1. Background
Acute stroke is characterized by the interruption of blood flow to the brain, which can result from either a ruptured blood vessel (hemorrhagic stroke) or a blockage caused by a clot (ischemic stroke). Both conditions deprive the brain of essential nutrients and oxygen, leading to tissue damage. Notably, ischemic strokes account for approximately 87% of all stroke cases (1). Stroke is a major cause of mortality and long-term disability, consistently ranking as a leading cause of death and varying degrees of impairment, particularly among vulnerable populations. Beyond the challenges of rehabilitation, stroke imposes significant economic and social burdens on societies worldwide. In the United States alone, its annual incidence is approximately 700,000 cases (2).
Iran currently lacks a national stroke registry, leading to significant disparities in the reported stroke cases across different regions. The incidence of stroke varies widely, ranging from 22 to 140 cases per 100,000 population (3, 4). Compared to individuals in some developed countries, Iranians experience ischemic stroke nearly a decade earlier, contributing to a higher fatality rate. The 30-day mortality rate for stroke is approximately 10%, while 90% of survivors often face long-term disabilities (5). Intravenous recombinant tissue plasminogen activator (IV-rtPA) is a highly effective thrombolytic therapy for acute ischemic stroke (AIS). Its administration in specialized stroke centers significantly enhances survival rates and functional outcomes for patients (6, 7). The American Stroke Association (ASA) has introduced the concept of primary and comprehensive stroke centers, along with designated emergency hospitals, to ensure adequate care for stroke patients and improve the overall quality of treatment (8).
2. Objectives
This study aimed to investigate the factors contributing to the non-administration of IV-rtPA in eligible patients with AIS and to understand why many Iranian medical centers withhold this treatment from eligible patients. Our findings highlight key barriers to optimal stroke care in Iran and emphasize the urgent need for targeted interventions to improve access to evidence-based therapies.
3. Methods
This cross-sectional descriptive-analytical study was conducted at Shahid Beheshti Hospital in Qom, following approval from the ethics committee of Qom University of Medical Sciences (Approval ID: IR.MUQ.REC.1401.181). The study included patients experiencing acute strokes who were admitted to Shahid Beheshti Hospital between November 2021 and September 2022. Eligible participants were adults aged 18 years or older who met the criteria for Code Stroke activation but did not receive thrombolytic therapy. The minimum sample size was calculated based on the results of the study by Hatamabadi et al. (9) and considering the percentage of non-receipt of rTPA due to delays, which was estimated at 70%, resulting in a sample size of 322 individuals. A total of 322 patients with suspected AIS were initially screened during the study period. Of these, 178 patients met the inclusion criteria and were thoroughly examined and analyzed.
Data collected for these patients included demographic information (age and gender), National Institutes of Health Stroke Scale (NIHSS) score upon arrival, onset-to-door time (the interval between symptom onset and hospital arrival), chief complaint, risk factors (such as a history of hypertension, dyslipidemia, diabetes mellitus, cerebrovascular disease, coronary artery disease, and smoking), initial CT scan findings, and reasons for not administering thrombolytic therapy. The collected data were analyzed using SPSS version 22 statistical software. The chi-square test was applied to analyze qualitative variables, while the t-test was used for quantitative variables. A P-value of < 0.05 was considered statistically significant for all tests.
