1. Background
Nurses play an important role in the assessment of elderly people with Alzheimer's disease (AD) and their caregivers. Due to the wide range of nursing roles, they can provide satisfactory and optimal management for people with AD and their family caregivers (1). A review of Asian research found four factors, in addition to others identified: Caregiver strain, stigma, family stress, and positive aspects. Although the 2017 WHO global action plan for dementia includes recommendations, there is a gap between these recommendations and actual research (2). The number of dementia caregivers has increased due to the changing needs of these patients over a long period of time, and their continued support is a significant challenge for all healthcare systems around the world (3). Limited interventions to support family caregivers of people with dementia have been implemented in different communities, taking into account culture, while it is important to address the unique needs of family caregivers on an individual basis (4).
Dementia is defined as a clinical syndrome and includes various brain disorders in which brain function is impaired. Dementia is often severe and progressive and affects a person's memory, thinking, behavior, and emotions (5-7). The clinical symptoms of AD include a decline in cognitive functions, impairment of normal daily activities, and changes in a person's behavioral actions (8, 9). Considering the increase in the percentage of elderly people compared to the whole population in society, the significance of AD becomes clearer (10). Alzheimer's disease is more common in older adults, but young people may also be affected by this disease (11, 12).
Although there is no specific and complete treatment for AD, drug and non-drug treatments are used to control it (13-15). Several drugs are available for AD patients in the early stages. Although these drugs do not cure AD, they can temporarily slow symptom progression in some cases (8, 9, 16). While caring for AD patients, the family is the most important source of help, and it is very important that all family members assist in caring for the patients. However, sometimes families do not help the patient due to a lack of understanding and awareness of the disease, causing discomfort for the patient. In such cases, contacting the family, providing care to the patient, and giving nursing counseling can be very helpful (13-15).
Palliative and supportive care are important in chronic patients (17-19). Family-centered care is a care philosophy. The family unit plays an important role as the main focus in all health care, especially in diseases that require patient care at home (20). In the family, health care is provided by the main caregivers of the patient (21). Nurses also interact with family members to care for the patient, and their duty is to increase awareness, skill, and provide support to family caregivers in order to ensure the provision of high-quality care at home. The goal of family-centered care is to improve the patient's ability to perform health-related activities independently (22-24).
According to Bandura's social learning theory, self-efficacy means an individual's ability to cope with challenging and stressful situations or to evaluate the individual's capacity to perform an activity or task in order to achieve a specific goal (24-27). In other words, self-efficacy refers to people's beliefs about their abilities in performing a task and mobilizing motivations, cognitive resources, and exercising control over a certain event (28, 29).
2. Objectives
Although there has been much research on caregivers' problems and the lack of support for them, there has been no study on the effect of nursing counseling on the self-efficacy of family caregivers of AD patients. Therefore, the present study was designed and implemented.
3. Methods
The study population of the present interventional study included 42 family caregivers of elderly people with AD in Khorramabad city in 2022 (ethics code: IR.MEDILAM.REC.1400.226). Inclusion criteria for caregivers included having a family relationship with the elderly, living with the patient for at least the past six months, having physical and mental health [scores less than 28 using the General Health Questionnaire (GHQ-28), a self-efficacy score less than 30 (using the Self-efficacy Questionnaire)], a confirmed diagnosis of AD by a specialist, earning a score of 6 or less in the abbreviated mental test score (AMTS), and age over 60 years. Exclusion criteria also included the sudden death of the AD patient during the study, separation of the caregiver from the patient during the study, non-participation in training sessions, and suffering from other debilitating diseases.
The data collection tools included a demographic information form, the General Self-efficacy Scale (GSE-10), the AMTS, and the GHQ-28. The demographic information form included questions on age, gender, marital status, level of education, occupation, and duration of patient care by the research samples. The GSE-10 consists of 10 items that all evaluate the level of general self-efficacy. Scores of 10 - 20, 21 - 30, and scores above 30 are considered as low, moderate, and high self-efficacy, respectively. The possible score range is 10 to 40. The AMTS consists of 10 questions from the 37-question Roth-Hopkins test, and the total score is obtained from the sum of the scores of all 10 questions. The possible score range is 0 - 10, and the lower the total score, the more severe the cognitive disorders will be (30). The GHQ-28 consists of 28 items and 4 subscales, which are scored based on a four-choice Likert scale. Each question is scored from 0 to 3 (A, B, C, and D are assigned 0, 1, 2, and 3, respectively) (31).
