1. Background
Currently, one of the most significant problems in healthcare centers is hospital infections (1-3). Nosocomial infections are infections that either occur locally or spread throughout the hospital and are caused by pathogenic microorganisms or their toxins. Hospital infections are a major cause of disease outbreaks and patient deaths (4, 5). A hospital-acquired infection is one that a patient acquires after 48 hours of hospitalization or within 72 hours of discharge, which was not present at the time of admission and was not in a latent state (6-8). Nosocomial infections should not be present at the time of patient admission and should not be in the incubation period (4, 9).
Despite many advances in treatment methods, the risk of hospital infections has increased due to prolonged hospitalization and the increased use of invasive methods. These methods include the use of vascular catheters, ventilators, intubation, surgical drains, long-term catheterization, immunosuppression, failure to change dressings, and improper glove use (10). Nosocomial infections prolong hospital stays, delay recovery, and reduce the patient’s quality of life, leading to various complications (11).
Prolonged hospital stays increase mortality rates and, consequently, hospital costs. Additionally, they pose a risk for the spread of infections in the community, with rates varying by country. Hospital infections are associated with increased mortality, disability, prolonged hospitalization, and significant treatment costs (9). Factors such as patient age, type and severity of the disease, underlying conditions, diabetes mellitus, chronic lung disease, kidney failure, cancer, patient immunodeficiency, and overuse of antibiotics during hospitalization affect the prevalence of hospital infections (12).
A significant number of hospital infections are preventable, and medical personnel can play a crucial role in reducing their incidence. Observing hand hygiene and basic handwashing is essential in preventing infections. Since a significant proportion of infections originate in the operating room, staff in these areas can play a critical role in preventing such infections by adhering to proper hand hygiene (4).
One type of hospital infection that can occur due to non-compliance with hand hygiene during therapeutic procedures, such as catheterization or other invasive measures in the operating room, is urinary tract infection. Urinary tract infection is a common nosocomial infection and is considered one of the most frequent hospital-acquired infections (13).
Urinary tract infection is a prevalent infection that constitutes a significant portion of all hospital infections. The infectious agents responsible for UTIs are diverse, including fungal, viral, and bacterial pathogens (14-16). Various factors contribute to the development of UTIs, including trauma (17). In cases of trauma, urinary catheterization is often required, which can increase the risk of UTIs. Trauma can affect different parts of the body, with spinal cord injury being one such type of trauma (18). Spinal cord injury is prevalent and can result in both short-term and long-term complications (19-22). These complications can lead to infections, including UTIs, which can cause additional complications for SCI patients (23-25).
2. Objectives
Given the importance of spinal cord injury (SCI), this study aimed to investigate the prevalence, etiological factors, and risk factors associated with urinary tract infections in SCI patients.
3. Methods
3.1. Study Design and Study Population
This study was conducted at a government hospital, examining patients who were admitted for spinal cord injury due to trauma.
3.2. Inclusion and Exclusion Criteria
Patients over 18 years of age who were admitted to the hospital during the first six months of 2020 were examined. Patients with a urinary tract infection at the time of admission were excluded from the study. Only patients who developed a UTI during their hospitalization or within 48 hours after discharge were included.
3.3. Data Gathering
The data collection tool included a checklist with questions about age, sex, signs and symptoms of the disease, presence of other diseases, length of hospital stay (in days), etiology of UTI (traumatic and non-traumatic causes), marital status, history of urinary tract infections in the past three years, causes of trauma (e.g., traffic accidents, fights, falls, sports accidents), type of injury (e.g., cervical, thoracic, lumbosacral), urinary incontinence (yes or no), bladder irrigation (yes or no), associated symptoms (e.g., fever, hematuria), and the type of microorganism (e.g., E. coli) if the patient used invasive methods such as urinary or venous catheters. The patient's profile was meticulously recorded, and the types of antibiotics used were also carefully documented.
3.4. Method of Research
Patients were examined daily. If a UTI diagnosis was confirmed based on laboratory results and the attending physician's opinion, the patient was included in the study, and the researcher-completed checklist was filled out by the researchers. Ethical considerations included obtaining an ethics approval code from the university, maintaining confidentiality in research and reporting, and adhering to all ethical guidelines established by the university.
3.5. Data Analysis
Data were analyzed using SPSS version 16 software.
