement compared to baseline performance when assessed 6 weeks after training. |
| Croot et al. 2019 (45) | 3 with nf/avPPA; 2 with svPPA; 2 with l/phvPPA; 1 with mixed PPA; f/m = 5/3 | nf/avPPA: 66.7 (6.8); svPPA: 64; (5.0); l/phvPPA: 61.5 (2.5); Mixed PPA: 68 | Series of single case experimental design studies (SCEDs) (case series) | RRIPP (repetition and/or reading in the presence of the picture), 10 - 20 sessions in the first and second treatment periods (2 - 4 weeks) and 104 sessions in the third treatment period (26 weeks) | 9 to 84 weeks | Oral naming of trained and untrained nouns | Improvement in the naming of the trained items was observed for those who completed the treatment period. However, generalization to untrained items was not observed. During follow-up, the trained items were retained. |
| Henry et al. 2019 (12) | 9 with svPPA; 9 with l/phvPPA; f/m = 11/7 | svPPA: 67.3; (8.7); l/phvPPA: 63.2 (7.8) | Case series | LRT (lexical retrieval treatment) + CART (copy and recall treatment) at home; 4-8 sessions (60 min, 4 - 8 weeks) plus daily homework (15 min) or LRT2 plus homework (CART) Duration: 8 - 16 sessions (60 min, 4 - 8 weeks) plus daily homework (15 min) followed by Booster phase: 8 sessions (30 min, 4 weeks | 3, 6, and 12 months | Oral naming of trained and untrained nouns and WAB AQ in generalization | Improvement in trained and untrained itemes, no changes in WAB AQ; maintained was seen on 3, 6 months |
| Meyer et al. 2019 (46) | 12 with lvPPA, 5 with svPPA, 9nfvPPA; 1 with mixed PPA (was excluded from the data analyses); f/m = 15/12 | lvPPA = 68.1 (9.9); svPPA = 65.5 (5.3); nfPPA = 68.1 (10.5); mixed | Case series | A phonological treatment and an orthographic treatment plus homework 13 sessions (45 min, 4 weeks) + 55 sessions homework (10-15 min, 20 weeks) | 1, 8, and 15 months | Oral naming trained and untrained nouns (naming accuracy); written trained and untrained nouns; generalization measure: - scene description task | Improvement in oral and written naming in trained and untrained items after both treatments; Improvement in - scene description task especially after orthographic treatment; treatment can persist for as long as 15 months post-treatment; long-term treatment effects were more robust in the orthographic treatment condition and for participants with svPPA. |
| Krajenbrink et al. 2020 (47) | 1 man with svPPA | 60 | Case report | RRIPP (repetition and/or reading in the presence of the picture) vs. conceptual enrichment (COEN) training | - | Oral naming trained and untrained nouns; Written trained and untrained nouns; generalization measures: Structured interview; picture-word verification task | Improvement in oral and written naming in trained and untrained items after both treatments; generalization: improvement in picture-word verification task only after RRIPP |
| Lavoie et al. 2020 (13) | 2 with svPPA; 3 with l/phvPPA | svPPA: 70.5; (4.5) lvPPA: 73.3 (4.8) | Single case series | Self-administered using a smart tablet; 16 sessions (4 weeks | 2 weeks, 1 and 2 months | Oral naming of trained and untrained nouns; generalization measure: - Ecological conversation task | Improvement in oral naming in trained and untrained items; ecological conversation task for three patients; maintenance for trained items for 2 svPPA and 2 LvPPA |
| Machado et al. 2021 (48) | 3 with nfvPPA; 5 with svPPA 5 with lvPPA; 5mixPPA; f/m = 9/9 | 66.3 | multiple single-case study (single subject) | cognitive intervention program directed toward a specific language-speech impairment; 24 sessions of 50 minutes over four months (twice a week) | 1 - 8 months | naming deficits, sentence production, speech apraxia, and phonological deficits | All subjects performed better on the trained items at the post-test for each rehabilitation program p, indicating that learning the taught strategies was achieved during the active phase of treatment. Statistical significance was obtained for 13 people. While for five people, the results were maintained. Generalization of untrained items was seen in naming and sentence production. Speech and language therapy strategies are helpful for the clinical management of individuals with primary progressive aphasia. |
| Montagut et al. 2021 (16) | 8 with svPPA; f/m = 4/4 | 64 (11.25) | Single subject design | Errorless Learning Therapy: 16 sessions (45 minutes each, twice a week) | 1, 3, and 6 months | Oral naming of trained and untrained items | In naming tasks, patients showed significant improvement in trained items immediately after the intervention, but this improvement gradually decreased as the treatment ended. No improvement was observed in the trained comprehension or in the untrained tasks. |
| Paek et al. 2021 (49) | 1 woman with nfvPPA; 1 man with svPPA | 68 (4.24) | Case-series design | semantic feature analysis, semantic comprehension training, phonological component analysis, definitions, memory game training, charades; 16 sessions (60 minutes, twice a week) | 3 months | Overall, both participants showed improvement in naming specially trained items. The participant with milder cognitive-linguistic showed greater outcomes |
Abbreviation: f/m, female/male.
