1. Background
Throughout life, individuals may lose teeth due to various causes, including caries, trauma, falls, periodontal diseases, and conflicts. Dental implants are a successful treatment method for replacing missing teeth. Compared to other therapeutic prostheses, dental implants have a higher survival and success rate. An ideal implant resembles a natural tooth in appearance and possesses beauty, strength, and durability. The success of implant placement is crucial (1-5). Patients of all ages are exposed to pathogenic microorganisms; however, in middle and old age, the risk of pathogenic microorganisms affecting individuals increases due to chronic diseases. A critical prerequisite for implant success is its initial stability, which is determined by the resistance or friction between the implant and the bone during placement (6).
Dental implants can experience various complications, categorized as biomechanical and biological. Patients seeking implant installation face issues such as the presence of microorganisms, mucositis around the implant, and peri-implantitis. Peri-implant mucositis is the inflammation of soft tissue around dental implants, while peri-implantitis involves an inflammatory reaction with the loss of bone supporting the implant (7-10). These complications result from bacterial accumulation around the implant and can lead to implant loss. Gram-negative bacteria, often responsible for gum disease, play a significant role in implant loss (11).
The common age range for implant placement is middle to old age, where patients often face mouth and dental issues alongside dysfunction of other body organs due to chronic and non-chronic diseases (12-15). Stroke is a prevalent condition leading to hospital visits in middle and old age (16, 17). There is a relationship between dental diseases and stroke; studies indicate that dental diseases such as tooth decay, periodontitis, and tooth loss can influence stroke occurrence (18-20). Stroke is a leading cause of disability and the second leading cause of death worldwide. In a study by Farzadfard et al., 65% of stroke patients died or remained disabled during a 5-year follow-up (21, 22). Disability from stroke affects patients' quality of life and lifestyle, causing complications such as hemiplegia, social communication issues, physical activity limitations, speech disorders, economic pressure, prolonged hospital stays, and inability to perform daily activities (23-26).
Given the prevalence of complications in stroke patients, attention to their oral and dental health is crucial. The presence of pathogenic microorganisms in these patients endangers their health and jeopardizes implant success. Successful implant treatment depends on the absence of inflammation in tissues surrounding the implant, as bacterial colonization, streptococci, anaerobic bacteria, and other pathogenic microorganisms can disrupt implant function (27-30).
2. Objectives
This study aimed to determine the number of microorganisms around bone level and tissue level implants after six months of loading in stroke patients in Ilam city.
3. Methods
This study was conducted on a group of patients who visited dental clinics and offices for implant placement. A total of 30 patients were examined regarding the number of microorganisms around bone-level (15 patients) and tissue-level (15 patients) implants.
The inclusion criteria for the study included patients who had suffered a stroke within the last 6 months to 2 years, as confirmed by their clinical records in the hospital. Additional criteria included obtaining informed written consent for participation, referral for implant placement, a doctor's confirmation of the necessity for implant placement, expert approval by a neurologist following neurological screening, the absence of critical health issues, and residency in Ilam city.
Exclusion criteria included the occurrence of any life-threatening condition or disease (such as death, accidents, or hospitalization), any traumatic injury to the mouth and teeth, and the patient's unwillingness to continue participation in the study.
The study was conducted by examining patients who visited clinics and offices in Ilam city for implant placement. If the patients met the inclusion criteria, they underwent implant placement, and a total of 30 patients were included in the study. Stroke patients were monitored for 6 months after implant placement to assess the number of microorganisms around bone-level and tissue-level implants. The collected data were analyzed using SPSS version 16 software with descriptive and analytical statistical tests.
All investigations related to the prevalence of microorganisms were conducted under standardized laboratory conditions, including the use of identical laboratory kits and devices. Additionally, all guidelines and ethical standards set by the University Research Ethics Committee were strictly followed, as outlined in the Code of Ethics in Research under the reference number IR.MEDILAM.REC.1402.045.
4. Results
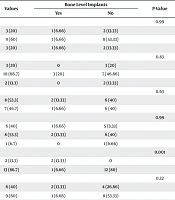
The study included 30 patients, divided into two groups: Fifteen patients received bone level implants, and 15 received tissue level implants. The demographic characteristics of the patients are presented in Tables 1 and 2. Of the participants, 15 were male and 15 were female. Additionally, 43.3% of the patients were former smokers, and only 6.7% were current smokers.
For the bone level implant group, the majority of patients were aged 51 - 60 years (60%). In terms of compliance with oral hygiene, 66.7% had an average status. Educationally, 53.3% had less than a diploma. Regarding health status, 86.7% did not have diabetes, 60% were not former smokers, and 93.3% were not current smokers (Table 1).