4. Results
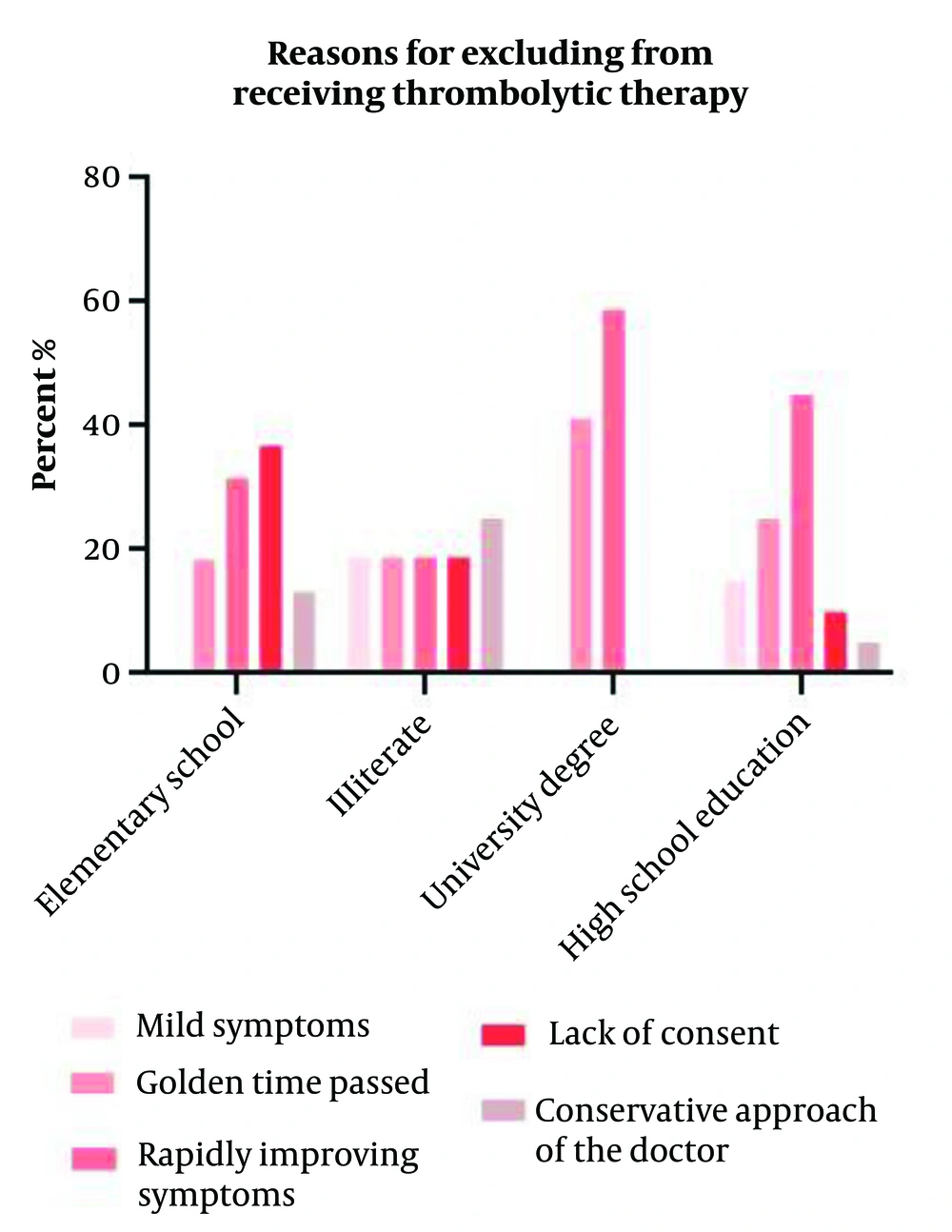
A total of 178 patients were analyzed, with an average age of 66.28 years (SD 12.77), ranging from 34 to 93 years. Of these, 43.3% were female, and 56.7% were male. Thrombolytic therapy was administered to 87 patients (48.9%), while 91 patients (51.1%) did not receive the treatment (Table 1). The reasons for not receiving thrombolysis included symptom improvement (37.4%), late arrival beyond 4.5 hours (24.2%), lack of consent (20.9%), the physician’s conservative approach (11%), and mild stroke severity (6.6%) (Table 1). A significant relationship was found between non-receipt of thrombolysis and both age (P < 0.001) and education level (P < 0.002), with lower education associated with higher dissatisfaction (Table 2). The mean NIHSS score on admission was 10.72 (SD 3.9), with significant associations between NIHSS scores and reasons for non-receipt of IV-rtPA (P < 0.001) (Table 3).