| Study | Number of Patients | Mean Age, year | Protocol Design | Intervention/Comparators | Follow-Up | Outcome Measure | Result |
|---|---|---|---|---|---|---|---|
| Wang et al. 2013 (50) | 1 woman with nvPPA | 67 | Single subject | Sham tDCS and anodal tDCS anodal (or sham) tDCS over the left posterior perisylvian region in the morning and left Broca's area in the afternoon, two sessions every day, 5 days | phone follow-up2 months | auditory word-picture identifications, picture naming, oral word reading, and word repetition | Anodal tDCS over the left Broca’s area and left PPR could improve picture naming, auditory word comprehension, oral word reading, and word repetition in nfvPPA after 5 days of treatment; language function began to decline 2 months after the treatment |
| McConathey et al. 2017 (22) | 1 with lvPPA, 6 with nvPPA; f/m = 5/2 | 68.71 ± 6.97 | RCT (randomized, sham-controlled design) | anode on the left prefrontal region, the cathode over the left occipital region, and sham tDCS | 6 and 12 weeks | semantic processing (picture naming), speech repetition, grammatical comprehension | Improvement in global language function with anodal tDCS; severity of deficits at baseline may be an important factor in predicting which patients |
| Gervits et al. 2016 (51) | 4 with lvPPA; 2 with nvPPA; f/m = 5/1 | 66.2 ± 5.7 | Unblinded pilot study | Anode over the left frontotemporal region (F7) cathode over the left occipito-parietal region for two weeks (10 days). 20-min stimulation session | Week stimulation period, and then 6 weeks and 12 weeks | Boston Naming Test (BNT), Pyramids and Palm Trees, test for the reception of grammar category naming latency; sentence repetition; elicited speech production | tDCS paired with a speech elicitation task induced persistent improvement in language skills in patients improvements on a variety of linguistic measures that were sustained for at least 3 months following tDCS |
Abbreviation: f/m, female/male.
| Study | Number of Patients | Mean Age, year | Protocol Design | Intervention/Comparators | Follow-Up | Outcome Measure | Result |
|---|---|---|---|---|---|---|---|
| Cotelli et al. 2014 (52) | 16 with nvPPA; AtDCS = 8; PtDCS = 8; f/m = 11/16 | 66.9 ± 8.2 | Clinical trial (parallel study) | tDCS was applied over the left DLPFC (BA 8/9) 25 minutes per day for two weeks (10 days). Each patient underwent 25 minutes of individualized speech therapy with either AtDCS or PtDCS during each treatment session. | 12 weeks | naming accuracy, treated and untreated items | Significant improvement in experimental naming was observed in both groups at treatment 1 and treatment 2, but this effect was significantly greater in AtDCS than in PtDCS patients. The analysis of daily living language abilities improved selectively in the AtDCS group. |
| Cotelli et al. 2016 (53) | 18 with nvPPA; f/m = 9/9 | 66.5 ± 9.5 | Clinical trial (parallel study | tDCS stimulation over the left DLPFC+ combination with ICAT; 2 weeks of five daily sessions of 25 min during 25 min of ICAT | 3 months | Naming accuracy- treated and -untreated items related to regional grey matter (GM) density | Naming accuracy was improved |
| Tsapkini et al. 2018 (54) | 14 with nfvPPA; 12 with lvPPA; 10 with svPPA | Double-blind, within-subject crossover | tDCS over the left IFG, sham stimulation paired + written language interventions; 15 consecutive therapy sessions for each stimulation condition, five sessions per week | 2 weeks; 2 months | Letter fluency, semantic fluency, object naming, action naming, digit span forward, digit span backward, JHU sentence anagrams, object semantics, action semantic, sentence repetition, syntactic comprehension, verbal learning, spelling words, spelling nonwords, | Using tDCS as an adjunct to written language interventions in individuals with logopedic or nonfluent/agrammatic PPA seeking compensatory treatments in clinical settings. | |