In order to determine the sample size in the present study, the study by Salamizadeh et al. on the mean score and deviation of the Self-efficacy Scale after the intervention was used (29, 32), and the sample size was calculated using the following formula:
n1 = K × 19 = 1 × 19 = 19
μ1 = 32.73; μ2 = 27.85; δ1 = 4.75; δ2 = 5.98; K = 1; α = 0.05; β = 0.2
The sample size was 19 people in each group. Considering that the number of people in the intervention and control groups is the same, a total of at least 38 people was required to participate in the study, which increased to 42 people (21 people in each group) by considering a 10% probability of sample attrition.
Participants were selected using convenience sampling from eligible caregivers of elderly people referred to health care centers or those whose information was registered in the Sib system, as well as the Alzheimer's Association of Iran, which is active in Khorramabad city. The study objectives were explained to them, and after obtaining their informed consent, they were randomly assigned to one of the experimental or control groups using random allocation. Moreover, after calculating the sample size, the researcher randomly assigned a group of them to group A and the rest to group B. In this study, considering a sample size of 42 people, 21 balls for each intervention group (A and B) were placed in a container. The balls were then randomly removed from the container without replacement, and the sequence was recorded. Both groups were assured that they would be informed about the results of the study.
Nursing counseling was used for the experimental group to increase self-care self-efficacy (26). Nursing consultation was individual and was conducted verbally, in person, or by telephone according to the caregiver's request or preference. The location, time, number of sessions, and content of consultations were adjusted according to the caregivers' needs. While such nursing counselling was not performed for the control group, and they only received the routine care of and the relevant educational materials were provided to the control group at the end of the study. The first nursing counselling session was dedicated to the self-efficacy of the family caregiver of a patient with AD. The researcher assessed the self-efficacy of caregivers by using guide questions (10 questions), which were designed based on the GSE (Schwarzer & Jerusalem, 1981). Then, he provided counselling to the caregiver, if needed.
Data analysis was carried out using descriptive and analytical statistical methods. In order to describe qualitative variables, percentage and frequency were used, and mean ± SD was used for quantitative variables. Also, paired t-tests and independent t-tests were used in SPSS version 16. The P-value was considered to be 0.05.
4. Results
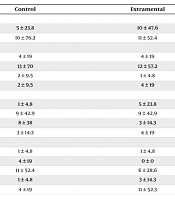
The mean ± SD of the participants' age in the experimental group was 45.71 ± 10.50 and in the control group was 44.86 ± 12.90 years, respectively. Table 1 shows the frequency and percentage of the variables of gender, marital status, education, and employment status in the two experimental and control groups.
| Variables | Control | Extramental |
|---|---|---|
| Gender | ||
| Man | 5 ± 23.8 | 10 ± 47.6 |
| Female | 16 ± 76.2 | 11 ± 52.4 |
| Marital status | ||
| Single | 4 ± 19 | 4 ± 19 |
| Married | 13 ± 70 | 12 ± 57.2 |
| The widow | 2 ± 9.5 | 1 ± 4.8 |
| Divorced | 2 ± 9.5 | 4 ± 19 |
| Education | ||
| Illiterate | 1 ± 4.8 | 5 ± 23.8 |
| High school | 9 ± 42.9 | 9 ± 42.9 |
| Diploma | 8 ± 38 | 3 ± 14.3 |
| University | 3 ± 14.3 | 4 ± 19 |
| Job | ||
| Retired | 1 ± 4.8 | 1 ± 4.8 |
| Unemployed | 4 ± 19 | 0 ± 0 |
| Housewife | 11 ± 52.4 | 6 ± 28.6 |
| Employee | 1 ± 4.8 | 3 ± 14.3 |
| Free | 4 ± 19 | 11 ± 52.3 |
a Values are expressed as mean ± SD.
