1. Introduction
Cerebral aspergillosis is an opportunistic infection primarily caused by the fungus Aspergillus fumigatus. This rare disease typically affects individuals who are immunocompromised and those with debilitating conditions such as alcoholism, diabetes mellitus, multi-organ failure, drug addiction, and certain types of hematological malignancies (1). Aspergillus is the most prevalent etiologic agent of fungal sinusitis. In noninvasive forms, it may present as chronic sinusitis characterized by mucosal destruction and expansion of the sinus cavity , without evidence of bony invasion (2). It affects 10% - 15% of patients who have disseminated aspergillosis (3). The distinctive ability of Aspergillus to break down elastin in the vessel wall makes it highly angioinvasive, resulting in a broad range of neurological complications (4, 5). Fever is a common symptom of pulmonary aspergillosis, but it is rare in cases of cerebral invasion. Magnetic resonance imaging (MRI) is a sensitive tool for detecting strokes early. While the classic imaging finding is ring-enhancing lesions, other patterns may also occur (6). Cerebral localization is observed in only 5% of patients, and a definitive diagnosis in such cases requires a biopsy (7). We present a case of cerebral angioinvasive aspergillosis in a patient with poorly controlled diabetes mellitus, who exhibited clinical and radiological signs consistent with an acute cerebral infarction.
2. Case Presentation
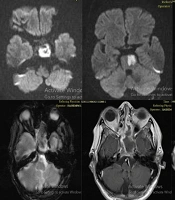
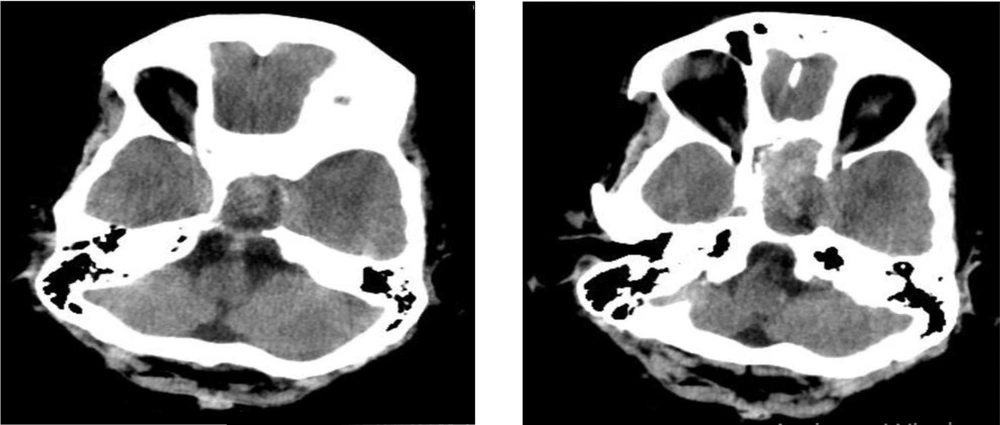
A 57-year-old Iranian female with a history of poorly controlled hypertension and diabetes mellitus was referred to the Neurology Emergency Department at Qaem Hospital in February 2023. She was taking metformin, losartan, and gliclazide. The patient presented with right-sided hemiparesis and right facial paresis upon awakening. On initial neurological examination, the patient exhibited a flattened fold in the right nasolabial area, consistent with central facial paresis. Muscle strength was assessed as 2/5 in the right upper limb and 1/5 in the right lower limb, with normal strength on the left side. A Babinski sign was noted on the right foot, though no lingual deviation was observed. Cranial nerve function was intact, and eye movements were regular, with no evidence of Marcus-Gunn pupil, proptosis, or ptosis. The ENT examination revealed no mucosal lesions, necrosis, plaques, or deviations of the tongue or uvula, and palate sensation was normal. Due to the delayed presentation — approximately 16 hours after symptom onset — the patient was not eligible for thrombolysis or thrombectomy. A brain computed tomography (CT) scan was performed, which revealed small vessel disease but no acute infarction. However, midline hyperdensity extending into the paranasal sinuses (PNS), along with deviation of the sphenoid bone, was noted (Figure 1). The patient was started on initial anti-ischemic treatment, including a loading dose of clopidogrel 300 mg followed by 75 mg daily, along with a loading dose of aspirin 325 mg, then 80 mg daily. Additionally, atorvastatin 40 mg daily was administered, and the patient was further evaluated for an acute stroke. Following the CT scan findings, a contrast brain MRI was performed. The MRI revealed a mass-like lesion extending into the bilateral sphenoidal sinuses (Figure 2). Differential diagnoses included ring-enhancing necrotic tumors and abscess formation.