| Variables | No. (%) |
|---|---|
| Gender | |
| Female | 77 (43.3) |
| Men | 101 (56.7) |
| Education level | |
| Illiterate | 24 (13.5) |
| Elementary school | 68 (38.2) |
| High school | 48 (27.0) |
| Some university degree | 38 (21.3) |
| Place of residence | |
| Rural areas | 30 (16.9) |
| City | 148 (83.1) |
| Modes of arrival | |
| Ambulance | 74 (41.6) |
| Personal vehicle | 104 (58.4) |
| Marital status | |
| Married | 169 (94.9) |
| Single | 9 (5.1) |
| Causes for not receiving thrombolytic therapy | |
| Mild symptoms | 6 (3.4) |
| Exceeded the golden time | 22 (12.4) |
| Clinical improvement | 34 (19.1) |
| Lack of consent | 19 (10.7) |
| Conservative approach | 10 (5.6) |
| Missing system | 87 (48.9) |
| Past medical history | |
| Hypertension | |
| Yes | 81 (45.5) |
| No | 97 (54.5) |
| Hyperlipidemia | |
| Yes | 22 (12.4) |
| No | 156 (87.6) |
| Diabetes mellitus | |
| Yes | 55 (30.9) |
| No | 123 (69.1) |
| Cardiovascular disease | |
| Yes | 38 (21.3) |
| No | 140 (78.7) |
| Past stroke | |
| Yes | 27 (15.2) |
| No | 151 (84.8) |
| Smoking cigarettes | |
| Yes | 14 (7.9) |
| No | 140 (78.7) |
| Received thrombolytic therapy | |
| Yes | 87 (48.9) |
| No | 91 (51.1) |
| Past Medical History | Reasons for Excluding from Not Receiving Thrombolytic Therapy | Total | P-Value | ||||
|---|---|---|---|---|---|---|---|
| Mild Symptoms | Exceeded 4.5-Hour Window | Rapidly Improving Symptoms | Lack of Consent | Physician’s Conservative Approach | |||
| HTN | 0.196 | ||||||
| Yes | 5 (12.5) | 8 (20.0) | 17 (42.5) | 6 (15.0) | 4 (10.0) | 40 (100.0) | |
| No | 1 (2.0) | 14 (27.5) | 17 (33.3) | 13 (25.5) | 6 (11.8) | 51 (100.0) | |
| Total | 6 (6.6) | 22 (24.2) | 34 (37.4) | 19 (20.9) | 10 (11.0) | 91 (100.0) | |
| DM | 0.139 | ||||||
| Yes | 2 (7.4) | 8 (29.6) | 7 (25.9) | 4 (14.8) | 6 (22.2) | 27 (100.0) | |
| No | 4 (6.3) | 14 (21.9) | 27 (42.2) | 15 (23.4) | 4 (6.3) | 64 (100.0) | |
| Total | 6 (6.6) | 22 (24.2) | 34 (37.4) | 19 (20.9) | 10 (11.0) | 91 (100.0) | |
| HLP | 0.619 | ||||||
| Yes | 0 (0.0) | 5 (38.5) | 4 (30.8) | 3 (23.1) | 1 (7.7) | 13 (100.0) | |
| No | 6 (7.7) | 17 (21.8) | 30 (38.5) | 16 (20.5) | 9 (11.5) | 78 (100.0) | |
| Total | 6 (6.6) | 22 (24.2) | 34 (37.4) | 19 (20.9) | 10 (11.0) | 91 (100.0) | |
| CVD | 0.236 | ||||||
| Yes | 0 (0.0) | 6 (28.6) | 9 (42.9) | 2 (9.5) | 4 (19.0) | 21 (100.0) | |
| No | 6 (8.6) | 16 (22.9) | 25 (35.7) | 17 (24.3) | 6 (8.6) | 70 (100.0) | |
| Total | 6 (6.6) | 22 (24.2) | 34 (37.4) | 19 (20.9) | 10 (11.0) | 91 (100.0) | |
| History of CVA | 0.011 | ||||||
| Yes | 3 (14.3) | 2 (9.5) | 6 (28.6) | 4 (19.0) | 6 (28.6) | 21 (100.0) | |
| No | 3 (4.3) | 20 (28.6) | 28 (40.0) | 15 (21.4) | 4 (5.7) | 70 (100.0) | |
| Total | 6 (6.6) | 22 (24.2) | 34 (37.4) | 19 (20.9) | 10 (11.0) | 91 (100.0) | |
| History of Smoking | 0.794 | ||||||
| Yes | 0 (0.0) | 2 (33.3) | 3 (50.0) | 1 (16.7) | 0 (0.0) | 6 (100.0) | |
| No | 6 (7.1) | 20 (23.5) | 31 (36.5) | 18 (21.2) | 10 (11.8) | 85 (100.0) | |
| Total | 6 (6.6) | 22 (24.2) | 34 (37.4) | 19 (20.9) | 10 (11.0) | 91 (100.0) | |
a Values are expressed as No. (%).