| Fenner et al. 2019 (19) | 6 with nfvPPA; 5 with lvPPA; f/m = 4/7 | 69.18± 6.2 | Within-subjects crossover design | Anodal tDCS over the left IFG, sham stimulation, verb therapy, 10 - 14 consecutive therapy sessions in each treatment period, 5 sessions per week lasting 40 - 60 min each. | 2 weeks and 2 months | improves trained and untrained written verb naming and spelling performance | tDCS over the left IFG improves written verb naming significantly more than sham in lvPPA and nfvPPA; the gain was significant at 2 weeks and 2 months post-treatment generalization of therapy gains to untrained verbs |
| Ficek et al. 2018 (55) | 8 with nfvPPA; 8 with lvPPA; 8 with svPPA; f/m = 11/13 | 67.2 ± 6.5 | double-blinded, within-subject crossover design | tDCS over the left inferior frontal gyrus (IFG), sham, speech-language therapy; 5 sessions of daily therapy, in which patients received either tDCS or sham simultaneous with the start of language therapy | - | Oral and written naming measures for trained and untrained items; task-based fMRI | tDCS modulates GABAergic inhibition to augment learning and is clinically useful for PPA combined with language therapy. the changes in FMRI were noticeable |
| Roncero et al. 2019 (56) | 4 with svPPA, 4 with lvPPA; 4 with nfvPPA; f/m = 4/8 | 65.41 ± 6.31 | RCT double-blind cross-over design | tDCS stimulation to either the left inferior parietotemporal region (P3), the left dorsolateral prefrontal cortex (F3), or sham stimulation; 10 sessions with 30 min of anodal 10 sessions; Language training (daily training sessions in each round of stimulation) | 2 weeks, 2 months | Naming performance (train and untrained items) | tDCS produced an improvement in picture naming for a mixed group of PPA participants that was superior to training and sham for both trained and untrained items. At the end of the stimulation sessions, real tDCS produced larger improvements than sham for both trained and untrained items, regardless of the montage. More specifically, although both the DLPC and parietal-temporal montages led to greater improvement for trained items when participants were evaluated at the final stimulation session, only the parietal-temporal montage maintained this advantage over sham stimulation when participants were evaluated 2 weeks after their final stimulation session. The parietal temporal montage was also the only montage where a significant improvement was found for untrained items 2 weeks post-stimulation. |
| Harris et al. 2019 (57) | 10 with nfvPPA; 6 with lvPPA; 6 with svPPA; f/m = 11/11 | 66.9 ± 7.5 | Double-blind study | Anodal tDCS, sham + langage therapy; 20 min tDCS and Language therapy started at the beginning of stimulation and continued for a regular speech-language therapy session of 45 - 50 minutes, i.e., 25 - 30 minutes after the end of stimulation for both conditions. | 2 months | Language score changes; metabolite changes | tDCS modulates GABAergic inhibition to augment learning and is clinically useful for PPA combined with language therapy. Patients who received anal tDCS showed improvement compared to the sham group. In the tDCS group, in the 2-month follow-up, the language scores were significantly higher than the sham group. |
| de Aguiar et al. 2020 (58) | 15 with nfvPPA; 17 with lvPPA; 8 with svPPA; f/m = 15/15 | 67.68 ± 6.76 | Between-subject randomized design | tDCS, sham + language therapy; 12 (± 2) sessions two-month interval in between therapy phase | 2 weeks, 2 months | written naming/spelling' and 'spelling-only' therapy | For trained words, patients who improve the most are those who retain longer language skills such as sublexical spelling processes (phoneme-to-grapheme correspondences) and word retrieval, and other cognitive functions such as executive functions and working memory, and those who have better learning capacity. Generalization of untrained words occurs through improvement in knowledge of phoneme-to-grapheme correspondences. Furthermore, tDCS enhances the generalizability and duration of therapy effects. |