| Variables | Values | Bone Level Implants | P-Value | |
|---|---|---|---|---|
| Yes | No | |||
| Age | 0.99 | |||
| 40 - 50 | 3 (20) | 1 (6.66) | 2 (13.33) | |
| 51 - 60 | 9 (60) | 1 (6.66) | 8 (53.33) | |
| > 60 | 3 (20) | 1 (6.66) | 2 (13.33) | |
| Compliance with oral hygiene | 0.83 | |||
| Weak | 3 (20) | 0 | 3 (20) | |
| Average | 10 (66.7) | 3 (20) | 7 (46.66) | |
| Great | 2 (13.3) | 0 | 2 (13.33) | |
| Gender | 0.63 | |||
| Male | 8 (53.3) | 2 (13.33) | 6 (40) | |
| Female | 7 (46.7) | 1 (6.66) | 6 (40) | |
| Education | 0.99 | |||
| Illiterate | 6 (40) | 1 (6.66) | 5 (3.33) | |
| Less than a diploma | 8 (53.3) | 2 (13.33) | 6 (40) | |
| Diploma and above | 1 (6.7) | 0 | 1 (6.66) | |
| Diabetes mellitus type 2 | 0.001 | |||
| Yes | 2 (13.3) | 2 (13.33) | 0 | |
| No | 13 (86.7) | 1 (6.66) | 12 (80) | |
| Former smoker | 0.32 | |||
| Yes | 6 (40) | 2 (13.33) | 4 (26.66) | |
| No | 9 (60) | 1 (6.66) | 8 (53.33) | |
| Current smoker | 0.04 | |||
| Yes | 1 (6.7) | 1 (6.66) | 0 | |
| No | 14 (93.3) | 2 (13.33) | 12 (80) | |
a Values are expressed as No. (%).
| Variables | Values | Tissue Level Implants | P-Value | |
|---|---|---|---|---|
| Yes | No | |||
| Age | 0.99 | |||
| 40 - 50 | 4 (26.7) | 1 (6.66) | 3 (20) | |
| 51 - 60 | 7 (46.7) | 3 (20) | 4 (26.66) | |
| > 60 | 4 (26.7) | 1 (6.66) | 3 (20) | |
| Compliance with oral hygiene | 0.7 | |||
| Weak | 11 (73.3) | 4 (26.66) | 7 (46.66) | |
| Average | 4 (26.7) | 1 (6.66) | 3 (20) | |
| Great | 0 (0) | 0 | 0 | |
| Gender | 0.001 | |||
| Male | 7 (46.7) | 5 (3.33) | 2 (13.33) | |
| Female | 8 (53.3) | 0 | 8 (53.33) | |
| Education | 0.04 | |||
| Illiterate | 5 (33.3) | 0 | 5 (3.33) | |
| Less than a diploma | 7 (46.7) | 3 | 4 (26.66) | |
| Diploma and above | 3 (20) | 2 (13.33) | 1 (6.66) | |
| Diabetes mellitus type 2 | 0.99 | |||
| Yes | 3 (20) | 1 (6.66) | 2 (13.33) | |
| No | 12 (80) | 4 (26.66) | 8 (53.33) | |
| Former smoker | 0.001 | |||
| Yes | 7 (46.7) | 5 (3.33) | 2 (13.33) | |
| No | 8 (53.3) | 0 | 8 (53.33) | |
| Current smoker | 0.16 | |||
| Yes | 1 (6.7) | 1 (6.66) | 0 | |
| No | 14 (93.3) | 4 (26.66) | 10 (66.66) | |
a Values are expressed as No. (%).
The detection rate of infection in the bone level implants group was 20%, while in the tissue level implants group, it was 33.3%. The overall infection rate across both groups was 26.7%. Additionally, no significant difference was observed between the number of microorganisms and the methods used in implant placement (P = 0.42) (Table 3).
| Variables | Yes | No | P-Value |
|---|---|---|---|
| Bone level implants | 3 (20) | 12 (80) | 0.42 |
| Tissue level implants | 5 (33.3) | 10 (66.7) | |
| Total | 8 (26.7) | 22 (73.3) |
a Values are expressed as No. (%).
5. Discussion
In this study, the overall prevalence of infection after implant placement was 26.7%. In contrast, a study by Camps-Font et al. in Spain, using a retrospective cohort method, reported a prevalence of 2.8%, with 65% of implants removed due to infection (31). Tabrizi et al. in Iran, using a cross-sectional cohort method, found that 3.46% of 980 patients with implant placement were diagnosed with infection, and 70.6% of these cases resulted in failure (32). Similarly, Sagnori et al. in Brazil, in a retrospective study conducted 21 years ago, reported that out of 4886 patients, 164 were diagnosed with infection (33).
In this study, the prevalence of infection after implant placement was higher in men than in women. Figueiredo et al. in Spain, examining 88 patients in case and control groups, also found a higher prevalence of infection in men (34). Thiebot et al. identified risk factors such as bone type density and smoking (35), while Kumari et al. reported that pain, mobility, and suppuration were more prevalent in men (36), consistent with our findings. Conversely, another study found no relationship between diabetes, age, gender, high blood pressure, and long-term drug use with implant failure (35). Differences in demographic characteristics may contribute to these variations.
Periodontitis increases systemic inflammatory response, playing a role in stroke development (37). Effective patient management is crucial in implant placement, especially for those with systemic and neurological conditions, including stroke. Findler et al. found no evidence of infective endocarditis (IE) during follow-up in patients with implant placement, although one patient developed mitral valve thrombosis and another experienced a stroke six months post-implantation (38). Elter et al. reported stroke/TIA incidences of 15.6% in dentate non-examinees, 13.5% in periodontal examinees, and 22.5% in edentulous individuals (37). Although hemorrhagic stroke is not infectious, other studies link stroke and periodontitis. Increased inflammation in stroke patients can cause acute cerebral ischemic episodes, highlighting the need for preventive measures to mitigate inflammatory responses and disease exacerbation (20, 39-41).
A strength of this study is its focus on implant placement in stroke patients, a topic with limited research in neurological contexts. These findings provide valuable insights for researchers. However, a limitation is the small sample size, suggesting that future studies should include larger patient cohorts.
5.1. Conclusions
The accumulation of microorganisms was higher in tissue level implants compared to bone level implants, underscoring the need for preventive and management measures. It is essential for dentists to provide patients with the necessary training and care to prevent infection.