| Dependent Variable | Reasons for Excluding from Not Receiving Thrombolytic Therapy | Reasons for Excluding from not Receiving Thrombolytic Therapy | Mean Absolute Difference | P-Value a |
|---|---|---|---|---|
| Age | Mild symptoms | Golden time passed | 9.89394 | 0.362 |
| Rapidly improving symptoms | 13.16667 | 0.092 | ||
| Lack of consent | 0.40351 | 1.000 | ||
| Conservative approach | -7.73333 | 0.706 | ||
| Golden time passed | Mild symptoms | -9.89394 | 0.362 | |
| Rapidly improving symptoms | 3.27273 | 0.845 | ||
| Lack of consent | -9.49043 | 0.082 | ||
| Conservative approach | -17.62727 | 0.002 | ||
| Rapidly improving symptoms | Mild symptoms | -13.16667 | 0.092 | |
| Golden time passed | -3.27273 | 0.845 | ||
| Lack of consent | -12.76316 | 0.002 | ||
| Conservative approach | -20.90000 | < 0.001 | ||
| Lack of consent | Mild symptoms | -0.40351 | 1.000 | |
| Golden time passed | 9.49043 | 0.082 | ||
| Rapidly improving symptoms | 12.76316 | 0.002 | ||
| Conservative approach | -8.13684 | 0.394 | ||
| Physician’s conservative approach | Mild symptoms | 7.73333 | 0.706 | |
| Golden time passed | 17.62727 | 0.002 | ||
| Rapidly improving symptoms | 20.90000 | < 0.001 | ||
| Lack of consent | 8.13684 | 0.394 | ||
| NIHSS | Mild symptoms | Golden time passed | -8.84848 | < 0.001 |
| Rapidly improving symptoms | -6.72549 | 0.002 | ||
| Lack of consent | -7.87719 | 0.001 | ||
| Conservative approach | -9.96667 | < 0.001 | ||
| Golden time passed | Mild symptoms | 8.84848 | < 0.001 | |
| Rapidly improving symptoms | 2.12299 | 0.305 | ||
| Lack of consent | 0.97129 | 0.937 | ||
| Conservative approach | -1.11818 | 0.948 | ||
| Rapidly improving symptoms | Mild symptoms | 6.72549 | 0.002 | |
| Golden time passed | -2.12299 | 0.305 | ||
| Lack of consent | -1.15170 | 0.853 | ||
| Conservative approach | -3.24118 | 0.171 | ||
| Lack of consent | Mild symptoms | 7.87719 | 0.001 | |
| Golden time passed | -.97129 | 0.937 | ||
| Rapidly improving symptoms | 1.15170 | 0.853 | ||
| Conservative approach | -2.08947 | 0.670 | ||
| Conservative approach of the doctor | Mild symptoms | 9.96667 | < 0.001 | |
| Golden time passed | 1.11818 | 0.948 | ||
| Rapidly improving symptoms | 3.24118 | 0.171 | ||
| Lack of consent | 2.08947 | 0.670 |
Abbreviation: NIHSS, National Institutes of Health Stroke Scale.
a P < 0.05 was considered statistically significant.