The magnetic resonance imaging (MRI) study, including diffusion-weighted imaging (DWI), fluid-attenuated inversion recovery (FLAIR), T2-weighted, gradient-recalled echo (GRE), and post-contrast T1-weighted sequences, reveals an acute brainstem infarction. Additionally, a mass-like lesion extending into the bilateral sphenoid sinuses is observed, further supporting the underlying pathology.
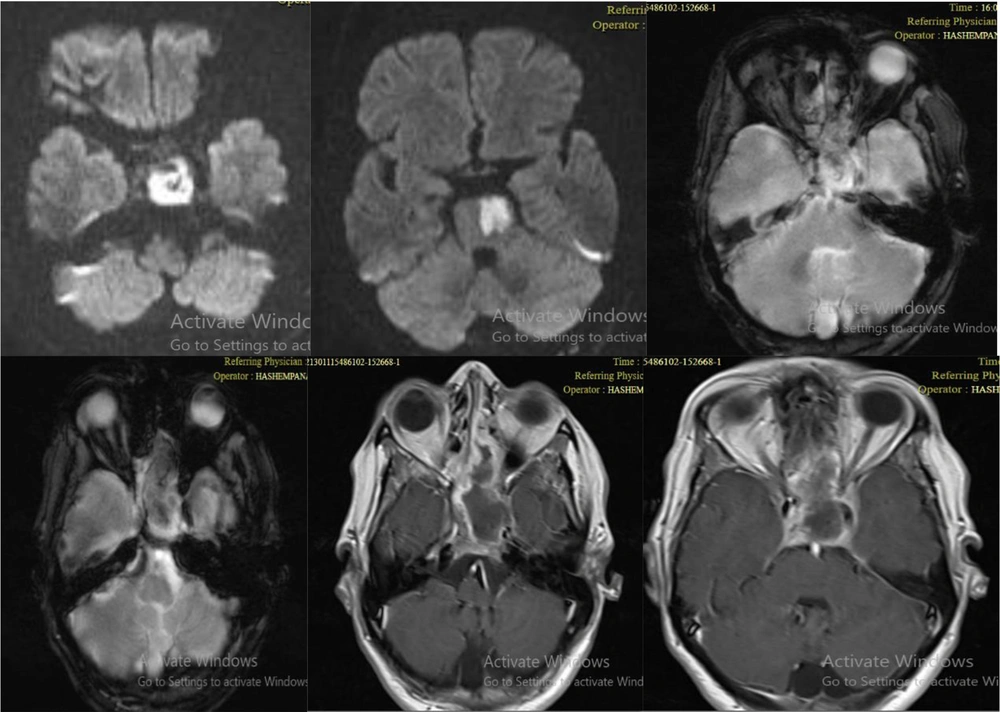
Additionally, an acute ischemic infarction was observed on the right side of the pons, where the vertebral artery is near the sphenoidal sinus on the left and posterior sides. To further investigate the PNS lesions and sphenoidal bone destruction, a PNS CT scan was conducted. The PNS scan revealed opacity in the bilateral sphenoidal and ethmoidal sinuses, with dilation and exposed walls in the left sphenoidal sinus (Figure 3).
The patient's medical history also included long-standing post-nasopharyngeal drainage (PND), which had worsened over the past 2 - 3 months. She reported occasional epistaxis and had experienced left retro-orbital pain in the last three months, although she had not sought specific treatment during outpatient visits. She also mentioned a transient episode of diplopia the day before her visit, which had since resolved. Over the preceding months, she had not experienced fever, headache, rhinorrhea, epiphora, hyposmia, anosmia, facial swelling, facial paresthesia, blurred vision, hearing loss, balance disturbances, swallowing difficulties, numbness in the palate or cheeks, dysphonia, or respiratory, gastrointestinal, skin, or musculoskeletal symptoms. There was no history of colds or infections. Given the MRI and PNS CT scan findings, along with the patient's history of diabetes mellitus, consultations with ENT, neurosurgery, and infectious disease specialists were initiated. The possibility of an invasive fungal infection in the PNS, such as mucormycosis, was considered, and empirical treatment with Amphotericin B (350 mg/day) and Piperacillin-Tazobactam (4.5 g every 8 hours) was started. The neurosurgical consultation confirmed that there was invasion of brain tissue. The lesion was confined to the PNS, particularly the sphenoid sinus, with extension into the cavernous sinus, but without evidence of dural involvement. Continued management by the ENT service was recommended.