| de Aguiar et al. 2021 (59) | 1 man with lvPPA | 72 | a single-case study; two separate treatment phases | Letter Fluency Therapy (LeFT) paired with tDCS, 10 1-h sessions | 3 months, 2 months | ords retrieved trained and untrained items | Letter fluency therapy combined with anodal tDCS is effective in improving lexical retrieval, particularly when left IFG stimulation is used. Effects generalize beyond the trained task, albeit slowing down responses in picture naming |
| Tao et al. 2021 (6) | 10 with nfvPPA; 14 with lvPPA; 8 with svPPA; f/m = 16/16 | 67 ± 6.73 | Double-blind, randomized, sham-controlled design | tDCS and sham interventions + language therapy (written word production) 15 sessions of daily therapy | 2 months; 2 weeks | the trained and untrained words; within-module and between-module; connectivity of the LIFG | TDCS-augmented language therapy in PPA increased the functional segregation of the language system, a normalization of the hyperconnectivity observed before treatment. tDCS group showed a significant decrease in global connectivity, whereas the Sham groups did not change, suggesting specific neural effects induced by tDCS. |
| Zhao et al. 2021 (21) | 18 with nfvPPA; 14 with lvPPA; 7 with svPPA; f/m = 20/19 | 7.69 ± 7.69 | Randomized, sham-controlled, double-blind, crossover design | anode over the left frontal lobe, centered on F7, sham, language therapy; 15 consecutive weekday sessions | 2 months; 2 weeks | - | Both sham and tDCS groups significantly improved in trained items immediately after and at 2 months post-therapy. Improvement in the tDCS group was greater and generalized to untrained words. White matter integrity of ventral language pathways predicted tDCS effects in trained items, whereas white matter integrity of dorsal language pathways predicted tDCS effects in untrained items. Conclusions. White matter integrity influences both language therapy and tDCS effects. Thus, it holds promise as a biomarker for deciding which patients will benefit from language therapy and tDCS. |
| Sheppard et al. 2022 (60) | 3 women with 2 nfvPPA; 1 with lvPPA | 73 ± 9 | A randomized, double-blind, sham-controlled, within-subject crossover design | Anodal tDCS, sham, VNeST; 15 VNeST training sessions + tDCS and 15 VNeST sessions + sham intervention period. Each session 1 hr, received 3 - 5 sessions per week | 1 week; 8 weeks | the accuracy of naming, trained and untrained verbs. Secondary outcome variables also included total accuracy in producing sentences on the sentence priming production test and comprehending sentences on the sentence comprehension. | Different patterns of outcomes were shown for each of the participants. Two participants with nonfluent variant PPA had a tDCS advantage for generalization to the naming of untrained verbs, which was apparent at 1 week and 8 weeks post-treatment. One participant with a confluent variant also showed evidence of generalization to sentence production in the tDCS phase. |
| Wang et al. 2022 (61) | 14 with lvPPA, 13 with nfvPPA, 9 with svPPA; f/m = 17/19 | - | Within-subjects, double-blind, crossover design with two experimental conditions | Anodal tDCS, sham, language therapy; 12 consecutive weekday sessions; the two phases were separated by a two-month wash-out period. | 2 weeks; 2 months | Semantic fluency; spelling accuracy | Semantic fluency improved significantly more in the active tDCS than in the sham tDCS condition immediately after and two weeks after treatment. This improvement was marginally significant two months after treatment |
Abbreviation: f/m, female/male.
4.2. Population
After diagnosing PPA, the time taken to initiate the treatment varied between 6.5 months and 10.5 years. The duration of the studies varied from 6.5 to 10.5 years. However, in most studies, treatment commenced two years after the onset of symptoms. The age range of participants was also broad, spanning from 48 to 87 years old.