Comorbidities were prevalent, with hypertension (45.5%) being the most common, followed by diabetes (30.9%), cardiovascular disease (21.3%), prior stroke (15.2%), hyperlipidemia (12.4%), and a history of smoking (7.9%). However, no significant associations were observed between the non-receipt of thrombolysis and comorbidities such as hypertension, diabetes, hyperlipidemia, cardiovascular disease, or smoking. A significant relationship was noted between a history of stroke and the physician’s conservative approach to treatment (P < 0.01), which was cited in 28.6% of cases for patients with prior strokes, compared to 5.7% for those without (Table 3).
5. Discussion
In 1995, the U.S. Food and Drug Administration approved the use of intravenous recombinant tissue plasminogen activator (IV-rtPA) for thrombolytic treatment in patients with AIS within a 4.5-hour window (10). Approximately 33% of eligible patients did not receive IV-rtPA due to various reasons (11). In our study, the incidence of AIS was higher among males compared to females, with 43.3% (77 patients) being female and 56.7% (101 patients) being male. A study conducted by Sharifi Razavi et al. investigated the factors influencing the duration of hospitalization for patients with AIS who received intravenous thrombolysis. Among the 173 cases analyzed, 95 patients (54.9%) were male, and 78 patients (45.1%) were female (12). Another study, conducted by Hatamabadi et al. at Mazandaran University of Medical Sciences in 2013, aimed to identify barriers to the timely initiation of thrombolytic treatment in AIS patients. The study included 151 patients, of whom 97 (64.2%) were male and 54 (35.8%) were female (9).
In this study, 91 patients (51.1%) did not receive thrombolytic therapy. The reasons for withholding thrombolytic therapy in these cases can be categorized into five groups: 37.4% (34 patients) experienced symptom improvement, 24.2% (22 patients) arrived beyond the 4.5-hour therapeutic window, 20.9% (19 patients) declined treatment due to lack of informed consent, 11% (10 patients) were affected by the physician's conservative approach, and 6.6% (6 patients) were not treated due to the mild severity of their stroke (Figure 1). A study conducted by P.A. Barber et al. in 2001 investigated the reasons for excluding patients with AIS from receiving IV-rtPA. The study found that 27% of patients (314 out of 1,168) were hospitalized within 3 hours of symptom onset, and of these, 84 patients (26.7%) received IV-rtPA. The main reasons for exclusion in the subgroup hospitalized within 3 hours were mild symptoms (13.1%), clinical improvement (18.2%), lack of consent (13.6%), delays in conducting initial examinations (8.9%), and the presence of significant underlying conditions (8.3%) (13).
In 2019, Zhou et al. conducted a study in Hubei, China, to evaluate the utilization of thrombolytic treatment and identify barriers in patients with ischemic stroke. Among 2,096 AIS patients, only 3.8% received thrombolysis (14). Of the 709 neurologists surveyed, 66.0% reported using thrombolysis for AIS patients. The main factors contributing to the underutilization of thrombolysis included delayed patient arrival, concerns about potential complications, and the presence of mild stroke symptoms or rapid clinical improvement. The study highlighted several factors that influence the likelihood of receiving thrombolytic treatment, including early hospital admission, use of emergency medical services for transportation, absence of a prior stroke history, and a low NIHSS score (< 4). Additionally, patient education level and the experience of the neurologist were found to play significant roles in determining thrombolysis utilization (14).
In this study, the most common reason for not administering thrombolytic therapy was mild or rapidly improving symptoms, which accounted for 37.4% of cases. Patients who experienced symptom improvement had a lower average age of 62.5 years compared to other groups. This finding suggests that the progression of AIS tends to be more favorable in younger individuals. The average age of stroke onset in Iran appears to be lower than in developed countries. Our findings are consistent with research conducted by Azarpazhooh et al., which highlights that the incidence of stroke in Iran is significantly higher than in many Western countries, with strokes occurring at younger ages (3). The results of the present study indicate that key factors preventing the administration of thrombolytic therapy in AIS patients were delayed hospital arrival and lack of consent from family members. Together, these two factors accounted for approximately 45% of the reasons for not administering IV-rtPA.
