1. Introduction
Cerebral deep venous thrombosis (CDVT) of Galen vein is an uncommon disorder manifested by bilateral thalamic infarcts, which can lead to poor outcomes without proper treatment. CDVT is a vascular disease with many clinical manifestations which makes the diagnosis difficult (1, 2). In this study, a case of Galen vein thrombosis with bi-thalami infarction was presented.
2. Case Presentation
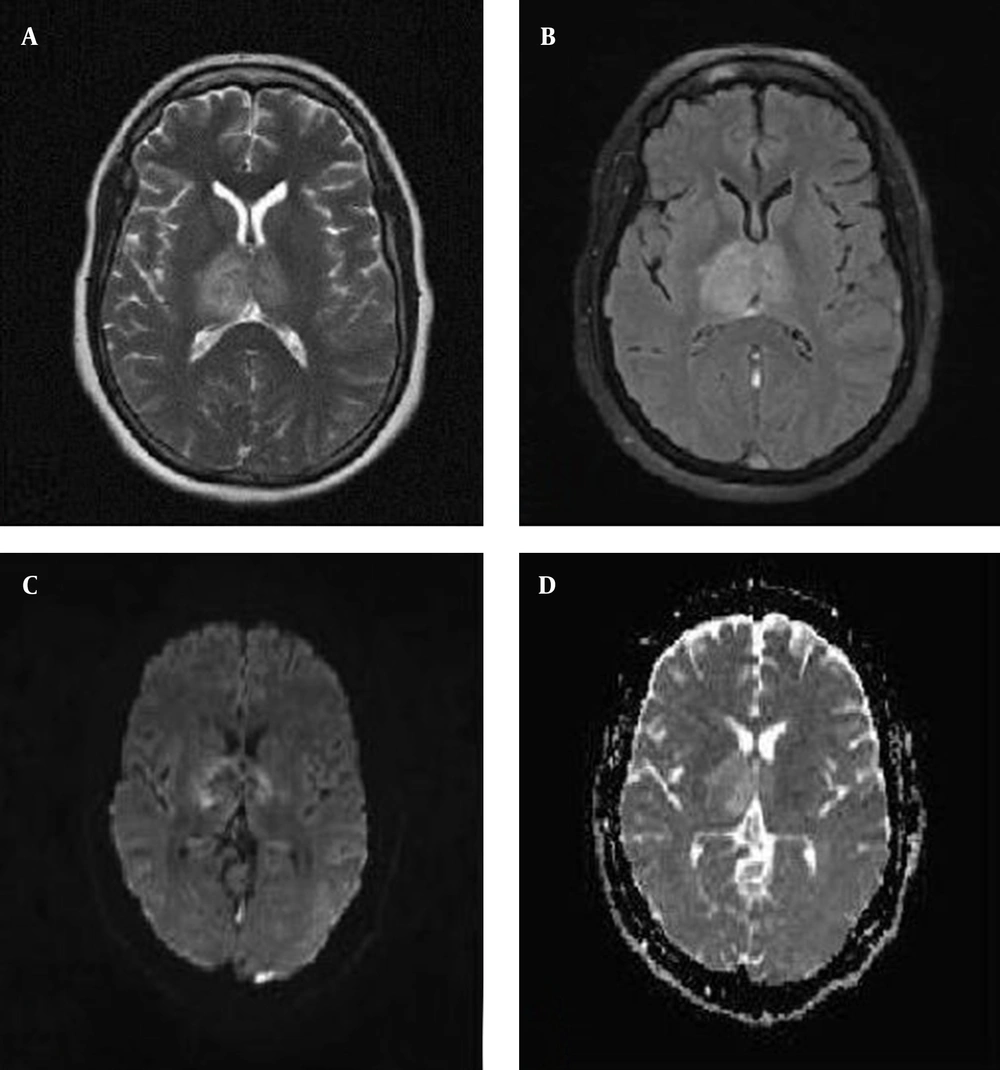
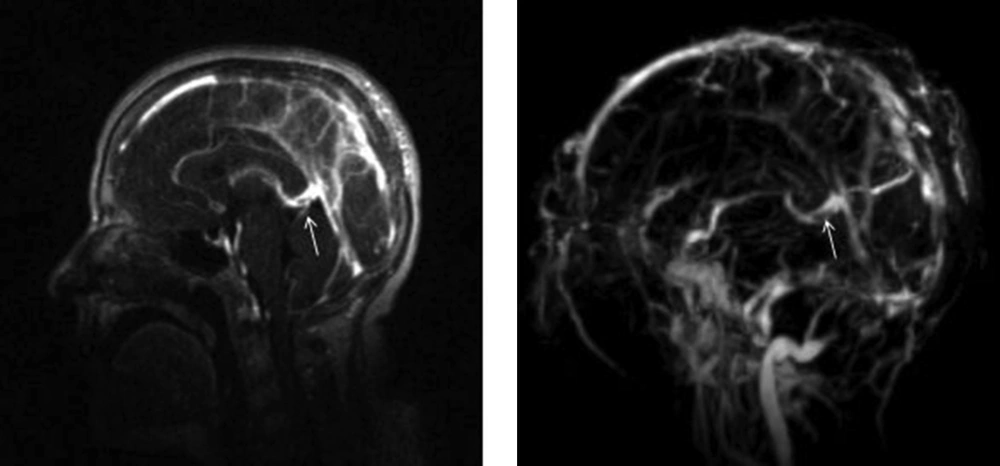
A 37-year-old female was admitted to the emergency department following tonic-colonic seizures occurring twice. She had had headache with acute onset since 11 days before coming to the hospital. Her headache was generalized and continuous all the time. She also had nausea and vomiting. Two days after the onset of her headache, mild weakness of her left limbs occurred. Her seizures occurred nine days later, which repeated twice a day, while she did not have any history of seizures before. Because of her ovarian cyst, she was consuming oral contraceptive pill (OCP) since 2-3 months before. She was confused and drowsy at the admission time. She did not have fever and neck rigidity. She had a mild left facial paresis, but examination results of other cranial nerves were normal. The tone and force of left limbs had decreased and it was 4 upon 5. Plantar reflex in the left side was up, but in the right side it was down. At first, she was admitted in the neurosurgery department with the diagnosis of diencephalon tumor because of her imaging result as well as the streotactic biopsy of the lesion. However, the diagnosis of CDVT was finally confirmed by reviewing the imaging results (Figures 1 and 2).
After that, treatments with anticoagulant (heparin) and then warfarin were performed. In addition, she was treated by an anticonvulsive drug (phenytoin). She had a good recovery through this treatment; her headache and neurological deficits were eliminated and she became quite oriented.
3. Discussion
CDVT is a rare variety of cerebral vein and sinus thrombosis, especially in OCP users, so that clinical information regarding its presentation, course and outcome are limited. Due to variable clinical presentations of CDVT, its diagnosis is often difficult; therefore, heparin treatment has been established with substantial delay, which is generally accompanied with poor prognosis (3, 4). Occlusion of the Galen vein and internal cerebral veins is the least common and most clinically obscurities