1. Introduction
Moya-Moya disease (MMD) is a rare, chronic, and spontaneous steno-occlusive condition involving the internal carotid artery and its branches. It results in the formation of disorganized compensatory vascular collaterals, which lead to recurrent strokes due to the occlusion of the terminal internal carotid arteries. The pathogenesis of MMD remains poorly understood, although recent genetic studies have identified a potential susceptibility gene (1). Research on familial aggregation indicates that relatives of patients with MMD are at a 30- to 40-fold higher risk of developing the condition compared to the general population. Up to 15% of MMD cases may have a positive family history (2).
Treatment options for MMD include surgical revascularization to prevent ischemic stroke, endovascular treatments such as embolization of a ruptured aneurysm in the collateral vessels, and angioplasty of narrowed segments with or without stenting (3). Non-surgical or conservative treatments may also be considered.
2. Case Presentation
A 55-year-old male, married with a BMI of 24.8, was admitted to our hospital. During admission, he reported weakness in the left upper extremity followed by weakness in the left lower extremity, lasting approximately 3 hours during the night. The patient also reported a history of dizziness, confusion, memory impairment, and inability to stand, possibly indicating previous transient ischemic attacks. There were no neurocutaneous markers or facial asymmetry observed. He had high blood pressure (140/90) but no history of head injury. The patient reported allergies to peanuts and other nuts, some antibiotics, and spicy foods.
His medication history included Plavix 75 mg, atorvastatin 40 mg, losartan 25 mg, and aspirin 80 mg. His family history included eight siblings, five of whom had a history of cardiovascular disease. Some siblings had undergone open-heart surgeries, and two brothers had died following myocardial infarctions. The patient’s father had high blood pressure.
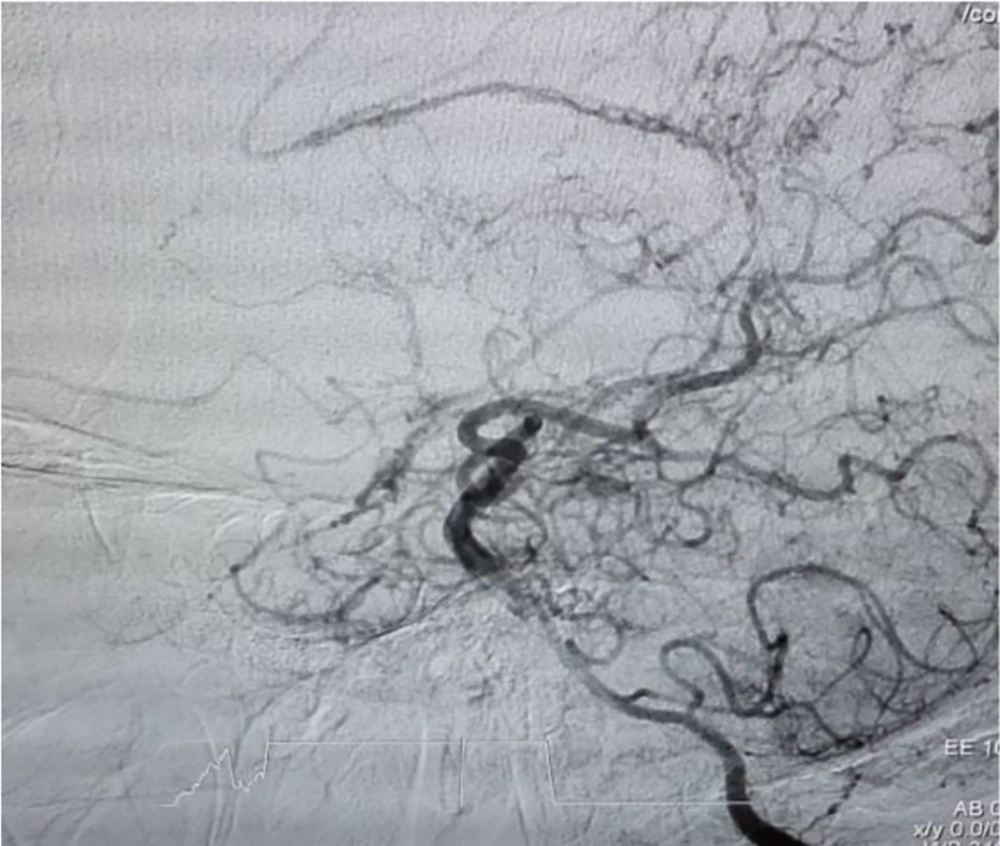
On neurological examination, the patient's gait was hemiplegic, with decreased tone on the left side. Power was 2/5 in the left upper and lower extremities, deep tendon reflexes were exaggerated, and an extensor plantar response was noted on the left side. Initially, the patient was diagnosed with a stroke, and digital subtraction angiography (DSA) was performed. The bilateral angiography revealed dominant lumen and blood flow in the left intra-cranial vertebral artery. Multiple, well-developed plexuses of MMD were detected in the basal cortical areas (Figure 1). The right superior cerebral artery (SCA) had a normal lumen with good blood flow.
Upon discharge, the patient’s symptoms included memory impairment, but his gait and muscle tone were normal (5/5), and his blood pressure was within normal limits (130/75). The patient was treated conservatively and had a favorable outcome. Periodic follow-up was recommended.
3. Discussion
Reports of Moya-Moya disease in Iran are very rare (4). Age and sex are important factors in its distribution, with notable age ranges of 5 - 9 years and 35 - 39 years. Two types of MMD have been identified: The ischemic type, which is found in the pediatric population, and the hemorrhagic type, which is seen in adults. Moya-Moya disease is more commonly diagnosed in females (5). The primary clinical features of MMD include cerebrovascular complications such as transient ischemic attacks, ischemic strokes, and convulsions. The presentation of the disease can vary depending on the age at diagnosis (6).
In the present case report, the patient had high blood pressure and likely had a familial risk of MMD among first-degree relatives. A 2014 report described individuals in 20 families with actin alpha 2 (ACTA2) genetic mutations, a major component of the contractile apparatus in the vascular smooth muscle cell (SMC)-specific isoform of α-actin located throughout the arterial system. The report indicated that mutation carriers might experience a range of vascular diseases, including premature onset of coronary artery disease, premature ischemic strokes (including MMD), as well as thoracic aortic aneurysms and dissections (7). In this case report, cardiovascular problems and a history of strokes in first-degree relatives may suggest undiagnosed MMD.
5.1. Conclusions
This case highlights the probable genetic predisposition as a significant factor in MMD pathogenesis. These findings could guide future genetic studies and preventive counseling with a focus on the clinical evaluation of serious adverse events.