4.3. Intervention
4.3.1. Language Intervention
As presented in Table 2, lexical retrieval treatment, encompassing 17 studies, was the most frequently investigated intervention for PPA. Among these, six studies focused on the cuing hierarchy approach (4, 12, 29, 35, 41, 43), four examined the errorless learning approach or its comparison with the error-prone approach (16, 30, 31, 40), two explored the Look, Listen, Repeat (LLR) treatment (33, 36), two investigated Repetition and Reading In the Presence of a Picture (RRIPP) (37, 45), two applied the lexical retrieval cascade treatment (32, 42), two studies utilized phonological and orthographic treatments (5, 46), one adopted the multimodality stimulation approach (15), and eight implemented semantic treatments (13, 34, 38, 39, 44, 47-49). Table 5 displays studies of language interventions across different variants of PPA.
| Types of Primary Progressive Aphasia | Number of Articles |
|---|---|
| svPPA | 13 |
| nfPPA | 2 |
| lvPPA | 1 |
| svPPA / lvPPA | 4 |
| nfPPA / lvPPA | 1 |
| svPPA / lvPPA / nfvPPA | 2 |
| nfvPPA / lvPPA/svPPA / mix PPA | 2 |
| svPPA / nfvPPA | 1 |
The duration of the treatment period ranged from 2 weeks to 12 months. In most cases, treatment occurred twice a week, with each session lasting between 20 and 60 minutes. Regardless of the type of language intervention, evidence from all studies indicated positive effects and improvements in naming. Most studies conducted follow-up assessments 1 to 6 months post-treatment, but three studies extended follow-up to one year or more. Some studies assessed the generalization of treatment gains.
4.3.2. tDCS
Studies on instrumental treatments, as listed in Table 3, included the use of tDCS (22, 50, 51). In all such studies, an anode stimulation electrode was positioned on the left hemisphere of the brain, targeting areas like the temporal and parietal temporal regions involved in word finding. Every study employing tDCS reported improvements in naming among patients with various variants of PPA. In Wang's study, a decline in language function was observed post-treatment, whereas Gervits' study indicated that treatment effects persisted for at least three months following tDCS.
4.3.3. Language Interventions and tDCS
Thirteen studies explored the combination of language treatment methods with tDCS as curative approaches (6, 19, 21, 52-54, 56-59) (Table 4). In these treatments, tDCS was applied anodally at various brain regions involved in word finding. Language treatment methods varied, including the use of orthographic and phonological cues, with semantic cues being less commonly employed. Retrieval cascade techniques were also utilized. Despite the variability in language treatment methods used alongside tDCS across these studies, results indicated that the combined application of these two treatments improved patients' performance. The duration of treatment typically spanned two weeks, with one or two sessions conducted daily. Therapy sessions ranged from one to two per day, lasting between 25 minutes and one hour. Follow-ups were conducted 2 weeks to 3 months post-treatment.
4.4. Study Design
4.4.1. The Level of Evidence
4.4.1.1. Language Intervention
As detailed in Table 2; 27 studies evaluated language treatment. Only two studies were quasi-experimental, based on the level of evidence (15, 31). Farrajota et al. investigated the effectiveness of the multimodality stimulation approach on 20 participants with varying follow-up periods in intervention and control groups (15). Another quasi-experimental study by Jokel and Anderson focused on lexical retrieval treatment using errorless learning principles without a follow-up period (31).
4.4.1.2. tDCS
According to Table 3, two randomized controlled trials investigated the effects of tDCS: one study with 7 participants and follow-up periods ranging from 6 to 12 weeks (22) and another with 6 participants and a four-month follow-up period (51).
4.4.1.3. Language Interventions and tDCS
From the perspective of the level of evidence, as shown in Table 4; 8 clinical trial studies (6, 19, 21, 54, 55, 58, 59, 61) and two quasi-experimental studies (53, 62) were identified for language interventions and tDCS.
5. Discussion
The current study demonstrates that language treatment methods, tDCS treatments, and the concurrent application of language treatment with tDCS can be effective in managing PPA, a neurodegenerative disorder. tDCS, as a tool for naming therapy, offers a promising new approach. All these interventions in PPA have shown improvements in naming function. However, not all have demonstrated adequate generalizability and maintenance of treatment effects. The ability of treatments to generalize to untreated items and the longevity of treatment effects warrant further exploration. Longitudinal studies are needed to assess whether these interventions can alter the disease's progression rate or even slow symptom progression. The duration of treatment is a critical factor that may affect the sustainability of treatment benefits.
