1. Background
Epilepsy is a neurological disorder characterized by spontaneous and recurrent seizures. It affects approximately 3 to 5 percent of populations worldwide, leading to significant psychological and social pressures on patients (1, 2). Repeated and unpredictable seizures result in physical and mental challenges that ultimately diminish the quality of life for those affected (3). The global incidence of epilepsy is estimated at 61.4 per 100,000 person-years, with notably higher rates in low- and middle-income countries (4).
Neurological disorders, including epilepsy, are prevalent and can cause numerous side effects for patients (5-7). Epilepsy, in particular, can impact sexual function (8, 9). Research on sexual issues in epilepsy patients is limited, but available studies indicate that sexual problems are more common among these patients compared to the general population (9-11). For instance, patients with epilepsy often experience reduced sperm concentration and seminal fluid volume, which can contribute to decreased sexual satisfaction (12).
Among men, various sexual disorders include libido disorders, erectile dysfunction (ED), and ejaculation disorders. Premature ejaculation (PE) is one of the most common sexual disorders in men (13). Due to varying definitions of PE, its prevalence differs across studies. PE can severely impact a person’s sexual quality of life and mental health, particularly when it coexists with ED (14, 15).
Premature ejaculation is generally defined by a short time interval from penetration to ejaculation, occurring either before or shortly after penetration. Some sources define PE as ejaculation occurring within one minute of intercourse, while others consider ejaculation within two minutes as premature. Additionally, PE is characterized by intermittent or consistent orgasm before the desired time (16-18).
Premature ejaculation is categorized into two types. The first type involves men who are physiologically predisposed to rapid peak sexual pleasure due to shorter neural latency. The second type includes cases conditioned by psychological or behavioral factors that result in PE (19).
In diagnosing PE, doctors should consider factors such as age, the novelty of the sexual partner, and the frequency and duration of intercourse, all of which can affect the duration of stimulation (20, 21). The diagnosis of PE is primarily based on the patient's or their partner's history. It has been observed that if a doctor attempts to measure ejaculation time in a clinical setting, it often appears normal or longer than reported by the patient. Therefore, routine clinical evaluation of ejaculation time is not recommended, and diagnosis relies mainly on the time reported by the patient or their partner
Male sexual dysfunction can result from physical, psychological, or a combination of both causes. Physical causes include chronic conditions such as diabetes, reproductive system tumors, hypertension, urinary infections, and surgeries affecting nerves or organs. Psychological causes may involve psychiatric disorders, the use of psychoactive drugs, anxiety, depression, and other related issues (13, 24, 25).
2. Objectives
Considering the importance of sexual health in men, particularly those with epilepsy, this study aimed to compare PE in men with focal epilepsy and generalized tonic-clonic seizures (GTCS).
3. Methods
In this cross-sectional and observational study, patients with epilepsy were included based on specific entry and exit criteria. The total sample size comprised 200 individuals, with 100 patients having focal epilepsy and 100 patients with GTCS. The patients were evaluated by psychiatrists and neurologists.
Inclusion criteria were: Males aged 18 to 40, married, with at least 6 months of sexual activity, who provided informed consent to participate, and had a diagnosis of epilepsy as determined by the physician. Patients with additional conditions such as mental retardation, a history of sexually transmitted diseases, or a history of drug use were excluded from the study.
The tools used included a demographic profile form, the Men Sexual Health Questionnaire (MSHQ), the Sexual Quality of Life-Men (SQOL-M), and the premature ejaculation diagnostic tool (PEDT).
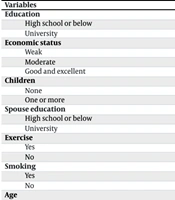
3.1. Demographic Information Form
It included questions about age, the education level of both the patient and their spouse, smoking history, exercise history, and the number of children.
3.2. Men Sexual Health Questionnaire
This tool includes three dimensions: Erection, ejaculation, and satisfaction. The items on the instrument have a response range from zero to five, with higher scores indicating better sexual performance (26). The MSHQ instrument evaluates dimensions such as erection, which includes three questions with a score range of 0 - 15; ejaculation, which includes seven questions with a score range of 0 - 35; and satisfaction, which includes six questions with a score range of 0 - 30 (26, 27).
3.3. Sexual Quality of Life-Men
This tool consists of 11 questions with scores ranging from "completely agree" (score 1) to "completely disagree" (score 6). The total score ranges from 11 to 66, with higher scores indicating a better quality of life (28, 29).