In developing countries, significant variability exists in the time it takes for AIS patients to reach hospitals. For instance, a study by Hatamabadi et al. in northern Iran reported that 68.7% of AIS patients did not arrive at the hospital within the time window necessary for IV-rtPA administration (9). In a cohort study conducted in northeastern Iran by Azarpazhooh et al., 85.6% of AIS patients were ineligible for thrombolytic therapy due to late hospital arrival (3). In contrast, our study revealed a notable finding: Approximately half of the patients examined received IV-rtPA. This proportion exceeds the results of similar studies conducted in local medical centers across Iran and is comparable to findings reported in studies conducted globally (15). In 2016, a telestroke network in the USA conducted 744 tele-consultations for emergencies and suspected strokes. Among these, 247 patients received IV-rtPA, with 33.2% experiencing positive outcomes. Of the remaining 497 patients evaluated, 244 did not have a stroke but presented with stroke-like symptoms, while 53 were diagnosed with a transient ischemic attack (TIA). Overall, 55% of eligible patients received thrombolytic therapy (16). There is a significant correlation between patients' education level and their consent to receive IV-rtPA (Table 4). Dissatisfaction with thrombolytic therapy was predominantly observed in individuals with an education level below high school. A higher level of education appears to increase the likelihood of providing informed consent. Both educational attainment and access to rapid transportation to the hospital were crucial factors influencing early hospital arrival and decision-making regarding thrombolytic therapy.
| Variables | Reasons for Excluding from Not Receiving Thrombolytic Therapy | Total | P-Value | ||||
|---|---|---|---|---|---|---|---|
| Mild Symptoms | Exceeded 4.5-Hour Window | Rapidly Improving Symptoms | Lack of Consent | Physician’s Conservative Approach | |||
| Gender | 0.758 | ||||||
| Female | 2 (5.1) | 11 (28.2) | 16 (41.0) | 7 (17.9) | 3 (7.7) | 39 (100.0) | |
| Male | 4 (7.7) | 11 (21.2) | 18 (34.6) | 12 (23.1) | 7 (13.5) | 52 (100.0) | |
| Total | 6 (6.6) | 22 (24.2) | 34 (37.4) | 19 (20.9) | 10 (11.0) | 91 (100.0) | |
| Education level | 0.002 | ||||||
| Illiterate | 3 (18.8) | 3 (18.8) | 3 (18.8) | 3 (18.8) | 4 (25.0) | 16 (100.0) | |
| Elementary school | 0 (0.0) | 7 (18.4) | 12 (31.6) | 14 (36.8) | 5 (13.2) | 38 (100.0) | |
| Diploma | 3 (15.0) | 5 (25.0) | 9 (45.0) | 2 (10.0) | 1 (5.0) | 20 (100.0) | |
| University degree | 0 (0.0) | 7 (41.2) | 10 (58.8) | 0 (0.0) | 0 (0.0) | 17 (100.0) | |
| Total | 6 (6.6) | 22 (24.2) | 34 (37.4) | 19 (20.9) | 10 (11.0) | 91 (100.0) | |
| Marital status | 0.792 | ||||||
| Married | 6 (6.7) | 22 (24.4) | 33 (36.7) | 19 (21.1) | 10 (11.1) | 90 (100.0) | |
| Single | 0 (0.0) | 0 (0.0) | 1 (100.0) | 0 (0.0) | 0 (13.5) | 1 (100.0) | |
| Total | 6 (6.6) | 22 (24.2) | 34 (37.4) | 19 (20.9) | 10 (11.0) | 91 (100.0) | |
| Location of living | 0.726 | ||||||
| Rural areas | 2 (9.1) | 7 (31.8) | 6 (27.3) | 4 (18.2) | 3 (13.6) | 22 (100.0) | |
| City | 4 (5.8) | 15 (21.7) | 28 (40.6) | 15 (21.7) | 7 (10.1) | 69 (100.0) | |
| Total | 6 (6.6) | 22 (24.2) | 34 (37.4) | 19 (20.9) | 10 (11.0) | 91 (100.0) | |
a Values are expressed as No. (%).
