1. Background
Seizures include different types, one of which is epilepsy. To be diagnosed with epilepsy, unprovoked seizures must occur (1-3). Epilepsy is defined as a clinical syndrome caused by the simultaneous discharge of a group of neurons in the brain, resulting from a change in the balance of excitation and inhibition of neurons. Therefore, many treatments aim to compensate for this imbalance (4, 5). Epilepsy is the second most common neurological disease after headaches, characterized by recurrent convulsive attacks. In 2020, the incidence of epilepsy worldwide was between 4 - 7 patients per 10,000 people, and its prevalence was estimated to be between 0.5 and 3% (6, 7).
Epilepsy is a common and serious disorder with epidemiology reported differently due to variations in study methodologies and definitions of active epilepsy (7-9). Epilepsy affects people of all ages. Although it is most commonly diagnosed in childhood and the elderly, it can occur in all age groups (10-12).
Factors affecting the incidence of epilepsy include genetic and family history, geographic region, social and economic levels, age, gender, and income, each playing a role in the incidence of epilepsy (9, 13, 14). More than 70 million people worldwide have epilepsy, with about 85% living in low- and middle-income countries (10, 15).
Although anti-epileptic drugs cause side effects, drug therapy remains the most common treatment for epilepsy. These drugs eliminate seizures in some cases and reduce their occurrence in others. However, some patients are resistant to anti-epileptic drugs and do not respond well to treatments (16). The goal of drug treatment in epilepsy is long-term, complication-free, and complete control of seizures, serving as the first treatment step for most patients. Despite advances in anti-epileptic drugs, about one-third of patients still experience frequent epileptic attacks (17, 18).
Non-adherence to medication regimens and irregular use of medications in patients with chronic diseases is a fundamental problem that reduces the effects of treatment, creates a financial burden on patients, and causes psychological problems. In patients with epilepsy, it has been shown that about 30 to 60% do not follow the treatment regimen properly (6, 19, 20). If these patients do not comply with drug treatment, they are at greater risk of increased subsequent seizures, more emergency visits to the hospital due to injuries caused by seizures, falls, and vehicle accidents (21, 22).
Epilepsy is associated with complications such as decreased quality of sleep and quality of life, restless legs syndrome, nocturnal rhythm disorder, decreased mental health, and increased stress. Convulsions and sleep affect each other, and the occurrence of convulsions, especially at night, reduces the quality of patients' sleep (1, 23). Additionally, anxiety and depression in patients with epilepsy are about eight times more prevalent than in other patients and can contribute to disability. Stress is another significant complication of this disease, which has a high prevalence in these patients. Seizures are stressful events that, due to the excessive secretion of cortisol in patients with epilepsy, can lead to chronic stress (24, 25).
Health Anxiety Inventory (HAI) occurs when a patient's health awareness is low in the context of a chronic medical condition. Illness anxiety is diagnosed when feelings or physical changes are interpreted as indicating a serious illness. Health anxiety refers to excessive and unreasonable worry or fear about having or contracting a disease that lasts for more than six months (26-28).
2. Objectives
Considering the importance and role of mental health in patients' quality of life, this study aimed to investigate the level of anxiety in patients with epilepsy at the beginning and three months after receiving anticonvulsant treatment in patients referred to the hospital.
3. Methods
3.1. Study Design and Population
This study, conducted in 2020 with the ethics code IR.MEDILAM.REC.1399.002, involved patients with epilepsy who referred to the clinics of public hospitals in Ilam city.
3.2. Inclusion and Exclusion Criteria
3.2.1. Inclusion Criteria
- Aged between 18 and 65 years
- Ability to speak Persian or Kurdish
- Informed consent to participate in the study
- Doctor's definite diagnosis of epilepsy
- Access to a telephone at home or mobile
- At least 3 months have passed since the diagnosis of the disease
3.2.2. Exclusion Criteria
- Development of any complications affecting anxiety (including the death of family members, family tensions, hospitalization of the patient, or any other significant factor)
- Death of the patient
- Only patients who were diagnosed with epilepsy for the first time and who took epilepsy medicine for the first time were included in the study; other patients were excluded.
