1. Introduction
Localization of brain lesions and prevention of damage to vital structures are important in operation of brain pathologies. Despite development of many techniques a more accurate localizing technique is still needed. A step forward to achieve this goal is to develop a navigation system (1). This system may have some disadvantages such a time consuming, calculation and registration, need for brain shift compensation after dura opening (2), restriction of space and view inside the operating field, increased risk of wound infection and cost. Nevertheless there are many advantages that can be helpful in the process of operation (3). An error in the white matter by the navigation device even in the range of 3 mm or 4 mm is still lower than when the procedure only relies on neurosurgical knowledge. The neurosurgeon is able to calculate the localization and approach a small lesion accurately, therefore he would feel more confident (4). Additionally, it reduces the risk for neurological morbidity by allowing the surgeon to determine the relationships of the lesion and surgical approach to nearby critical brain structures. In modern neurosurgery the main clinical utilities are: localization of small intracranial lesions, skull-base surgery, intra cerebral biopsies, intracranial endoscopy, functional neurosurgery and spinal navigation (5). Safe navigation of the critical anatomy is a priority in skull base surgeries. This is particularly the case for endoscopic skull base surgery where the surgeons work within millimeters of neurovascular structures. Navigation can help accurate localization of important anatomic structures such as the carotid artery or cranial nerves, particularly if they are deep in the tumor (6). Navigation can also be successfully used in epilepsy surgery for localization and introduction of subdural strip and grid electrodes or for implanting deep-brain electrodes in the hippocampus. Equally interesting is the navigated operation during ablative surgery in cases of epilepsy, such as with hippocampectomy, to more accurately localize the resection size (7). There are reports of neuronavigation use for cerebral aneurysmal surgery but they are scarce. Here we present a case with cerebral aneurysm that was operated with the guide of navigation system. We also review related papers that have been published in the literature.
2. Case Presentation
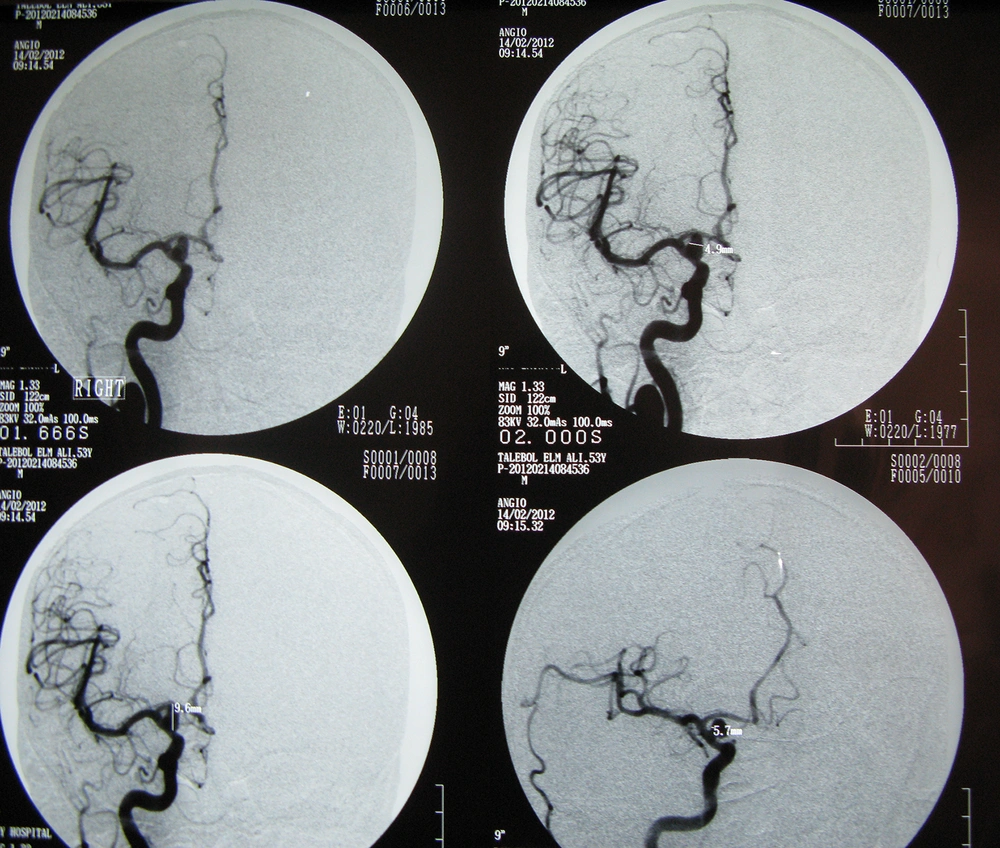
A 53-year-old man developed a sudden severe headache two days before admission. He did not have any specific medical problems, such as hypertension, diabetes mellitus, hypercholesterolemia, infectious disease, head trauma, or heart disease. On inspection of neurological status, he was alert and his motor power was normal in all extremities. CT scan on admission showed diffuse blood in sylvian fissures and basal cisterns. CT angiography and magnetic resonance imaging revealed an aneurysm and angiography confirmed an aneurysmal dilatation where the posterior communicating artery arises from the right internal carotid artery (ICA). Its neck diameter was 4.9 mm and its dome looked medially (Figure 1). We planned to operate on the right posterior communicating aneurysm. MRI scan with appropriate protocol for neuronavigation was done and demonstrated, on Gadolinium (Gd) enhanced images, a small round hyperintense lesion in the parasellar region on the right side.