An analysis of education levels among patients revealed that 21.3% had a university education, while the remaining 78.7% had only primary or high school education, or were illiterate. These factors contribute to a low perception of threat, a tendency to underestimate the severity of symptoms, and poor recognition of stroke warning signs. Additionally, cultural and perceptual barriers play a significant role in delaying the presentation of AIS patients to the emergency department. A 2016 review reported by the American Academy of Neurology analyzed the cases of 124 eligible AIS patients who arrived at a hospital in China within 2 hours of symptom onset. The findings revealed that only 22.6% of these patients received IV-rtPA. The most common reason for not administering thrombolytic therapy was patient or family refusal (74%), followed by physicians opting for a conservative approach (10%) and the presence of mild or rapidly improving symptoms (9%), among other factors.
The academy’s assessment highlighted that the current utilization of IV-rtPA remains below expectations, raising public concern. However, it is anticipated that rapid advancements in healthcare systems and increased public awareness will significantly improve the use of thrombolytic therapy in China (17).
A significant correlation was observed between the factors contributing to the non-receipt of thrombolytic therapy and a patient's history of stroke (Table 2). Patients with a prior stroke were more likely to attribute their non-receipt of thrombolytic therapy to their physician's conservative approach (28.6% of cases) compared to those without a history of stroke (5.7%). However, this represents only one of the factors influencing non-receipt of therapy. Notably, individuals with a prior stroke history exhibited shorter time intervals between symptom onset and hospital admission, as well as faster treatment initiation, compared to those experiencing their first stroke.
In 2013, a study conducted on 100 AIS patients at Buali Hospital in Qazvin, Iran, found that 33% had an NIHSS score of 0 - 5, while 38% had a score of 5 - 10, indicating their eligibility for thrombolytic therapy (18). In another study, the average NIHSS score recorded before treatment was 11 in 87.7% of the patients (19). A study by Atena Sharifi Razavi et al. also investigated the factors influencing hospitalization duration in AIS patients who received intravenous thrombolysis. The study reported an average NIHSS score of 10.64 ± 4.4 (12). In this study, the NIHSS was an important parameter considered. The average score was 10.7 ± 3.9, with a minimum score of 2 and a maximum score of 28. A significant relationship was observed between the NIHSS score and the reasons for not receiving thrombolytic therapy (Table 3). The average NIHSS score in the group that did not receive thrombolytic therapy due to mild stroke severity was 3.33, which is lower than the overall average and the averages of other groups. This difference is expected and aligns with the NIHSS grading scale, where mild cases typically receive lower scores. Overall, the mean and range of NIHSS scores in this study are consistent with findings from similar studies, indicating alignment with previously reported results.
5.1. Limitations
It is important to note that the medical records section at Shahid Beheshti Hospital did not have access to documents and files for certain cases that could have been included in this study. As a result, the study was conducted using only the available and accessible records.
5.2. Conclusions
In conclusion, our study identified delayed hospital admission beyond the 4.5-hour window as the primary barrier to receiving thrombolytic therapy for AIS. Among patients presenting within 4.5 hours, key reasons for withholding thrombolysis included clinical improvement, lack of consent from patients or their families, and mild, non-disabling symptoms. Raising public awareness about the symptoms, risks, and complications of stroke is essential to encourage prompt action and reduce delays in reaching medical centers. Public education campaigns, such as 'Know Stroke' initiatives and mass media outreach, should emphasize the importance of seeking immediate and timely treatment to minimize the risk of disability or permanent damage.