3.3. Data Gathering
The tools used included a demographic information form (age, gender, education, etc.), the HAI, and the Beck Anxiety Inventory (BAI).
3.3.1. Health Anxiety Inventory (HAI)
This tool has 18 items, each with 4 options (scoring for each item ranges from 0 to 3 points). Each option includes a description of health and illness components in the form of a news sentence, and the subject must choose the sentence that best describes their experience. The total score ranges from 0 to 54, with a higher score indicating greater health anxiety (29-31). In Nargesi et al.'s study, the reliability of the questionnaire was confirmed with a Cronbach's alpha value of 0.75 (32).
3.3.2. Beck Anxiety Inventory (BAI)
This tool has 21 questions on a 4-point Likert Scale (not at all, mild, moderate, severe), with scores ranging from 0 to 63. A higher score indicates more anxiety (33). In Kaviani and Mousavi's study, the reliability of the tool was confirmed with a Cronbach's alpha value of 0.92 (34).
After obtaining permission from the university's research ethics committee, the researchers started data collection by visiting the clinics of educational hospitals in Ilam city, which serve as referral centers for epilepsy patients. If the patients were literate and understood the research questions, the questionnaire was completed by self-report; otherwise, it was completed through interviews. In this study, the patients used epilepsy drugs as prescribed by their attending physician. The research tools were administered before taking the drug and at intervals of one, three, and six months after starting the drug, with follow-ups by the patients. The data was analyzed using SPSS version 16 software. Descriptive tests, paired samples test, independent t-test, and ANOVA were also used.
4. Results
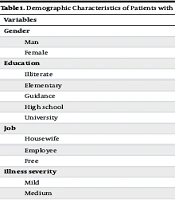
The results showed that 59.5% of the patients were male, 33.5% had received guidance, and 42% of the patients were employees. Additionally, 71% of the patients had severe illness, 59.5% had no history of underlying disease, and the mean ± SD age of the patients was 32.85 ± 9.6 years (Table 1).
| Variables | No. (%) |
|---|---|
| Gender | |
| Man | 119 (59.5) |
| Female | 81 (40.5) |
| Education | |
| Illiterate | 6 (3) |
| Elementary | 43 (21.5) |
| Guidance | 67 (33.5) |
| High school | 70 (35) |
| University | 14 (7) |
| Job | |
| Housewife | 62 (31) |
| Employee | 84 (42) |
| Free | 54 (27) |
| Illness severity | |
| Mild | 19 (9.5) |
| Medium | 142 (71) |
| Intense | 39 (19.5) |
| History of underlying disease | |
| Have a disease | 81 (40.5) |
| Without disease | 119 (59.5) |
| Age; (mean ± SD) | 32.85 ± 9.6 |
The results showed that the mean ± SD score of HAI before drug administration was 43.82 ± 7.29, and six months after drug administration, it was 17.52 ± 8.08. In terms of BAI, the mean (SD) score before drug administration was 48.66 ± 9.84, and six months after drug administration, it was 19.73 ± 0.73 (Table 2).
| Variables | Before | One Month After | Three Months After | Six Months After |
|---|---|---|---|---|
| Health Anxiety Inventory | 43.82 ± 7.29 | 34.16 ± 8.57 | 36.94 ± 8.00 | 17.52 ± 8.08 |
| P-value | - | 0.000 | 0.000 | 0.000 |
| Beck Anxiety Inventory | 48.66 ± 9.84 | 49.27 ± 8.75 | 34.08 ± 8.86 | 19.73 ± 10.73 |
| P-value | - | 0.41 | 0.000 | 0.000 |
a Values are expressed as mean ± SD.