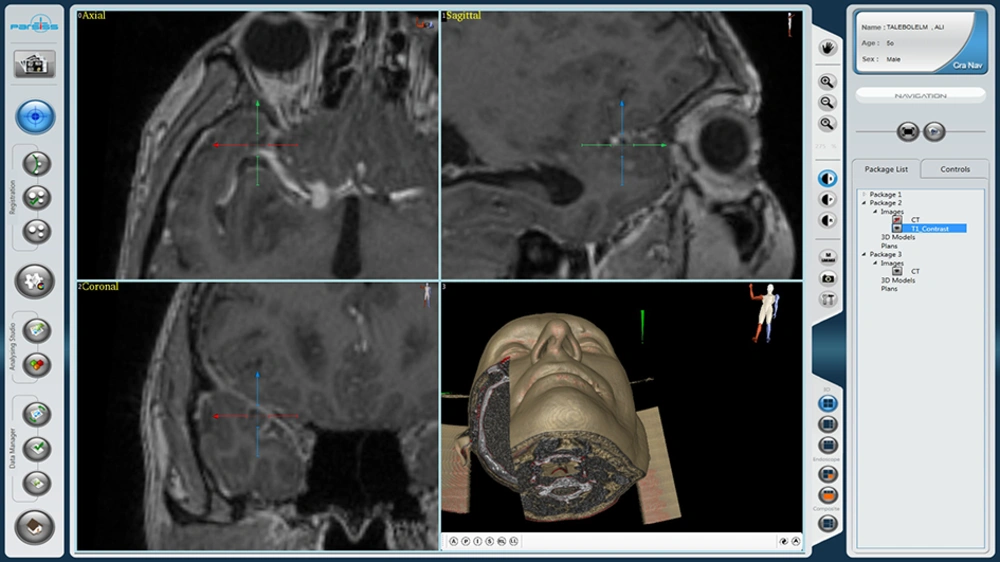
Using Parsiss neuronavigation system (Parseh intelligent surgical system, Tehran, Iran), preoperative MRI stereotactic images were loaded after facial scanning and the source images were translated into an operative plan. These images allowed surgical planning and visualization of the aneurysm during surgery; we prepared the navigation based on CT scan and MRI for surgery of the aneurysm (Figure 2). Right frontotemporal craniotomy was performed, brain retracted and arachnoid membranes were opened under the guidance of navigation-MRI. An aneurysm was found to arise from posterior communicating artery with medial direction. Its neck width was about 5 mm and without temporary clipping of the ICA, the neck was dissected and a 7 mm long Yasargil type clip was applied to the aneurysm. Neurological status of the patient was unchanged postoperatively and control CT scan was unremarkable.
3. Discussion
It is important to localize brain lesions and prevent damage to vital structures during operation of brain pathologies. Many techniques have been developed but a more accurate localizing technique is still needed. Neuronavigation is used for this proposes and its utilities are in: biopsy and resection of tumors, endoscopy, skull base surgery and functional neurosurgery. Reports of its use in aneurysmal surgery are scarce.
Schmid-Elsaesser et al. stated that Navigation-CT angiography is useful when performing surgery on unruptured aneurysms, especially middle cerebral artery (MCA) aneurysms. They reported that the deviation of the neck in navigation-CT angiography was less than 2.6 mm and that, with this instrument, MCA aneurysms were approached via minicraniotomy, avoiding detachment of the temporalis muscle. Also they stated that current navigation systems are not precise enough to allow "blind" aneurysm clipping by placing a real clip on the virtual aneurysm neck (8).
Lee and Bang reported a rare case of an unruptured non-traumatic dissecting aneurysm of the M4 segment of the MCA accompanied by total occlusion of the ipsilateral ICA. They used navigation-CT angiography and treated M4 aneurysm with proximal ligation. With the guidance of this instrument, they could precisely locate the aneurysm without corticotomy, and by approaching through sulci, further cortical injury was avoided (9).
Kim et al. reported on 12 patients with a distal anterior vertebral artery (DACA) aneurysm who were treated with direct clipping guided by the neuronavigation system. There were no technical problems or complications during application of the neuronavigation system. The registration precision ranged from 0.5 - 1.5 mm (mean: 0.88 mm). The neuronavigation system provided real-time presentation of DACAs and assisted in detection of the DACA aneurysms. They believe that DACA aneurysms are good candidates for neuronavigation and additional benefits of a small craniotomy and accurate intraoperative orientation during surgery result in a minimally invasive aneurysm procedure (10).
Carvalho et al. used a frameless stereotactic navigation system for the microsurgical resection of a distal infectious aneurysm. They used MRI scan with appropriate protocol and demonstrated the aneurysm on Fluid attenuated inversion recovery (FLAIR) sequence. They explained that these images increased aneurysm localization accuracy, allowed surgical planning and visualization of the infectious aneurysm during surgery, resulted in a simpler procedure with a smaller craniotomy, reduced the time for dissection and diminished the risk of vascular and parenchymal iatrogenic damage (11).
Kil et al. reported on 32 patients with unruptured intracranial aneurysms. They were treated by direct surgical neck clipping through the neuronavigation-guided keyhole approach. A 4 to 5 cm skin incision and a small 2.5 × 4 cm craniotomy was performed around the sylvian fissure. They stated that navigation-guided keyhole approach is helpful for the management of anterior circulation aneurysms in selected cases. It has the advantages of less operative time, fewer days of hospitalization, and cosmetic results (12).
We applied the neuronavigation system to guide identification of a ruptured right posterior communicating aneurysm. We used Gd enhanced MRI with appropriate protocol and detected the aneurysm in axial and coronal images. The aneurysm could be visualized virtually and we were able to confirm the location of the vascular pathology by this approach. MRI based neuronavigation results in precision of localization of the aneurysm, increases visualization of the lesion, decreases normal parenchymal and vascular injury and is useful for the treatment of cases of distal MCA and distal ACA aneurysms, while it can also be helpful for better localization of the neck of the aneurysm and results in less damage during aneurysm dissection in paraclinoid lesions.