Dear Editor,
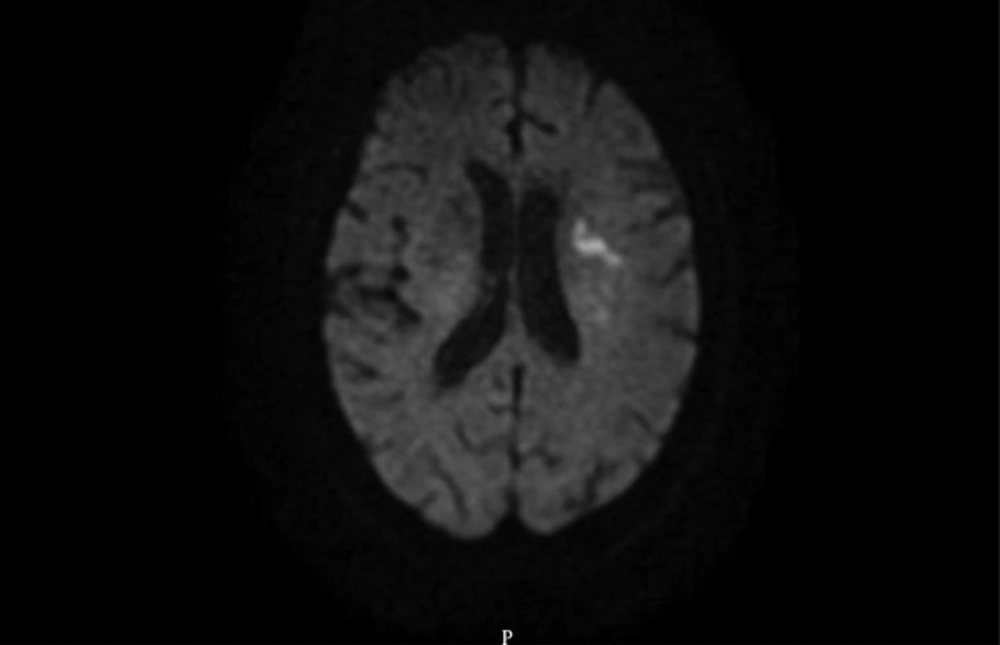
A 87- year-old lady with known history of paroxysmal atrial fibrillation (PAF) presented with sudden onset of expressive aphasia and right sided hemiparesis. She was not on any anticoagulant for her PAF at the time of presentation. She was eligible for intravenous thrombolysis (IVT) and received IVT within 3 hours of symptom onset with significant improvement in her neurological symptoms in the next 24 hours. Her Brain MRI post IVT showed an area of acute infarct in left corona radiata (Figure 1), her CT angiogram of head and neck did not show any hemodynamically significant stenosis. EKG on admission shows paroxysmal atrial fibrillation. Within 12 hours of hospital admission, she developed acute onset severe epigastric abdominal pain associated with nausea and vomiting. Serum amylase was 372 Unit/Liter (normal range: 20 - 96) and serum lipase was 364 Unit/Liter (normal range: 7 - 78). Abdominal computed tomography with contrast showed acute interstitial edematous pancreatitis involving the head of the pancreas. There was no evidence of gallstone or distended gallbladder. Her serum triglyceride level and calcium were within normal range. There is no history of alcohol use or autoimmune disease.
Our patient did not have any gallstones, history of alcohol use, hypertriglyceridemia, hypercalcemia, and history of trauma or concomitant autoimmune disease which are considered the common causes of acute pancreatitis (1). Atrial fibrillation (AF) is a well-established cause of cardio-embolic stroke and also peripheral embolism (2). Given the simultaneous occurrence of acute cardio-embolic ischemic stroke with acute pancreatitis in our patient, an ischemic cause for the acute pancreatitis can be assumed with a high degree of probability. Acute pancreatitis associated with PAF has been reported rarely (3) and our case is one of the first reports of acute pancreatitis possibly caused by thromboembolism associated with AF. Due to high prevalence of PAF in the elderly, it should be considered as one the potential causes of idiopathic pancreatitis particularly in the patients with evidence of simultaneous other thromboembolic events.