4. Results
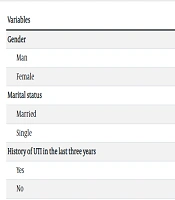
The results showed that 67.4% of the patients were male, 76.5% were married, 33.3% had a history of UTI, 44.7% had etiology related to traffic accidents, and 56.1% had urinary incontinence. The mean (SD) age of the patients was 44.77 (7.64) years, and the mean (SD) duration of illness was 14.87 (7.25) years (Table 1).
| Variables | Values |
|---|---|
| Gender | |
| Man | 89 (67.4) |
| Female | 43 (32.6) |
| Marital status | |
| Married | 101 (76.5) |
| Single | 31 (23.5) |
| History of UTI in the last three years | |
| Yes | 44 (33.3) |
| No | 88 (66.7) |
| Etiology | |
| Quarrel | 36 (27.3) |
| Traffic accidents | 59 (44.7) |
| Falling from a height | 34 (25.8) |
| Sports events | 3 (2.3) |
| Neurological level | |
| Lumbosacral | 48 (36.8) |
| Thoracic | 61 (46.2) |
| Cervical | 23 (17.4) |
| Urinary incontinence | |
| Yes | 58 (43.9) |
| No | 74 (56.1) |
| Bladder irrigation | |
| Yes | 79 (59.8) |
| No | 53 (40.2) |
| Age | 44.77 ± 7.64 |
| Duration of illness | 14.87 ± 7.25 |
Distribution of Demographic Characteristics of Patients with Spinal Cord Injury a
The results showed that 30.3% of patients had hematuria symptoms, 35.5% had fever symptoms, and 12.9% had scrotal pain or turbid urine (Table 2). Regarding microbial infections, 55.3% of patients had E. coli, 11.4% had Proteus, 9.1% had Klebsiella, and 7.6% had Candida spp (Table 3).
| Variables | No. (%) |
|---|---|
| Hematuria | 40 (30.3) |
| Suprapubic pain | 4 (3) |
| Scrotal pain | 17 (12.9) |
| Turbid urine | 17 (12.9) |
| Fever | 47 (35.6) |
| Scrotal pain | 7 (5.3) |
Accompanying Symptoms in Urinary Tract Infection Infections in Patients with Spinal Cord Injury
| Variables | Yes | No |
|---|---|---|
| E. coli | 73 | 55.3 |
| Acinetobacterspp. | 9 | 6.8 |
| S. aureus | 7 | 5.3 |
| Proteus spp. | 15 | 11.4 |
| Klebsiella spp. | 12 | 9.1 |
| Candida spp. | 10 | 7.6 |
| Enterobacter spp. | 4 | 3 |
| Pseudomonas | 2 | 1.5 |
| Total | 132 | 100 |
Frequency (%) of Types of Microorganisms Present in Urinary Tract Infection Infections of Patients with Spinal Cord Injury a
5. Discussion
This study aimed to determine the prevalence, etiological factors, and risk factors of UTIs in spinal cord injury patients. Patients with SCI are particularly susceptible to surgical and hospital-acquired infections due to frequent interactions with healthcare staff and the use of invasive diagnostic and treatment methods. Among these infections and complications, pneumonia, urinary infections, and pressure ulcers are notable (26-28).
The findings indicate that the prevalence of UTI was higher among patients with a urinary catheter compared to other patients, highlighting the high prevalence of catheter-associated urinary tract infections (CAUTI) in SCI patients. In Vinoth et al.'s study, the prevalence of CAUTI was 20%, with 70% of catheters placed in patients for 6 to 9 days and 30% for more than 10 days (29). Barbadoro et al. found that 40 (6.2%) of 641 patients had CAUTI, and the duration of hospitalization was longer for patients with CAUTI compared to those without (30). Additionally, Oumer et al. reported a 16.8% incidence rate of CAUTI symptoms in 231 patients, with increased incidence associated with factors such as diabetes, catheter insertion lasting more than 7 days, and insertion in the surgical department (31). Saint et al. found that implementing a specific program and interventions reduced the UTI rate from 2.4 to 2.05 per 1,000 patients (32).
Given the increased risk of UTIs and related complications associated with CAUTI, it is crucial to implement preventive measures to reduce the occurrence of UTIs and their complications (33, 34).
According to the findings, the prevalence of E. coli was 55.3%, and Proteus spp. was 11.4%. In the study by Togan et al., among patients with symptomatic urinary system infections (SUSI), the rates were as follows: E. coli was 10 (41.7%), Enterococcus spp. was 2 (8.3%), Klebsiella spp. was 5 (20.8%), Acinetobacter spp. was 3 (12.6%), and Candida spp. was 2 (8.3%) (35). Goodes et al. reported that among patients with SCI, the prevalence was as follows: Escherichia coli in 8 patients, Klebsiella spp. in 13 patients, Enterobacter spp. in 5 patients, Enterococcus spp. in 12 patients, Pseudomonas aeruginosa in 4 patients, and Citrobacter koseri in 1 patient (36). Bhatt et al. found that the prevalence of S. aureus and E. coli was both 12.2%, P. mirabilis was 9.8%, and S. marcescens was also 9.8% (37). Evans et al. reported the prevalence of S. aureus as 36.6%, Enterococcus faecium as 15.3%, E. coli as 14.9%, and Pseudomonas aeruginosa as 12.3% (38).
5.1. Conclusions
Given the significant prevalence of UTIs among patients, it is essential to implement preventive measures to mitigate infection risks.