In language treatments, lexical retrieval interventions have proven effective for addressing naming difficulties in individuals with various PPA variants. Nonetheless, some treatments have a low level of evidence, and only a few studies have examined their generalization effects and sustainability. Lexical retrieval treatments employ a set of cues that activate semantic and phonological knowledge, aiding in lexical retrieval. The purpose of these cues is to make optimal use of semantic, phonological, and orthographical knowledge to facilitate word retrieval. Improvements in naming can enhance both content and effective communication, thereby improving the quality of life (9).
Among lexical retrieval treatments, errorless learning has garnered considerable evidence for its effectiveness. Errorless learning prioritizes exposure to correct information, positing that creating errors may strengthen incorrect stimulus-response associations and reduce treatment efficiency, especially in patients with memory issues. This approach has been utilized for naming treatments, aiming to prevent the elicitation of incorrect responses through the patient's repeated attempts (63). Patients are exposed to educational cues that increase the likelihood of a correct response. This treatment has been particularly used for the svPPA variant. In a study comparing errorless and errorful treatments, errorless learning proved significantly more effective than errorful learning. While some studies have incorporated phonological and semantic cues, semantic cues appear more effective (40). This treatment method is well-suited for patients with svPPA who exhibit semantic memory deficits.
Semantic treatment has primarily been applied to patients with svPPA, with only a few studies assessing its impact on other PPA variants. Semantic treatment has also been used to address naming deficiencies in other types of dementia, especially when naming failures are associated with semantic deficits.
Regarding the level of evidence for language treatments, the study by Farrajota et al. in 2012 stands out as a quasi-experimental study involving 20 participants and a follow-up period of nearly 22 months, showcasing substantial evidence. The findings from this study suggested that individual multimodality treatment was effective in treating naming difficulties in individuals with progressive aphasia (15). Another quasi-experimental study by Jokel et al. (40) involved four people with semantic dementia and four healthy individuals. This study applied semantic and phonological treatment approaches following errorless learning principles and assessed their naming performance. The results indicated that this approach ameliorates naming deficiencies in individuals with svPPA, irrespective of the severity of their semantic impairment.
Based on the studies mentioned, there is no one-size-fits-all treatment for the various variants of PPA. For instance, phonological-orthographic treatment has been applied to individuals with svPPA. Thus, the specific variant of PPA becomes less critical, with the focus shifting to the type of treatment and its level of evidence. Of these, treatments based on errorless learning present stronger evidence compared to lexical retrieval and multimodality treatments, although research in these areas is also somewhat limited.
Instrumental treatment methods have been less frequently explored, yet there is solid evidence supporting their effectiveness. While such treatments have not been formally incorporated into the treatment protocol for progressive aphasia, three controlled clinical trials have examined the impact of tDCS on the language abilities of individuals with PPA. The findings from all studies suggest that tDCS can effectively address naming deficiencies in PPA, even in the absence of language interventions.
In 13 studies, tDCS was utilized alongside language treatments, with results suggesting that this combination is effective. This method boasts a strong level of evidence; notably, eight of these articles were controlled randomized trials. Such robust evidence could support the use of tDCS as a standardized and accepted method for treating PPA. However, it has yet to be incorporated into treatment plans for individuals with PPA, as it has not yet received endorsement as a standard treatment by international scientific associations. Two major global organizations, the US Food and Drug Administration and the European Medicines Agency, are responsible for approving treatment methods. Currently, both entities have not approved the use of tDCS for treating PPA, allowing its use only for research purposes.
The duration since disease onset varied across studies, typically beginning two years after symptom manifestation, a timeline often necessary for a definitive diagnosis of PPA. The participants' ages also varied, with no study specifically exploring the impact of age on treatment efficacy. Nonetheless, some studies indicated that the treatment was effective even in older age groups.
5.1. Conclusions
The three treatment approaches reviewed here all led to positive outcomes despite the diversity of interventions applied. However, these studies faced limitations such as design issues, small sample sizes, short follow-up periods, and a lack of assessment of the maintenance and generalization of treatment effects.