The results of the paired samples test analysis showed that drug administration led to a decrease in the HAI score at all time points from the first month to the sixth month after drug administration (P = 0.000) (Table 3).
| Measurement Time | Paired Differences | t | Sig. | ||||
|---|---|---|---|---|---|---|---|
| Mean | Std. Deviation | Std. Error Mean | 95% Confidence Interval of the Difference | ||||
| Lower | Upper | ||||||
| First stage | 9.66500 | 5.19690 | 0.36748 | 8.94035 | 10.38965 | 26.301 | 0.000 |
| Second stage | -2.78500 | 6.25174 | 0.44206 | -3.65673 | -1.91327 | -6.300 | 0.000 |
| Third stage | 19.42000 | 2.74065 | 0.19379 | 19.03785 | 19.80215 | 100.210 | 0.000 |
Regarding the BAI score, the results showed that drug administration in the first month had no effect on reducing the BAI score (P = 0.415). However, in the subsequent months of the study, drug administration significantly decreased the BAI score of the patients (P = 0.000) (Table 4).
| Measurement Time | Paired Differences | t | Sig. | ||||
|---|---|---|---|---|---|---|---|
| Mean | Std. Deviation | Std. Error Mean | 95% Confidence Interval of the Difference | ||||
| Lower | Upper | ||||||
| First stage | -0.61500 | 10.64676 | 0.75284 | -2.09957 | 0.86957 | -0.817 | 0.415 |
| Second stage | 15.19500 | 8.75788 | 0.61928 | 13.97382 | 16.41618 | 24.537 | 0.000 |
| Third stage | 14.35000 | 8.13254 | 0.57506 | 13.21601 | 15.48399 | 24.954 | 0.000 |
5. Discussion
Chronic diseases have a significant prevalence and profoundly impact patients' physical and mental health. Neurological diseases, including epilepsy, are particularly important due to the limitations they impose on patients, their families, and those around them. These limitations can contribute to depression in both patients and their families. Given the challenges faced by patients with epilepsy, early diagnosis and treatment are essential priorities (35-38). Epilepsy is one of the most important diseases that creates certain limitations in the life of the patient, the patient's family and those around him, which can lead to the risk factor of depression in patients and the patient's family. Considering the problems that patients with epilepsy have during the course of the disease, early diagnosis and treatment is an important priority (39, 40).
In Iran, epilepsy has a notable prevalence. For example, the study by Mohammadi et al. reported a prevalence of 1.3% (41), while Safavi et al. found a prevalence of 2.5% (42). Similarly, the study by Amiri et al. reported a prevalence of 2.8% (43), Nasiri et al. found a prevalence of 1.7% (44), Ahmadpanah et al. reported 0.98% (45), and Najafi et al. reported a prevalence of 10.1% (46). Globally, the prevalence of epilepsy is approximately 7 people per 1000 (46).
The results showed that the mean ± SD age of the patients at the onset of the disease was 32.85 ± 9.6 years, and 59.5% of the patients were male. In Pakdaman et al.'s study, the mean ± SD age of disease onset was 21.1 ± 19.1 years, with an overall seizure prevalence of 4.1 per thousand people (47). The study by Vakili et al. found that 57% of the patients were male, with a mean ± SD age of 20.13 ± 22.27 years (48). In Babahajian et al.'s study, the median (percentile) age of the patients was 23.0 (21.0 - 29.0) years, with 87.6% of the patients being male (49).
In many cases, epilepsy begins in early youth and adolescence, and it has a significant prevalence among both women and men.
The results showed that before receiving the drug, the mean ± SD HAI score of the patients was 43.82 ± 7.29, and the mean ± SD BAI score was 48.66 ± 9.84. In Scott et al.'s meta-analysis of 27 articles, the prevalence of anxiety was reported as 20.2%, and the prevalence of depression as 22.9% (50). In the study by Kwong et al., conducted among adolescents with epilepsy, 32.8% of the patients had anxiety symptoms, and 22.1% had depressive symptoms (51). Anxiety disorders and depression are common and debilitating in patients with epilepsy, necessitating measures to reduce these complications (52).
According to the results of this study, drug administration reduced both the HAI and BAI scores. These findings are consistent with other studies. For instance, Choudhary et al.'s meta-analysis of interventional studies showed that cognitive behavioral therapy (CBT) reduced patients' anxiety scores (53). Similarly, Losada-Camacho's study demonstrated that pharmaceutical care reduced patients' depression scores, thereby improving their quality of life by reducing anxiety and depression (54).
5.1. Conclusions
Considering the positive effect of drug administration on reducing the HAI and BAI scores of the patients, it is suggested that drug interventions be carried out to improve the health of these patients.