3.4. Premature Ejaculation Diagnostic Tool
This tool consists of 5 domains, with responses scored on a Likert scale from 0 to 4. Higher scores indicate a greater level of sexual disorder. A score below 8 suggests no PE, a score between 9 and 10 indicates possible PE, and a score above 11 indicates PE (30-32).
In this study, patients with a confirmed diagnosis of epilepsy, approved by a neurologist, were included. Patients who visited specialized clinics and hospitals and met the study's entry criteria were enrolled. Since all the patients were male, the interviews were conducted by a male researcher. Informed written consent was obtained from each patient before starting the questioning, and the study procedures were explained to them. The collected data were entered into SPSS statistical software with confidentiality maintained, and analyses were performed using independent t-tests, ANOVA, regression, and descriptive statistics.
4. Results
The results in Table 1 show that the mean (SD) age of patients in the focal epilepsy group was 30.09 (3.66), in the GTCS group was 30.27 (4.05), and for all patients combined was 30.18 (3.85). Additionally, 15% of all patients had experience with sports, and 15.5% had experience with smoking.
| Variables | Focal Epilepsy | GTCS | Total Epilepsy |
|---|---|---|---|
| Education | |||
| High school or below | 49 (49) | 47 (47) | 96 (48) |
| University | 51 (51) | 53 (53) | 104 (52) |
| Economic status | |||
| Weak | 65 (65) | 54 (54) | 119 (59.5) |
| Moderate | 33 (33) | 40 (40) | 73 (36.5) |
| Good and excellent | 2 (2) | 6 (6) | 8 (4) |
| Children | |||
| None | 57 (57) | 64 (64) | 121 (60.5) |
| One or more | 43 (43) | 36 (26) | 79 (39.5) |
| Spouse education | |||
| High school or below | 38 (38) | 47 (47) | 85 (42.5) |
| University | 62 (62) | 53 (53) | 115 (57.5) |
| Exercise | |||
| Yes | 18 (18) | 12 (12) | 30 (15) |
| No | 82 (82) | 88 (88) | 170 (85) |
| Smoking | |||
| Yes | 14 (14) | 17 (17) | 31 (15.5) |
| No | 86 (86) | 83 (83) | 169 (84.5) |
| Age | 30.09 ± 3.66 | 30.27 ± 4.05 | 30.18 ± 3.85 |
Abbreviation: GTCS, generalized tonic-clonic seizures.
a Values are expressed as No. (%) or mean ± SD.
According to Table 2, the mean (SD) score for the MSHQ tool was 51.81 (11.98), for the SQOL-M tool was 34.75 (9.36), and for the PEDT tool was 8.63 (4.79). Although the mean (SD) PE score in the focal epilepsy group was 9.17 (4.49) compared to 8.09 (5.04) in the GTCS group, this difference was not statistically significant.
| Variables | Focal Epilepsy | GTCS | Total Epilepsy | P-Value, F |
|---|---|---|---|---|
| MSHQ | ||||
| Erection | 6.6 ± 1.71 | 6.08 ± 1.27 | 6.7 ± 1.5 | 0.04, 4.25 |
| Ejaculation | 25.78 ± 4.63 | 21.57 ± 6.84 | 23.67 ± 6.19 | 0.000, 32.37 |
| Satisfaction | 22.47 ± 7.33 | 20.4 ± 7.94 | 21.43 ± 7.7 | 0.05, 3.67 |
| MSISQ total | 54.85 ± 10.38 | 48.77 ± 12.72 | 51.81 ± 11.98 | 0.007, 7.48 |
| SQOL-M | 36.31 ± 10.62 | 33.2 ± 7.66 | 34.75 ± 9.36 | 0.001, 10.47 |
| PEDT | 9.17 ± 4.49 | 8.09 ± 5.04 | 8.63 ± 4.79 | 0.76, 0.09 |
Abbreviations: MSHQ, Men’s Sexual Health Questionnaire; SQOL-M, Sexual Quality of Life-Men; PEDT, premature ejaculation diagnostic tool; GTCS, generalized tonic-clonic seizures.
The findings showed a significant relationship between the PEDT score, the SQOL-M score, and the MSHQ score (P < 0.05). The MSHQ score and SQOL-M score were reported to be lower in patients with PE disorder (Table 3).
| Variables | SQOL-M | PEDT | MSHQ | ||||||
|---|---|---|---|---|---|---|---|---|---|
| P | R | F | P | R | F | P | R | F | |
| MSHQ | 0.000 | 0.28 | 17.63 | 1 | 1 | 1 | |||
| SQOL-M | 1 | 1 | 1 | 0.03 | - 0.15 | 4.65 | |||
| PEDT | 1 | 1 | 1 | 0.000 | 0.47 | 58.74 | |||
Abbreviations: MSHQ, Men’s Sexual Health Questionnaire; SQOL-M, Sexual Quality of Life-Men; PEDT, premature ejaculation diagnostic tool.