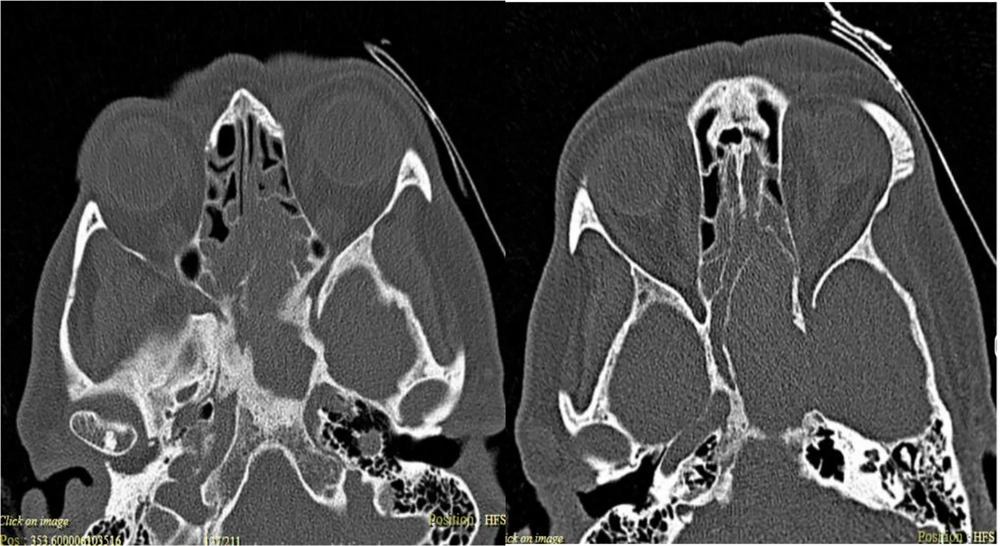
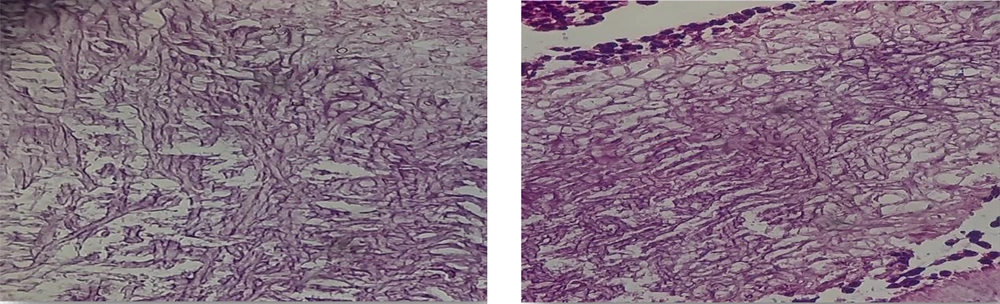
The patient was subsequently transferred to the ENT operating room for biopsy and endoscopic examination of the nasal and PNS. Under general anesthesia, the left sphenoid sinus was opened, and fungal secretions were suctioned. Degradation of the superior wall of the sphenoid sinus was noted, exposing the dura, brain, and carotid artery, and as much of the fungal material as possible was removed. The right sphenoid sinus was also opened and found to be connected to the opposite side. A nasal mesh was inserted, and the patient was transferred to the recovery area. Following endoscopic removal of the fungal mass, histopathological examination identified septate hyphae with acute-angle branching, indicative of Aspergillus species. The periodic acid-Schiff (PAS) stain enhanced the visibility of the hyphal structures, distinguishing them clearly from the surrounding tissue (Figure 4). After five days of Amphotericin B treatment, the patient's regimen was switched to voriconazole, following the identification of the specific fungal species. Voriconazole was administered for 10 days, starting with a loading dose of 6 mg/kg every 12 hours for one day, followed by 4 mg/kg every 12 hours.
Simultaneously, the cause of the pons infarction was investigated, and anti-ischemic treatment was initiated on the first day of hospitalization. Cardiac consultations were conducted to evaluate potential heart disease, and echocardiography and endocrine tests were performed to manage the patient's blood sugar and metabolic risk factors. A CT angiography was also conducted to assess the neck vessels. The echocardiography results were as expected, and the CT angiography revealed no intracranial or extracranial stenosis that could explain atherosclerosis. All laboratory tests were standard, except for an elevated erythrocyte sedimentation rate (ESR), which was initially 81 but decreased to 60 after sinus drainage. Upon discharge, the ESR had further declined to 42. Five days after starting voriconazole, the patient underwent a repeat sinus endoscopy, which showed no fungal tissue. A follow-up biopsy also yielded a negative result.
Following partial recovery and the negative biopsy result, the patient was discharged on an oral regimen of voriconazole, 300 mg every 12 hours, with instructions for outpatient follow-up. Despite extensive evaluation during the stroke work-up, no definitive cause for the infarction was identified in the cardiac assessment or imaging of the brain and neck vessels. Based on imaging, the infarction was likely caused by the proximity of the fungal infection in the sphenoid sinus to the vertebral artery, leading to inflammatory damage to the arterial wall and resulting in infarction in the territory of the artery. The patient had experienced transient diplopia before to referral. Since the high-resolution CT (HRCT) scan of the lungs was routine, the fungal dissemination was likely to have originated from the PNS. This is an unusual presentation, as cerebral invasive aspergillosis typically spreads hematogenously from the lungs or gastrointestinal tract, rather than directly extending from sinus disease. The reporting of this study conforms to CARE guidelines (8). Written informed consent was obtained from the patient for the publication of this case report and any accompanying images.