of venous syndromes. From the few studied cases, a picture of bi-thalamic infarction emerged, which was sometimes reversible, mainly consisting inattention, spatial neglect, amnesia and akinetic mutism, as well as apathy. Other cases manifested coma and pupillary changes, referable to ischemic diencephalon and rostral midbrain. Therefore, clinical demonstrations of CDVT can be nonspecific and can cover the changes in mental status, alter consciousness, and even lead to coma (5, 6).
Thrombosis of Galen vein is a rather fatal event, resulting in venous hypertension, infarction, and hemorrhage, than a slow and easy-going clinical course. Patients get referred to a neurologist after interventions and different care modalities. Even though partial flow disturbance in the course of Galen vein has somehow contributed to the course of the disease, perhaps, it has not been the main causative element (7-9). Changes shown by the white arrows in the magnetic resonance venography (MRV) (Figure 2) could also be due to a stenosis, duplication, or fenestration rather than thrombus formation; but, response to the treatment highlighted the possibility of thrombosis.
Imaging-based diagnosis of CDVT is usually problematic due to the absence of characteristic delta sign of superior sagittal sinus thrombosis on contrast enhanced CT scan. Furthermore, normal variability of flow-related signals in straight sinus on MRI leads to seduction. However, deep veins hyperdense thrombus on CT scan can be suggestive for the diagnosis and MRI and MRV can serve as confirmatory tools, by showing hyperintense lesion on T2-weighted and hypointense ones on T1-weighted images that related to ischemia and vasogenic edema, induced by CDVT (10-13). The intraluminal clot clearly appeared as an area of hyperintensity on T1 weighted images and the absence of flow signal in MRV (14). Heparin has been accepted as the cornerstone of treatment in primary encounter and invasive procedures such as endovascular thrombolysis; in more severe cases, decompressive hemicraniectomy is left for nonresponsive cases. Accompanied neurological complications such as seizures and intracranial hypertension require specific treatments (12, 15).
CDVT with numerous clinical features is usually associated with diagnostic difficulty. We described a case of Galen vein thrombosis to emphasize the importance of different manifestations of deep vein thrombosis which can lead to delay in appropriate treatment due to misdiagnosis.