The mean ± SD self-efficacy score of the experimental group increased significantly from 18.19 ± 5.11 before the intervention to 29.04 ± 5.80 after the intervention (P = 0.001). However, the control group showed no significant change in mean ± SD scores, moving from 18.19 ± 6.05 to 18.52 ± 6.15 (P = 1.00). This result highlights the effectiveness of nursing counseling in improving self-efficacy among caregivers of AD patients (Table 2).
| Variables | Mean ± SD | Min | Max | P-Value |
|---|---|---|---|---|
| Extramental | 0.001 | |||
| Before intervention | 18.19 ± 5.11 | 11 | 29 | |
| After intervention | 29.04 ± 5.80 | 17 | 39 | |
| Control | 1 | |||
| Before intervention | 18.19 ± 6.05 | 9 | 35 | |
| After intervention | 18.52 ± 6.15 | 9 | 34 |
5. Discussion
Any stressor can lead to an increase in mental disorders in old age, and the patient's family experiences a lot of care pressure (33). The results of the present research showed that the mean ± SD of the pre-intervention self-efficacy scores of the experimental and control groups were 18.19 ± 5.11 and 18.19 ± 6.52, respectively, which shows that the participants of both groups had low self-efficacy. The results of a study by Bastani et al. (34) also showed that the mean ± SD of the self-efficacy scores of caregivers of AD patients was 28.24 ± 6.34; in other words, a majority of participants (65%) had poor self-efficacy. Karami et al. (35) reported that the mean ± SD of the GSE score in caregivers of patients with bipolar disorder was 41.99 ± 7.64 (36). It should be noted that a single instrument was used to measure self-efficacy in studies by Bastani et al., Karami et al. (34, 35), and the present study, but the self-efficacy score was divided differently in the study by Bastani et al. (34) as compared to the present study and Karami et al.'s study (35). That is, self-efficacy scores were divided into non-optimal (score 30 and below) and optimal levels (score 30 and above) in Bastani et al.'s study, and the results of these studies are consistent with the present study, which indicates low self-efficacy scores in family caregivers of Alzheimer's patients in Iran (34).
The mean ± SD self-efficacy score of the experimental group increased significantly from 18.19 ± 5.11 before the intervention to 29.04 ± 5.80 after the intervention (P = 0.001). However, the control group showed no significant change in mean ± SD scores, moving from 18.19 ± 6.05 to 18.52 ± 6.15 (P = 1.00). This result highlights the effectiveness of nursing counseling in improving self-efficacy among caregivers of AD patients. In Gitlin et al.'s study, a difference was found between the two groups after the training program in the mean self-efficacy scores of caregivers of patients with dementia (P = 0.03) (36). In the study of Salamizadeh et al., after the test, the two scores in the test and control groups were reported as 32.73 ± 4.75 and 27.85 ± 5.98, respectively (32). Also, in Easom et al.'s study, which was conducted on the self-efficacy of two Hispanic and non-Hispanic Caucasian groups using an educational test and the RSCSE tool to measure self-efficacy, a difference was found between the self-efficacy scores of the two groups after the test (P < 0.001) (37).
A study used conversational artificial intelligence (AI) to provide dementia care advice based on the dementia care guide in 30 Days. The PDC30 chatbot’s responses to 21 common questions were compared with ChatGPT responses and another chatbot (called Chatbot-B) as reference standards. Twenty-one family caregivers used the PDC30 chatbot for two weeks and rated and commented on its acceptability. Results showed that the PDC30 chatbot was user-friendly, and users described its responses as helpful and relatively satisfactory (4). Although the performance of AI and chatbots was not compared to that of a nurse and nursing advice, this study also highlights the importance of advice for family caregivers of patients with AD.
5.1. Conclusions
Given the effectiveness of nursing counseling on the self-efficacy of family caregivers of elderly people with Alzheimer's, nursing counseling can be used in centers providing services to elderly caregivers. Nursing counseling can also be used for family caregivers of other patients with cognitive disorders and can help improve the quality of care and increase the self-efficacy of caregivers.