The results showed that 29.5% of patients were in the definitive PE status, 8.5% were in the possible PE status, and 62% were in the no PE status (Table 4).
| Variables | Focal Epilepsy | GTCS | Total Epilepsy |
|---|---|---|---|
| No PE | 55 (55) | 69 (69) | 124 (62) |
| Possible PE | 12 (12) | 5 (5) | 17 (8.5) |
| Definitive PE | 33 (33) | 26 (26) | 59 (29.5) |
| Total | 100 (100) | 100 (100) | 200 (100) |
Abbreviation: PE, premature ejaculation; GTCS, generalized tonic-clonic seizures.
a Values are expressed as No. (%).
5. Discussion
This study aimed to compare PE in men with focal epilepsy to those with GTCS. Sexual problems in both men and women with epilepsy have been investigated in various studies. The results of this study will be compared with findings from other studies across several categories: The general population, patients with epilepsy within Iran, and patients outside Iran.
In a meta-analysis conducted by Ramezani et al. in Iran, 11 articles were reviewed, covering diverse patient groups, including those with heart problems, diabetes, dialysis, neurological issues, and others. The analysis found that the prevalence of ED in men was 56.1% (33). Porst et al. reported the prevalence of PE as 24% in the United States, 20.3% in Germany, and 20% in Italy. Men with PE were also found to be at higher risk for other sexual disorders, such as ED, sexual aversion, and anorgasmia (14). Additionally, Tang and Khoo reported a 46.9% prevalence of PE in a study involving 207 men aged 18 - 70 years (34). These findings are consistent with this study's results on the prevalence of PE in patients with epilepsy.
Nikoobakht et al. included 80 male patients aged 22 to 50, all diagnosed with epilepsy. They found that 42.5% of the patients had ED, and 11.3% had PE. The study also highlighted a significant relationship between seizure type and frequency with erectile function, orgasmic function, and sexual desire (35). Mazdeh et al. examined 35 married patients and found ED in 48.1% of those on sodium valproate and 51.9% of those on carbamazepine. The study also categorized ED severity, noting 11 patients with moderate conditions, 15 with moderate to mild conditions, 16 with mild conditions, and 18 without ED (36). These previous studies, which highlight the presence of sexual disorders among patients with epilepsy in Iran, are consistent with the results of this study.
In the study by Mazdeh et al., which included 80 married women with epilepsy, disorders were reported as follows: 41% for the state of desire, 35% for the state of arousal, 48% for the state of lubrication, and 41% for the state of orgasm (37). These results are consistent with the findings of this study regarding the prevalence of sexual problems in patients with epilepsy.
Henning et al.'s study, which examined 171 patients with epilepsy, found that the most commonly reported issues were erectile problems, decreased libido, vaginal dryness, and orgasm-related issues. The prevalence of sexual problems was 63.3% in men and 75.3% in women. In men, the reported problems included sexual dysfunction (63.3%), delayed ejaculation (5.6%), reduced sexual desire (25.6%), feelings of sexual deviation (5.6%), orgasm difficulties (13.3%), and PE (15.6%) (38).
In Calabrò et al.'s study of 30 men with epilepsy, aged 20 to 53 years, the prevalence rates were as follows: Retarded ejaculation 3.8%, ED 3.3%, PE 6.7%, hyperactive desire 1.7%, hypoactive desire 8.3%, and 21.7% of patients reported no sexual disorders (39). Similarly, Sureka et al. found that 66% of patients reported sexual dysfunction, which included ED (36%), hypoactive sexual desire (0.4%), PE (26%), and 34% of patients reported no sexual dysfunction (40).
One limitation of this study is the potential influence of cultural factors. Conducted in Ilam city, some patients may have been reluctant to discuss sexual problems due to cultural reasons. Therefore, it is recommended to conduct further studies with larger sample sizes.
5.1. Conclusions
The findings indicate a significant prevalence of sexual disorders, including PE, in both groups of patients with epilepsy. Consequently, it is essential to implement both pharmacological and non-pharmacological interventions to reduce the incidence of PE in these patients.