3. Discussion
Aspergillus is a common soil fungus whose spores are often inhaled without harm in healthy individuals. However, in immunocompromised individuals, it can cause respiratory infections, most notably pulmonary aspergillosis, which includes forms such as aspergilloma, allergic bronchopulmonary aspergillosis, and invasive pulmonary aspergillosis. In severe cases, particularly in those with hematologic malignancies or those undergoing immunosuppressive therapy, the infection may spread to other organs, including the central nervous system (9-11). CNS aspergillosis is a rare but serious infection, primarily affecting immunocompromised patients, particularly those undergoing treatment for hematologic malignancies, stem cell, or solid organ transplantation (12, 13). In our case, the patient experienced transient diplopia before to referral, and a normal lung HRCT, suggesting an uncommon direct extension from the PNS, as opposed to the typical hematogenous spread from the lungs or gastrointestinal tract. Neuro-aspergillosis may present as persistent meningitis, encephalitis, brain abscess, or mycotic aneurysm rupture, and can mimic other CNS infections. Its unique vasculopathic nature may result in acute infarction or hemorrhage (14). In some cases, hyphal invasion may fully occlude vessels, resulting in ischemic stroke. In our case, imaging suggested that the infarct was due to inflammation of the vertebral artery, likely caused by the proximity of the fungal infection to the sphenoid sinus. Cerebral aspergillosis has a poor prognosis, with a mortality rate of 10 - 20% in immunocompetent patients and up to 90 - 100% in immunocompromised individuals. Antifungal therapy should be continued until all symptoms resolve or residual scarring is observed on imaging, which may require up to 12 weeks (15). In a case series by Little et al. involving 78 patients with invasive fungal carotiditis, Aspergillus species were identified in 41 cases. The most frequent initial symptoms included headache, visual disturbances, and cranial nerve palsies. Vascular complications observed were arterial occlusion, aneurysm formation, and vessel rupture, with cerebral infarctions occurring in 50% of patients. The study reported a high mortality rate, with 71% of patients dying within two years (3).
According to a recent meta-analysis published in 2024, early diagnosis and treatment of fungal infections, as well as endovascular surgery, are key factors for a better prognosis. Amphotericin B was previously the treatment of choice; however, due to its severe adverse effects, particularly in renal transplant patients, voriconazole has proven to be a better alternative for angioinvasive aspergillosis, especially in transplant recipients. Surgical excision or drainage, as performed in our case, serves as an essential adjunct to antifungal therapy. It can help reduce the fungal load, improve antifungal penetration, relieve mass effect, and decrease the local neurotoxic and inflammatory effects of the infection. Neurosurgical debridement combined with antifungal therapy has been shown in some studies to provide better survival rates compared to pharmacologic treatment alone (13, 15-17). Our patient underwent 24-hour cardiac Holter monitoring to assess heart rhythm and blood pressure, as well as trans-thoracic echocardiography, all of which were normal. Additionally, a CT angiography of the neck and intracranial vessels was performed, revealing no obstruction or significant narrowing of the lumen. Given the location of the infarction, the recent lesion, and the presence of multiple micro-infarctions, the most likely diagnosis is a stroke induced by aspergillosis. The patient benefited from a combination of antifungal therapy and surgical intervention, which reduced the fungal burden, enhanced the efficacy of the drugs, and alleviated the mass effect. This multidisciplinary approach, supported by evidence in the literature, highlights that a combined strategy involving antifungal treatment and surgical debridement yields better survival rates compared to pharmacological treatment alone.
3.1. Conclusions
Cerebral invasive aspergillosis is a rare yet life-threatening condition that primarily affects immunocompromised individuals. In this case, the patient's stroke-like symptoms led to a diagnosis of aspergillosis, confirmed through imaging, endoscopic biopsy, and clinical findings. Early diagnosis, combined with antifungal therapy and surgical debridement, was instrumental in improving the patient's outcome. This case underscores the importance of maintaining a high index of suspicion, particularly in immunocompromised patients, to facilitate prompt diagnosis and intervention. The successful outcome demonstrates the value of an integrated treatment approach, which combines antifungal therapy with surgical debridement to reduce the fungal load and enhance drug efficacy. Literature supports this multidisciplinary strategy as it is associated with better survival rates compared to pharmacologic treatment alone. This case underscores the need for vigilance, early intervention, and a comprehensive approach to managing cerebral aspergillosis, which can improve prognosis and lower the high mortality risk associated with this infection.